Peri-implant fractures in short versus long cephalomedullary nails following pertrochanteric fracture consolidation
Introduction
Pertrochanteric femoral fracture fixation with the use of cephalomedullary nails (CMNs) has become increasingly popular in the recent past. Known complications after fracture consolidation include peri-implant fractures following the use of both short and long nails, with fracture lines around the tip of the nail or through the interlocking screw holes, resulting in secondary midshaft or supracondylar femoral fractures, respectively. Limited research exists to help the surgeon deciding on the use of short versus long nails, though both have their benefits.
This project aimed to investigate one of the newest generations of short and long CMNs in a human anatomical model, in terms of construct stability and generation of secondary fracture pattern following pertrochanteric fracture consolidation.
Materials and Methods
Sixteen paired human anatomical femora from eight donors (five women and three men) aged 83.4 ± 7.7 years (range, 74–95 years) were assigned to two groups of eight specimens each for nailing with short or long CMNs. The newest generation CMNs of the series Trochanteric Fixation Nail Advanced (TFNA) of 10 mm diameter and 130° neck-shaft angle were used with reaming of the intramedullary canal to a diameter of 11 mm before insertion of the long nail. Based on a multi-ethnic computational analysis, this generation features an improved nail shape with 1.0 m radius of curvature designed to better fit the patient's anatomical bow and enhance implantation. The length of the short nails was 170 mm, whereas the length of the long ones was chosen distally to the metaphyseal flare. Helical blades were used as head elements, ensuring an appropriate tip-to-apex distance of less than 20 mm. The short nails received one distal interlocking screw in the static position, and the long nails also received one distal interlocking screw in the most proximal static hole. The implantation was performed without a fracture to simulate a peri-implant fracture in a united femur.
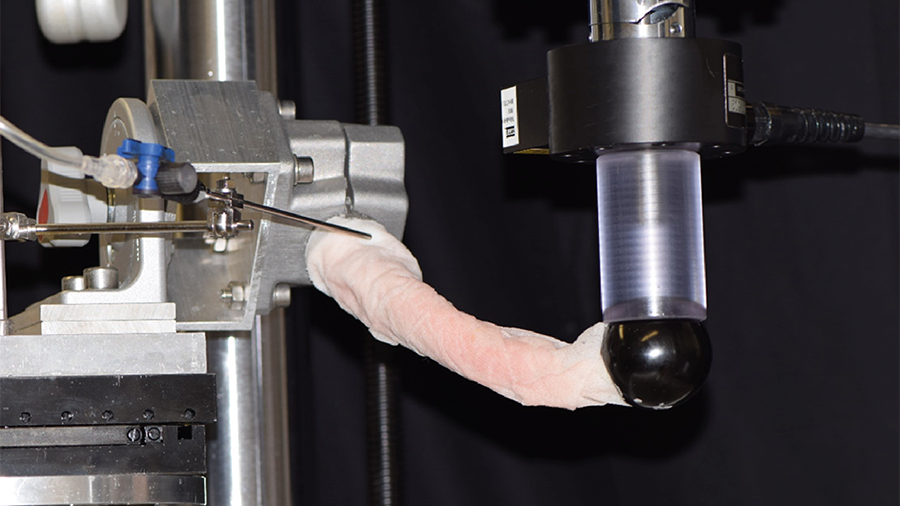
Each specimen was first biomechanically preloaded at 1 Hz over 2000 cycles in superimposed synchronous axial compression to 1800 N and internal rotation to 11.5 Nm (Fig 1). Next, internal rotation to failure was applied over an arc of 90° within 1 second under 700 N axial load. Torsional stiffness as well as torque, angle, and energy at failure were evaluated. Digital image correlation analysis was performed by means of stereographic optical measurements using a contactless full-field deformation technology to calculate the strain at the fracture site. Fracture patterns were analyzed.
Results
Outcomes in the groups with short and long TFNA were 9.7 ± 2.4 Nm/° and 10.2 ± 2.9 Nm/° for torsional stiffness, 119.8 ± 37.2 Nm and 128 ± 46.7 Nm for torque at failure, 13.5 ± 3.5° and 13.4 ± 2.6° for angle at failure, and 887.5 ± 416.9 Nm° and 928.3 ± 461.0 Nm° for energy to failure, respectively, with no significant differences between them (P ≥ .17).
Minimum major strain at the fracture site measured immediately before initiation of the fracture line was 0.327 ± 0.114% for short and 0.262 ± 0.081% for long nails, with no significant difference between them (P =.32).
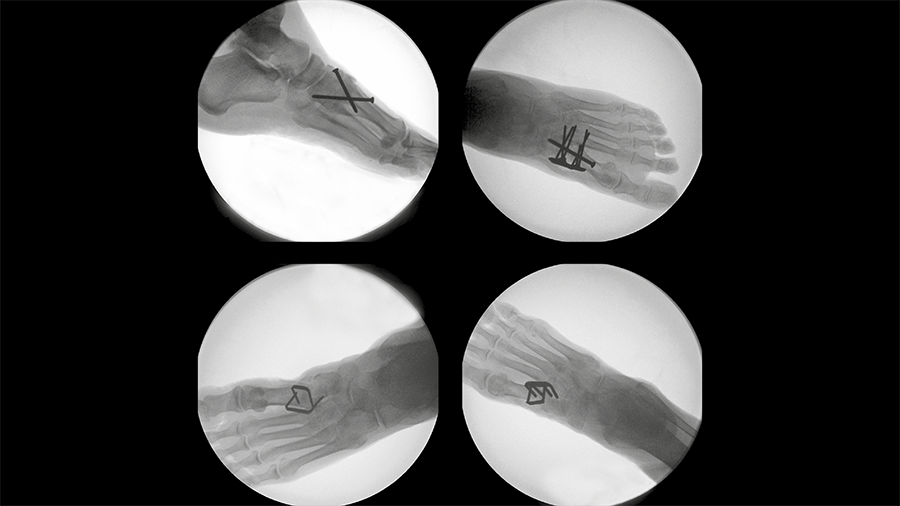
The group with short nails had a fracture through the head element in three specimens, all of which appeared to have a spiral fracture line in continuity with the distal interlocking screw hole (Fig 2). Two additional specimens in this group had a fracture through only the distal interlocking screw hole. Moreover, three femora with short nails had a fracture through only the shaft, not involving the distal interlocking screw hole or head element. Two of the fractures were multifragmentary, both of which were only through the shaft.
In the group with long nails six specimens were fractured through the distal interlocking screw hole (Fig 2). Two femora were fractured at only the head element, with an additional specimen being fractured through the head element and distal interlocking screw hole. However, the latter did not have a fracture in continuity with the head element and distal interlocking screw hole in contrast to the group with short nails. Five multifragmentary fractures were observed, ie, four through the distal interlocking screw hole and one through only the head element.
Discussion
From a biomechanical perspective, the risk of secondary peri-implant fracture after intramedullary fixation of pertrochanteric fractures is similar when using short or long TFNA. Moreover, for both nail versions the fracture pattern does not unexceptionally involve the distal locking screw hole.
This investigation supports more recent clinical and biomechanical research on the peri-implant fracture risk in short and long CMNs. It seems reasonable that if a patient has a canal amenable to a well-fitting short nail, the quicker operation and less blood loss can make it the better procedure, especially for the sicker patient. Moreover, a revision of a secondary fracture around a long nail might be more demanding because of fracture lines being potentially closer to the knee joint.
You might also be interested in
Rib fracture plating comparison
Intrathoracic plate fixation demonstrates significantly higher stiffness versus extrathoracic plating.
Tarsometatarsal joint fusion
Nitinol stables might demonstrate comparable performance to established techniques for fusion of the first TMT joint.
Improving fixation stability with ASL
The novel TN-A delivers new approaches to treating unstable distal tibia fractures.
Combined nail and plate fixation
The treatment of osteoporotic comminuted distal femoral fractures shows a positive response to this new approach.