First tarsometatarsal joint fusion in foot
Introduction
Advanced deformities of the first tarsometatarsal (TMT-1) joint—being accompanied by a considerable increase in the first intermetatarsal angle—are often associated with relative hypermobility and instability of the joint. Arthrodesis is an established technique for management of such deformities and arthrosis of different origins.
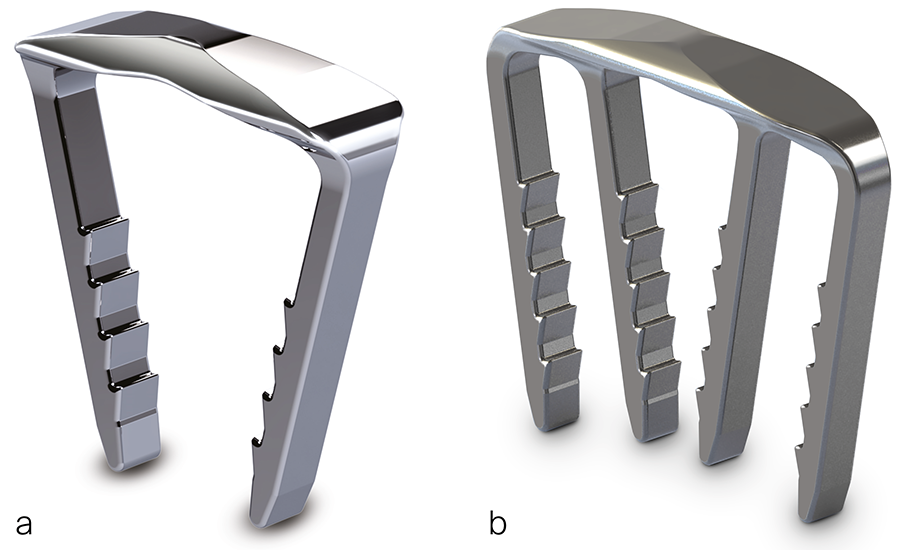
Currently, the standard TMT-1 arthrodesis technique is fixation with two crossed screws, having the disadvantage of necessitating 6–8 weeks immobilization in a short-leg cast and related to implant failure rates of up to 4.5% and nonunions in up to 15%. Use of locked plates as an alternative fixation technique could conceivably allow for earlier weight bearing and improve bony union; however, controversial findings are reported. On the other hand, the ability of low-profile superelastic shape-memory Nitinol staples to act as continuous compression implants (CCIs; Fig 1) by applying and maintaining a uniform active compression at the fusion site offers an attractive alternative to conventional screw and plate arthrodesis. Moreover, in contrast to screw fixation that occupies valuable area across the joint interface, CCIs could allow full joint coaptation by maximizing the footprint for fusion.
In 2018, AO TC Trauma provided product approval 'Recommended' for the following DePuy Synthes (DPS) BME CCI series for usage in the foot: SPEED™, SPEEDSHIFT™, SPEEDARC™, SPEEDTITAN™, SPEEDTRIAD™, and ELITE®. However, biomechanical and clinical research evaluating the use of CCIs for TMT-1 fusion is scant.
The aim of this project was to investigate under dynamic loading the potential biomechanical benefit of fusion with CCIs in two different configurations in comparison with screws and locked plating in a TMT-1 human anatomical model.
Materials and Methods
Thirty-two paired human anatomical lower legs were randomized to four groups:
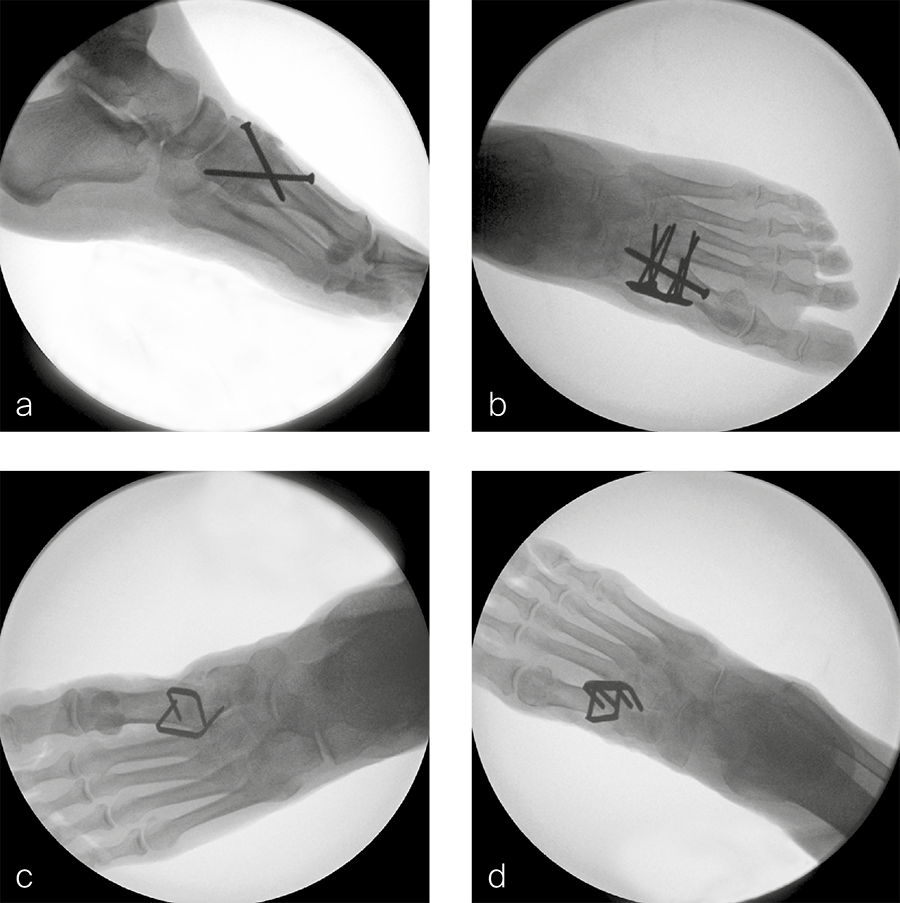
- Crossed-screw fusion with two DPS 4.0 mm fully threaded stainless steel lag screws inserted in standard fashion, ie, first screw from the first metatarsal to medial cuneiform and second screw from medial cuneiform to the plantar base of the first metatarsal (Fig 2a).
- Plate-and-screw fusion with a DPS 4.0 mm standard midfoot fully threaded stainless steel cortex screw, inserted cortically in lag fashion, and a DPS 6-hole TMT-1 stainless steel VA Fusion Plate 2.4/2.7 (Fig 2b).
- CCI fusion with 2 two-leg staples DPS SE-1818TI BME SPEEDTITAN™ and DPS SE-2520TI BME SPEEDTITAN™ placed orthogonally to each other (Fig 2c).
- CCI fusion with 1 two-leg staple DPS EL-1818S2 BME ELITE® and 1 four-leg staple DPS EL-2520S4 BME ELITE®, placed orthogonally to each other (Fig 2d). All fusion procedures were performed on intact feet with preparation of the joint articulations and under image intensification control according to the implant manufacturer's guidelines.
The lower legs were randomized to the four groups, with bone mineral density measured at the distal tibia being not significantly different between them (P = .92).
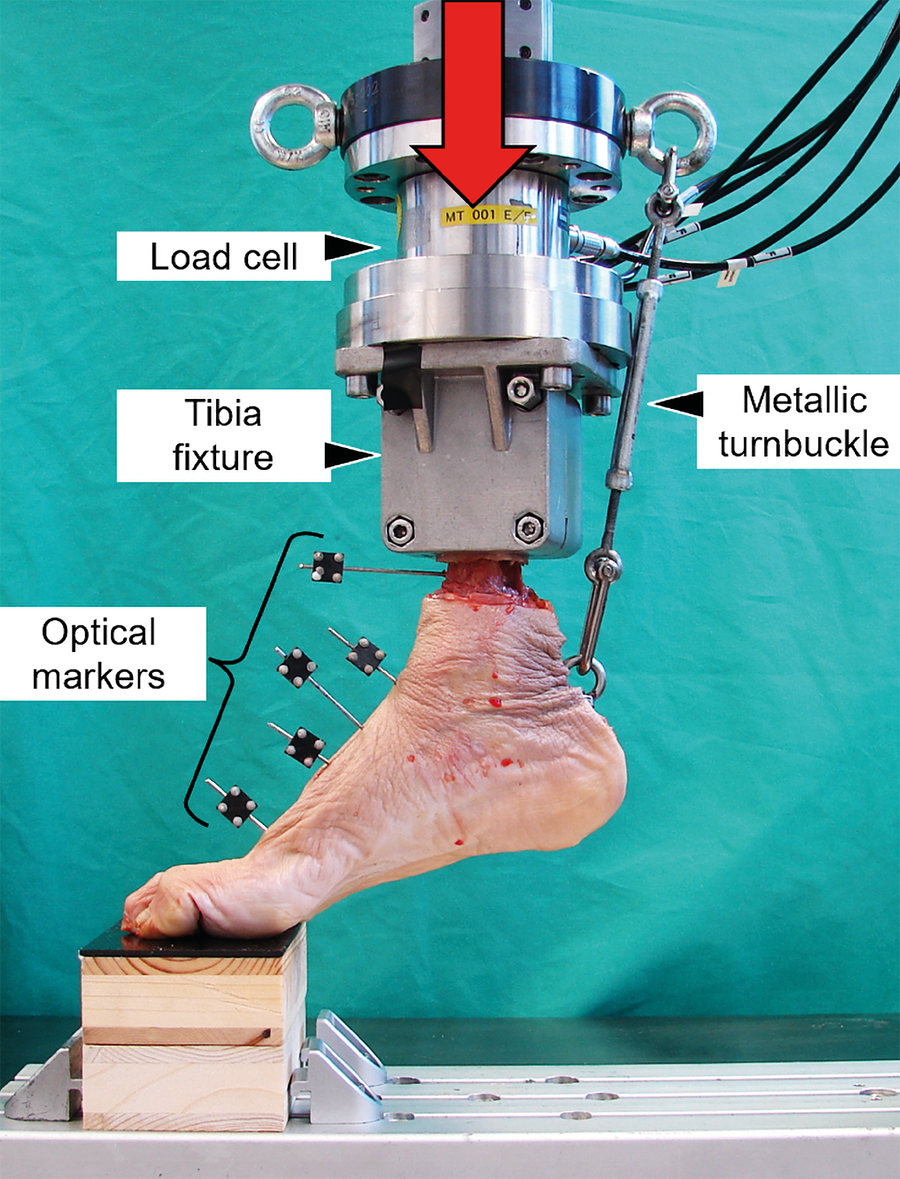
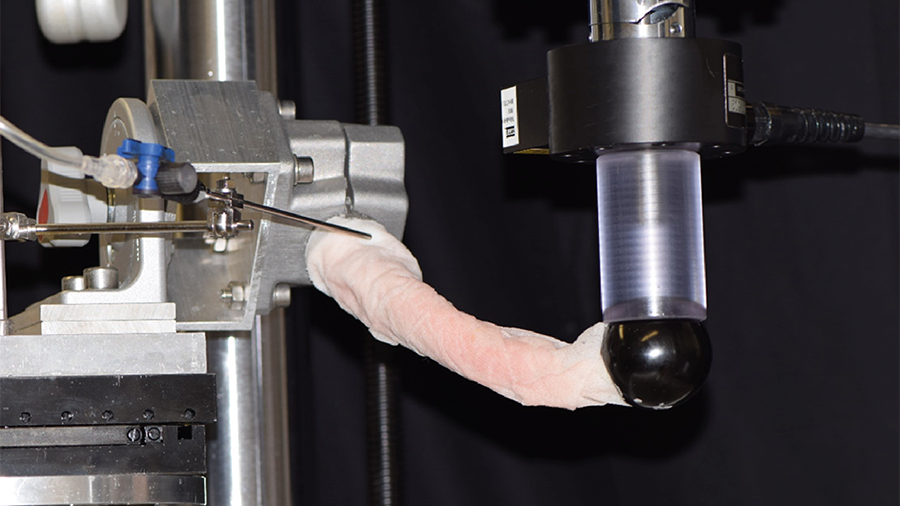
Each specimen was biomechanically tested using a setup simulating forefoot weight-bearing on the toes and the metatarsals (Fig 3). The testing was performed at 35–37°C under initial quasi-static axial ramped loading, followed by progressively increasing cyclic axial loading, and accompanied by triggered mediolateral radiographs and optical motion tracking, the latter capturing movements in the joints forming the medial column of the foot.
Results
The lower legs were randomized to the four groups, with bone mineral density measured at the distal tibia being not significantly different between them (P = .92).
Initial stiffness of the specimens did not differ significantly among the four fusion techniques (P = .87).
Combined adduction and dorsiflexion movement of the TMT-1 joint in unloaded foot condition increased significantly between 500 and 2500 cycles (P < .01); however, no significant differences were observed among all pairs of groups (P ≥ .13). In contrast, the amplitude of this movement between unloaded and loaded foot conditions within each cycle was significantly bigger for the two CCI fusion techniques compared with both crossed-screws and plate-and-screw techniques (P ≤ .04). No significant differences were detected between the two CCI fusion techniques, as well as between the crossed-screws and plate-and-screw techniques (P ≥ .49).
Displacements at the superior and inferior aspects of the TMT-1 joint in unloaded foot condition, together with their amplitudes between unloaded and loaded foot conditions within each cycle, increased significantly between 500 and 2500 cycles (P ≤ .04) but did not differ significantly among all pairs of groups (P ≥ .22).
Discussion
From a biomechanical perspective based on human anatomical specimen setting, the low-profile superelastic shape-memory Nitinol staples used as CCIs for more elastic stabilization under active compression might demonstrate comparable performance to established crossed-screws and plate-and-screw techniques for fusion of the first tarsometatarsal joint, which could allow full joint coaptation by maximizing the footprint for fusion.