Intrathoracic versus extrathoracic rib fracture plating
Introduction
A considerable amount of data has emerged in the recent past demonstrating the benefits of surgical rib stabilization for treatment of multiple rib fractures, particularly incorporating a flail component. The AO Technical Commission Trauma approved in 2009 the MatrixRIB Fixation System to improve treatment outcomes. Self-drilling screws were added to the portfolio in 2019, complementing the existing self-tapping screws. Despite medical and scientific evidence indicating that successful implantation decreases complications, mortality, and length of hospitalization for surgical rib stabilization, the number of treated patients who could potentially benefit from this treatment is still small.
One of the barriers is related to challenges associated with the surgical procedure itself. Large incisions can increase the risk of infection and severe postoperative complications, raising concerns whether the treatment is more detrimental to the patient than the original trauma. Minimizing incision's size reduces infection risk; however, a large incision is often needed to treat multilevel fractures or address challenging locations, for example, within the subscapular region. Implants placed on the intrathoracic curve of the rib through small incisions from the contralateral side will reduce the risk of infection. However, construct stability following intrathoracic rather than extrathoracic plating has not yet been investigated. Therefore, the aims of this project were (1) to investigate the biomechanical performance of intrathoracic versus extrathoracic plate fixation in a human anatomical rib fracture model and (2) to compare the effect of rib plating with two versus three screws per fracture fragment. It was hypothesized that the fixation stability following intrathoracic plating—with the plate placed on the tension rib side—is superior; therefore, three bicortical screws may not be required per fracture fragment.
Materials and Methods
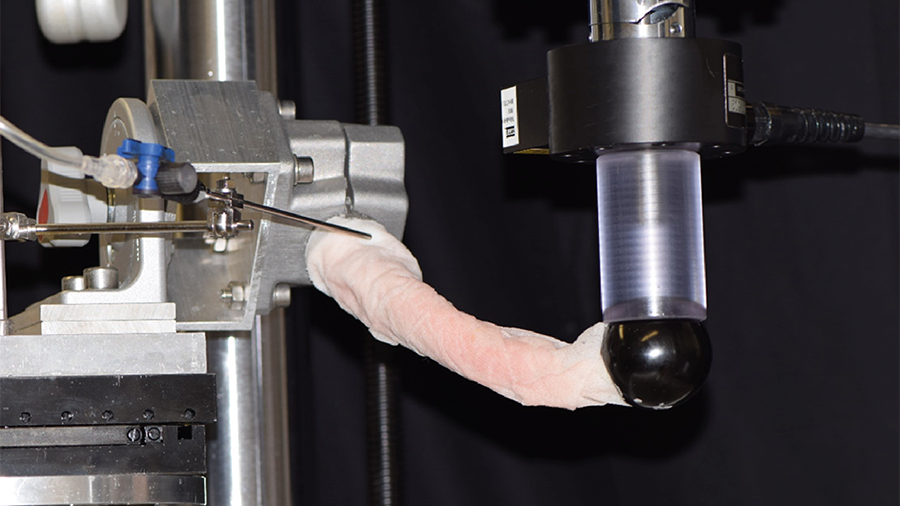
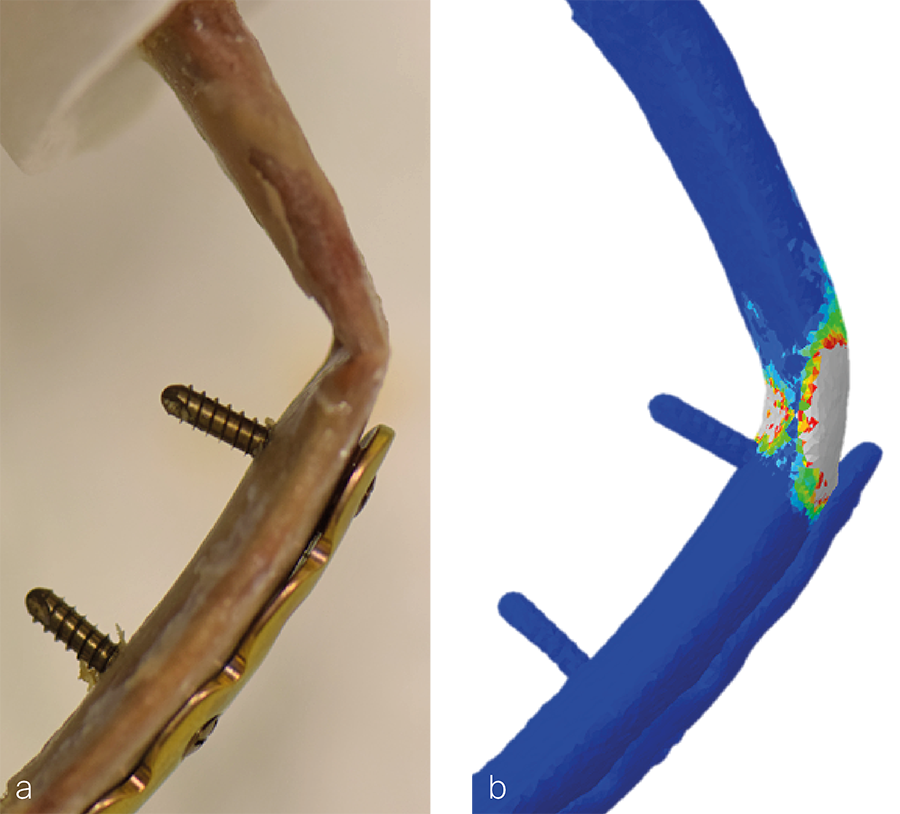
Twenty pairs of fresh-frozen human level-five ribs from elderly female donors (82.4 ± 7.8 years; range, 65–97 years) were assigned to four different groups of ten specimens each, splitting each pair for intrathoracic and extrathoracic plating with either two or three screws per fracture fragment. The specimens were fractured in a three-point bending test and fixed with an 8-hole titanium MatrixRIB universal plate with four or six self-tapping screws. First, all constructs were cyclically tested over 400,000 cycles applying a combined torsional and tensile-bending loading to replicate the physiological situation during respiration (Fig 1). Stiffness was evaluated every 100,000 cycles and overall construct subsidence was monitored. Second, a destructive quasi-static axial bending test was performed to assess the ultimate compression failure force. Test data was used to validate a finite element model predicting the failure location of plated ribs under axial compression bending (Fig 2).
Results
Stiffness of the intrathoracic plated specimens increased significantly compared with their intact state. In contrast, stiffness of the extrathoracic plated ribs decreased significantly versus intrathoracic. Plate positioning and number of screws did not demonstrate significant differences in construct subsidence or change in stiffness during cyclic and ultimate quasi-static testing.
Discussion
Intrathoracic plating of the rib allows for a minimally invasive approach; and, thus, may reduce risk of infection. Moreover, intrathoracic plate fixation demonstrates significantly higher stiffness versus extrathoracic plating, supporting its advantages as a fixation method. The number of screws does not seem to influence significantly construct stability regardless of the plate position, suggesting that two screws per fracture fragment can be sufficient to achieve stable fixation. In the clinical context, using fewer screws mean not only lower surgery costs but also shorter surgery time; therefore, reduction of the infection's risk.
You might also be interested in
You might also be interested in
Combined nail and plate fixation
The treatment of osteoporotic comminuted distal femoral fractures shows a positive response to this new approach.
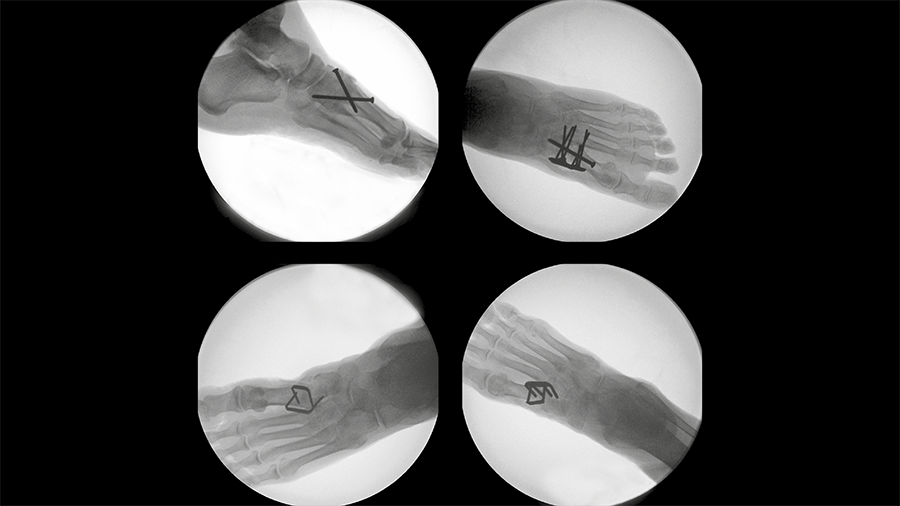
Tarsometatarsal joint fusion
Nitinol stables might demonstrate comparable performance to established techniques for fusion of the first TMT joint.
Peri-implant fractures
Short vs long cephalomedullary nails following pertrochanteric fracture consolidation.
Improving fixation stability with ASL
The novel TN-A delivers new approaches to treating unstable distal tibia fractures.