Simplicity derived from complexity: the development of the new variable angle clavicle fixation system based on digital modeling of anatomy and pathoanatomy
Abstract
Nonoperative management has been the common standard of care for shaft and distal fractures of the clavicle. Randomize-controlled trials suggest that functional outcomes improve and return to work is faster with operative treatment. Current internal fixations systems, with poor fit to the anatomical variability of the clavicle and excessive subcutaneous prominence, hinder the acceptance of operative approaches. A series of studies investigating the implant-preferred pathway and principle component analysis revealed the "rules" to be considered for a new clavicle internal fixation system. The new system considers the subdivision of the clavicle into fifths and each segment has particular anatomical features that will influence the shape of the plate. Variable angle technology was introduced impacting screw size and screw hole pattern.
The changing concepts of clavicle fracture management
Nonoperative management has been the common standard of care for shaft and distal fractures of the clavicle. When it occurs, nonunion after nonoperative treatment has been considered to be benign. Little attention has been paid to neural and vascular symptoms of retroclavicular space compression or distortion presenting as thoracic outlet syndrome after malunion, yet these symptoms may be more common than previously diagnosed. This is the subject of a current application for a research project within the AO Research Institute Davos (ARI). Understanding the functional disability consequent on fixed scapular displacement after malunion of the clavicle (nearly always in ventral rotation with anterior, inferior, and medial displacement of the lateral fragment) has been hindered by the difficulty of characterizing the position and motion of the scapula in clinical and laboratory practice. This is compounded by taking radiographs of the injured clavicle in only the frontal plane and excluding the scapula with no comparator views of the opposite clavicle and scapula.
The fracture displacement is commonly described as displacement of the medial fragment since this is apparently displaced superiorly in relation to the lateral fragment. This is not the case, as it is the lateral fragment (therefore also the scapula) that displaces away from the medial fragment. Since the center of rotation of the shoulder joint is determined by the position of the scapula, a clavicle fracture will always have a consequence for shoulder joint motion. The amount of consequential shoulder and shoulder girdle dysfunction is variable and may be accommodated by the wide range of motion of the shoulder joint, so that it becomes difficult to evaluate and difficult to measure or categorize accurately when using current scoring systems to justify and to compare between treatments.
Clearly patients with nonoperative management of displaced clavicle fractures take longer to return to work, have more pain, and achieve poorer functional outcomes than those who undergo operative fixation of similar fractures. Scapular postural disturbance and altered patterns of scapular motion result from the common inferior, anterior, medial, and rotational displacement of the lateral fragment. Recent randomized-controlled trials of operative versus nonoperative management of displaced clavicle shaft fractures have convincingly shown that functional outcomes and the interval to return to work are favored by operative fixation. The incidence of malunion and nonunion are both reduced by internal fixation. However, excessive subcutaneous prominence of current plate systems, and dissatisfaction with the intraoperative ‘fit’ of the plate systems in common use mitigated against a generally accepted operative approach. Recent detailed cost analyzes of clavicle fracture fixation suggested that it may be possible during the early phase of follow-up to predict which fractures will not eventually heal and/or have a good functional outcome. Those fractures were considered for delayed operative intervention achieving good rates of union. This strategy was pragmatic and cost-efficient since fewer fractures were fixed than might have otherwise been the case had all displaced fractures been fixed in the first place. The overall reoperation rate including removal of prominent plates was reduced. It is hoped with the advent of quick, low-risk CT scanning with 3D reconstructions which include the scapulae that the evaluation, prediction, and risk stratification of functional outcomes will be facilitated.
Although the rates of infection, nonunion and malunion among surgically treated clavicular fractures are low (< 4.2%), the rate of surgical device removal or revision was reported to be high (83%) in a retrospective database analysis in the US [1]. The associated costs for the healthcare system are considerable and improved surgical options to reduce the rate of unplanned reoperations are necessary.
Motivation for changing clavicle fracture internal fixation system
The poor fit of current clavicle internal fixation systems originates in the combination of implant design and anatomical variability of the clavicle.
- Implants are mainly designed for fractures of the middle third of the clavicle and have a shape that matches the clavicle anatomy in this region. Robinson [2] showed that clavicles are better described as having subdivisions into fifths, i.e., five segments starting from the lateral end. Most diaphyseal fractures occur between the second and third fifths, for which a middle third plate is inappropriate. Compromising between plate fit and plate position with respect to the fracture could lead to imbalanced fixation, and failure of fixation. Describing a fracture as the ‘middle third’ according to a frontal radiograph leads to incomplete diagnosis and inaccurate treatment.
- The complex topographical anatomy of the clavicle challenges the definition of an internal fixation system which accommodates all variants of surface shape, dimension, and form.
- The surgical goal to avoid further fracture-related soft tissue damage in order to avoid further periosteal injury and consequent risk of failure of periosteal perfusion leading to delayed union.
An ARI research project [3] investigated the implant-preferred pathway (IPP) on the clavicle through 3D computational modeling of its shape. The IPP represents a continuous linear region of interest where the least possible soft-tissue disruption is necessary for plate fixation. Vectors created perpendicular to the tangent of the IPP define the ‘twist’ of the bone. This feature had not been designed into existing implants accurately for most fracture locations. The twist was a constant 35° independent of length and bowing of the clavicle. Furthermore, the radii of the antecurve and retrocurve segments had different consequences for clavicle morphology. The radius of curvature of the IPP in the retrocurve segment (the most lateral two fifths) was invariant between clavicles of different length and gender. Principle component (PC) analysis showed that clavicular length is the primary determinant of clavicular shape: the radius of curvature of the medial antecurve segment, the medial three fifths of the bone, was directly related to length. Further PC analyses determined that the clavicle shape obeyed ‘rules’ that were simple if a single IPP was considered.
A group of internal fixators might be designed based on these underlying ‘rules’ of the IPP concept. The length of an internal fixator which determined the arc of curvature medially could be predicted from the patient’s other clavicle or from his/her height and span, since these were also correlated to the clavicle length.
Market opinions
Hardware prominence and related pain, and reoperation for hardware removal are common concerns with clavicle osteosyntheses, so the focus was on better fitting, lower profile implants for various clavicle fractures, including lateral fractures with associated acromioclavicular joint dislocations in which a hook plate is indicated. Although minimally invasive percutaneous bridging osteosynthesis is acceptable for many anatomical regions, including the clavicle, a full spanning internal fixator is questionable for most surgeons. The absolute need for clavicular hook plate removal because of acromial lysis and subacromial bursal disease is a major barrier to its general use. Better design characteristics for a clavicular hook plate were required because of the high-complication rate noted in the literature and through personal experience.
Evolution of the design features of the next generation internal fixator for clavicle fractures
Since a plate has a footprint and the IPP is a line, the IPP cannot fully describe the shape of a novel plate for the clavicle. The lateral fifth is a relatively flat bone segment for the attachment of muscles on its superior surface and the suspensory ligaments on its inferior surface. This lateral fifth morphs into a cylindrical bone at the transition region between the second and third fifths of the clavicle with constant twist (see above ). The novel plate shape had to respect this surface topography, which is considered complex. The recognition of ‘rules’ underlying the IPP triggered the question of the existence of similar ‘rules’ for the shape of a plate.
At the same time, variable angle (VA) technology was introduced into many systems for internal fixation, and screw design evolved to accommodate the qualitative and biomechanical differences between cortical and metaphyseal bone. These available technological advancements allowed for a broader reconsideration of the next generation internal fixator, in terms of screw sizes and screw hole pattern. The standard 3.5 mm screw fixation systems were too stiff for the caliber of some clavicles, and an investigation was initiated into the validity of a 2.7 mm screw-based system for the clavicle. Recognizing that the introduction of a 2.7 mm rather than a 3.5 mm screw system would raise questions about the strength of the fixation, considerations of required screw density and clustering, as determined by fracture patterns, were also initiated. A better understanding of specific patterns and locations of the clavicle fractures and their frequency was identified as a requirement to determine the optimal range of plate lengths, allowing for a ‘balanced’ fixation with a 2.7 mm system.
To answer all these questions a ‘back-to-basics’ approach was required: opinion was sought and expertise valued but not relied on. The topics identified for basic and applied scientific evaluation included: the specific regional anatomy of the intact bone and its variants, epidemiological studies of actual fracture patterns and frequency, biomechanical behavior of various options for the internal fixation systems, and likely behavior of fracture after fixation with respect to the risk of complications. To enable these themes to produce useful material for the design process, computational modeling, virtual design development, predicate and evolved plate biomechanical testing, fracture and fixation simulations were all undertaken, with dry and wet laboratory testing of several iterations of the prototype fixators. Market research and usability testing in laboratory programs were initiated and valued with expert opinions from UEEG and surgeons not affiliated with UEEG. This package of evidence generation and continuous ‘sense-checking’ was unique to the process of development of a novel internal fixation system.
An analysis of computed tomographic scans of intact clavicles from a broad patient population investigated the underlying ‘rules’ of the clavicle shape by correlating the relevant anatomical parameters with individual patients’ metadata, such as height or ethnicity [4]. Although many studies analyzed clavicle parameters, such as length or curvature, the relationship between the morphometric parameters and patients’ demographics was partially described in the literature. The results showed that there is a strong correlation between the patients’ height and clavicle length, as well as between the clavicle length and specific shape parameters, such as curvature radii. This means that the shape of the clavicle is ruled by its length and ultimately by the stature of the patient. Smaller patients have shorter and more curved clavicles, whereas taller patients have longer and less curved clavicles. The novel internal fixator system was developed based on this predictable relationship between length and shape.
Different elements of the research were addressed by different groupings of the members of the Upper Extremity Expert Group (UEEG) with colleagues in the ARI, members’ university establishments, and DePuy Synthes (DPS) development and design engineers and marketing departments. The results were discussed, assessed, and analyzed within the UEEG in partnership with our colleagues from DPS in a collaborative effort. The consistent collaboration of the core group was instrumental in the continuing progress of the project through phases of organizational changes.
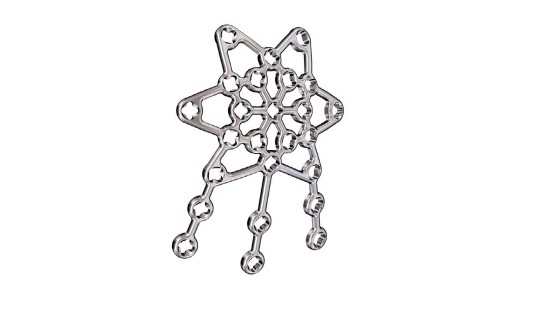
Evolution of the design features of the next generation internal fixator for the distal clavicle fractures, distal clavicular fracture-dislocation, or equivalent acromioclavicular separations
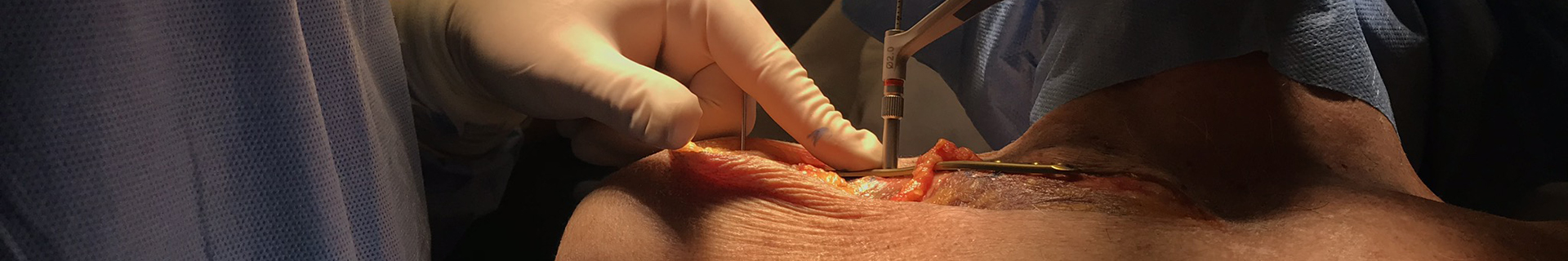
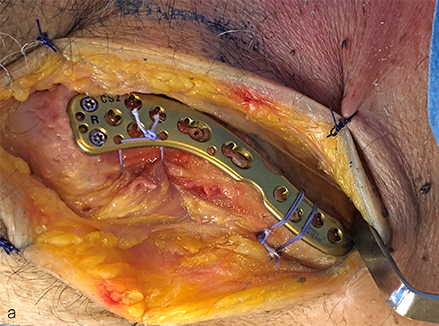
Distal clavicular fractures are characterized by splitting of fragile bone in a horizontal plane as well as vertically, with fragments which are often closely associated through the soft tissues around the fracture zone. Fixation of these fractures requires complex and variable orientation of fixation in the weaker distal bone and optimal balanced fixation in the stronger diaphyseal bone while respecting the trapezius, deltoid, and pectoral muscle attachments and permitting repair and reconstruction of coracoclavicular ligaments where required. Low-profile fixators are tolerated better, screw head prominence should be avoided, and fixation in the shaft should not compromise fixation in the distal clavicle, and vice versa. A prototype fixator used in a user-evaluation laboratory is shown in Figure 1.
It has long been recognized in clinical practice that use of the clavicular hook plate for a range of distal clavicular injuries was complicated by inadequate understanding of the topographical anatomy of the deep surface of the acromion. This mismatch leads to small regions or points with high-compressive loading by the tip of the hook on the deep surface of the acromion, in bone which under normal conditions is subject largely to tension, and therefore has thin cortices. This localized loading of the hook resulted in frequent acromial pain, acromial osteolysis, and occasional acromial fracture. Subacromial bursitis and superior surface rotator cuff damage was also recorded.
These complications mandated a redesign of the hook plate system in conjunction with the novel internal fixation system considered for the clavicle shaft fractures. Little was known about the acromial surface morphology and how this related to the position and other design attributes of the hook plates (depth, length, orientation in all planes, tip design etc).
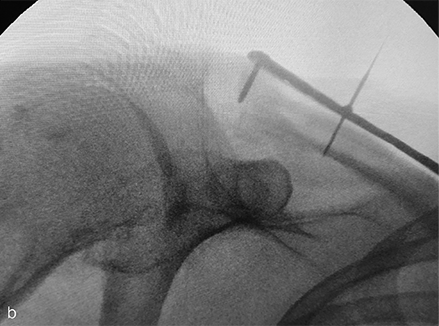
Figure 1a–c Distal clavicular fixation during prototype evaluation of the novel VA Clavicle System. Lateral is to the left in all figures. Conformation of the plate to the superior topography of the distal clavicle is designed to facilitate positioning of the distal margin of the plate parallel to the acromioclavicular joint (a) and respects the almost universal 12o downward tilt of the distal clavicle in the lateral fifth of the bone (b), while also allowing the plate to follow the beginning of the twist region at the junction of the second and third fifths of the bone (c).
A separate research project based on 3D imaging of the acromion and distal clavicle was initiated (Martin Zenker et al, unpublished data). This aimed to describe the variation in morphology of the deep surface of the acromion with respect to the distal end of the clavicle, and to relate this to the optimal size and shape for the entire hook, not just the tip as a neutralization device for the realignment of the distal clavicle with respect to the acromion. The study concluded that there exists a high inter-patient variability of the deep acromion morphology. However, it was possible to identify a sweet spot, where this variability is minimized. Hook plates should aim at this spot to best reduce the risk of pin-point contact, sub-acromial undercut and impingement. With these insights, hook plates with optimized hook inclination, torsional angle, depth, and length were developed within the novel internal fixator system.
Discussion
The continuous collaboration between UEEG members and DPS project team members focusing on clinical unsolved needs, advanced morphological investigations, prototype usability and reassessment of fixation technologies was the key for succeeding in developing a new internal fixator system for the clavicle. This new system was developed on the foundation of an extensive analysis of clavicular and shoulder computed tomographic scans, where plate shapes were designed and optimized based on the underlying rules and correlations of the clavicle anatomy. The optimized plate shape with the implementation of a low profile, smaller screw diameter, and VA technology in the system allow the surgeon to achieve a balanced fixation of a wide variety of clavicle fractures while ensuring optimal fit and reduced plate prominence.
Acknowledgment
Simon Lambert contributed to this article on behalf of the former AO Technical Commission UEEG, and Arabella Fontana and Martin Zenker belong to the DPS project team.
The former AO Technical Commission UEEG, now part of the Upper Extremity Global Expert Committee, comprised Stefaan Nijs, Martin Jaeger, Chunyan Jiang, Harry Hoyen, and Simon Lambert. The DPS project team comprised (at different periods in the development pathway) André Galm, Arabella Fontana, Martin Zenker, Daniel Andermatt, Paul Franer, Regan Barber, Martin Bammerlin, Manish Gupta, and Thomas Doerdelmann.
References
1. Putnam, M, Vanderkarr M, Nandwani P, et al. Surgical treatment, complications, and reimbursement among patients with clavicle fracture and acromioclavicular dislocations: a US retrospective claims database analysis. J Med Econ. 2019 Sep;22(9):901–908.
2. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998 May;80(3): 476–484.
3. Lambert S, Al-Hadithy N, Sewell M, et al. Computerized tomography based 3D modeling of the clavicle. J Orthop Res. 2016 Jul;34(7):1216–1223.
4. Fontana AD, Hoyen HA, Blauth M, et al. The variance of clavicular surface morphology is predictable: an analysis of dependent and independent metadata variables. J Shoulder Elbow Surg Int. 2020 Jun 19;4(3):413– 421.
5. Zenker M, Galm A, Hoyen H, et al. 3D Morphometric Analysis of the Acromion and Distal Clavicle at the AC Joint – Implications for Surgical Treatment Using Subacromioal Support rather than Claviculocoracoid Suspension (in preparation).
You might also be interested in
Cannulated Screw System CSS+
Improving cutting performance and facilitating accurate screw insertion.
VA-LCP Clavicle Systems
The next generation of internal fixation for the clavicle and a solution for fractures and injuries.
The new Variable Angle Locking Patella Plating System
The Variable Angle Locking Patella Plating System was developed to reduce complication rates.
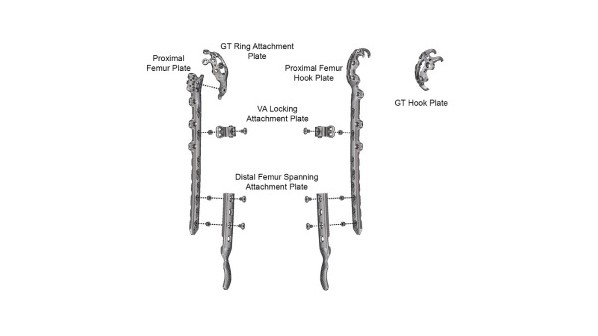
The new Variable Angle LCP Periprosthetic Proximal Femur Plating System
Developed to address various aspects in periprosthetic femoral fracture treatment.
Disclaimer:
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
The brands and labels "approved by AO Technical Commission" and "approved by AO Foundation", particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.