How to maximize accuracy and streamline orthognathic surgery with virtual surgical planning
BY DR DANIEL BUCHBINDER

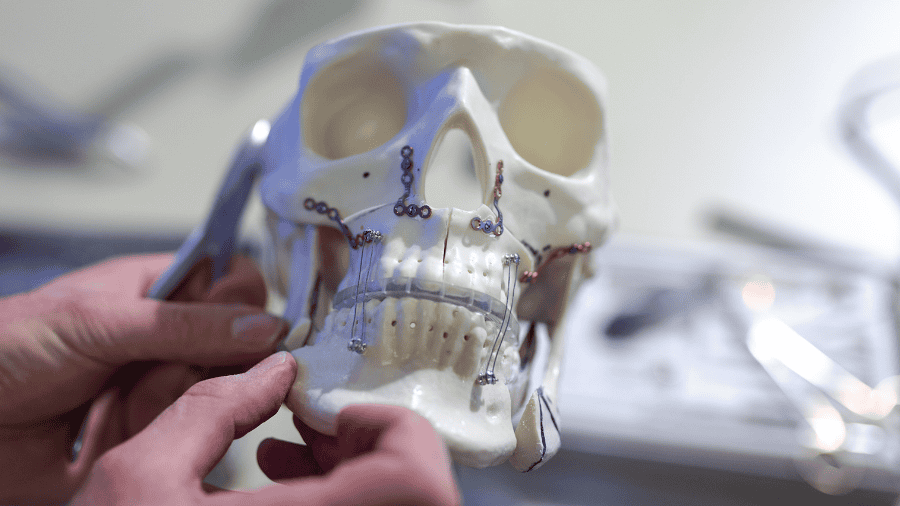
For decades, model surgery was the mainstay in treatment planning—and everybody had burns from the hot wax used to create models! Yet the accurate 3D repositioning of the maxilla remained difficult. Computer-assisted planning tools reduced the use of model surgery, and today, most surgeons use a combination of computer-assisted planning and patient-specific plates. The use of 3D patient-specific plates and cutting guides are a logical solution to transfer the surgical plan to the operating room.
The digital workflow looks something like this: You start off with the clinical evaluation, followed by cephalometric analysis, you take articulated casts to generate 3D models, and you perform the model surgery. From there you generate the CAD/CAM splint fabrication and go into the surgery. The splints are the main way you take your plan into surgery.
We had an idea to change the workflow, so we'd no longer need articulated casts or split fabrication once we used 3D printed plates. One of the main ways we got there was by using optical scanners to fuse the models or CT data together with the optical scan, to create very precise 3D models. We used the 3Shape intra-oral scanner to capture hundreds, if not thousands, of images of the dentition, then overlay that to the DICOM files from your CBCT or CT scanner.
This enables us to produce precise virtual models, then to manage the occlusion or do the model surgery where you can actually set the occlusion completely digitally, without having to send any physical models to the company. By doing that, you get these occlusal maps, which tell you the areas of contact or collision, so you can establish the bite and make sure you have everything you need to set the occlusion virtually.
Pros and cons of virtual planning and 3D printed plates
The method transforms the workflow so that you no longer need the physical casts, and you perform the model surgery entirely virtually. You design and fabricate the surgical guides and patient-specific plates, and then go on to surgery, which really streamlines the workflow.
Considering the workflow in more detail, you can take the DICOM data and use it to create 3D virtual models, which are fused with the optical scans. Once you do that, you perform the virtual osteotomies. The occlusion could be set virtually or by optical scans. With that in place, you can design patient-specific plates, so the bony segments are moved to their final position.
You can predetermine the location of your screws, then working from your plate design, go back and reposition the bone segments to the pre-op position. This allows you to create 3D printed titanium cutting guides. There are also cylinders there that let you know where to drill the predictive holes, allowing you to precisely position the maxilla or mandible. From there, you perform the osteotomies, drill the predictive holes, and attach the plates in the exact position you generated in your computer-assisted plan.
This is particularly good for patients with asymmetries, because it’s very difficult to control the pitch, roll and yaw of the maxilla unless you have 3D printed plates to take your plan to the OR.
So, what are the advantages and disadvantages of patient-specific cutting guides and 3D printed plates?
The advantages are accuracy, efficiency and safety, time saving, and overall cost-effectiveness. The cost measure takes account of the time it would have taken to do the planning, as well as the time saving in the operating room. But with this method we are not able to modify the plan intraoperatively, so once you have made the plan, there is no bailout. Then there’s the availability and accessibility of the technology, and the high cost in most countries, as well as the lead time for manufacturing.
Reaching sub-millimeter precision with virtual planning
Having taken you through the journey, I want to build an evidence base for the advantages of virtual planning and examine the scientific data.
A few years ago, we published one of our first studies on the accuracy of the 3D repositioning of the maxilla, which appeared in the Journal of Oral and Maxillofacial Surgery. In that paper, we looked at 10 cases and examined accuracy in the x, y, and zed axis. All patients were over 18, no revision cases, and all underwent bimaxillary orthognathic surgery. We used computer-assisted planning and PSP for all cases, so it wasn’t really randomized. In the postoperative analysis we looked at some cephalometric landmarks, and we tried to overlay these to judge how they compared with our plan. We used the x-axis, right-left direction, the y-axis, AP direction, and the zed-axis, which was a superior-inferior direction.
The sample size was equally male and female, we had class twos as well as class threes, and most were single-piece Lefort osteotomies. One was a three-piece osteotomy, and that's where we had the largest discrepancy, in terms of results. When we did the analysis, everything was sub-millimeter, and most of the movements were even within half a millimeter discrepancy between the plan and the postoperative result. The conclusion from that study was that, on average, we had a high level of accuracy and precision using virtual surgical planning. The idea was to look at other studies to see what else was out there.
The next study of interest is a meta-analysis of all the articles on computer-assisted studies and the use of patient-specific plates. This systematic review reached a promising conclusion, with the studies showing that the waferless osteotomy procedure I pursued has produced accurate postoperative results. The study authors determined that further long term follow up is required, as well as additional studies directly comparing the waferless osteotomies to the traditional method, which utilizes a surgical wafer.
Ed Ellis and his group did a study just like that last year in our journal. Their conclusion was that the use of patient-specific plates provides a more accurate maxillary positioning during bimaxillary surgery than the use of the interim splint. So again, there is more evidence that patient-specific plates and computer-assisted surgery are more accurate than traditional means.
Lastly, in terms of cost-effectiveness, very few studies have really looked at it, because there are so many variables. However, James Xia from Houston, Texas, did a study a few years ago that showed a significant cost reduction if you took account of not only the actual surgical event, but also how long it takes to do the planning by hand, how much longer the surgery takes, the OR time, et cetera. He was able to show, even as early as 2006, that there was a lot of merit to computer-assisted planning, and now even using patient-specific orthognathic internal fixation devices.
Watch the video:
Virtual Surgical Planning with Daniel Buchbinder, Rafael Cypriano, Belinda Beltrán, Juan Carlos Orellana (Global Study Club, 2023).
Survey reveals widespread use of computer-assisted surgery
With that in mind, a global survey we carried out on behalf of the AO CMF looked at the world trends in terms of what's happening with patient-specific plates and computer-assisted surgery. The primary objective was to analyze the current performance of the technology, and we sent the survey to CMF surgeons who perform orthognathic procedures using computer-assisted planning. The result was a comprehensive, adaptive survey that took you down a path, depending on your responses, because we wanted to look at different trends. The vast majority of responses came from CMF surgeons, cranial maxillofacial, or oral maxillofacial surgeons. Interestingly, there was a bimodal distribution by experience. A lot of very experienced surgeons were using it probably for efficiency, and younger surgeons who were using it more for the reason of accuracy.
Here is a snapshot of the survey results:
- Orthognathic surgeries: most respondents were doing less than 25 and they were using computer-assisted planning as well as patient-specific plates. The majority of respondents were doing between 25 and 50 cases a year.
- Region: 68.2% of respondents in Latin America used computer-assisted planning. It was also very popular in Europe and North America, where the cost is bundled into the hospital cost.
- Experience: Most respondents used the technology regardless of their level of experience with it.
- Frequency: 66% of respondents planned to use computer-assisted planning in fewer than 25 cases a year. Only 1% were doing more than 100. 72% of people said they used it in less than 25% of cases, and I don’t blame them because this really should only be used in complex cases.
- Cutting guides: In terms of patient-specific cutting guides and plates, those that are in training used these the most. However, almost 60% of people with more than 15 years' experience also used them.
- In-house or web-based planning: Most people in North America use web-based planning. In Europe and academic centers, some of the people use in-house planning. This type of planning takes between one hour to two hours.
- Maxilla or mandible: Roughly half of people used it for both, and half used it for the maxilla only, because once you have it set in 3D, the mandible just must follow with the occlusion.
- Lead time: A lot of people said it was too long, and the optimal time should be less than one week. Only 7% said it modified their preoperative planning.
- Maxillary splint: Most surgeons still used an interim splint when performing bi-maxillary cases, which I think is a belt and suspenders thing.
- Postoperative imaging: Unsurprisingly, most people take images, though I was surprised to see that the lowest was people in training.
- Accuracy: Most people felt that computer-assisted surgery and patient-specific plates really did the job.
- Time reduction: 131 respondents reported reduced operating time, and the majority said that it was about 16-50% less than when you were not using computer-assisted, the cutting guides, as well as the patient-specific plates.
In summary, most people were using computer-assisted planning and patient-specific plates for accuracy. 196 out of 253 (77%) were doing it for efficiency. Ease of pre-operative planning was a motivation for 60% of people, and overall cost benefit for 16%.
The take home message is that computer-assisted planning, cutting guides, 3D printed plates and patient-specific plates, are a very effective way to address complex 3D corrections of skeletal facial deformities.
About the author:
You might also be interested in:
AO CMF and virtual surgical planning
Find upcoming courses, recorded webinars and expert presentations, and AO CMF assets on virtual planning.
AO CMF Global Study Club
A reliable and dynamic platform where AO CMF members get together to discuss compelling cases.
Join the network!
The dynamic and universal spirit of the AO CMF community transcends borders and specialties, benefiting both patients and healthcare providers across the globe.
Further resources on orthognathic surgery
Explore AO CMF’s resources on craniomaxillofacial orthognathic surgery.