Biomechanical benefit of combined nail and plate fixation for treatment of osteoporotic comminuted distal femoral fractures
Introduction
Osteosynthesis of native or periprosthetic comminuted distal femoral fractures using either a lateral locking plate or a retrograde intramedullary nail alone is considered to allow for early protected weight bearing only, especially in case of osteoporosis. Combining the two techniques may offer a stronger well-balanced fixation construct providing sufficient stability under full weight bearing. The rationale behind this implementation assumes a more balanced load sharing between bone and implants. Moreover, distal interlinking of the nail and plate could potentially result in even smoother transition of forces and moments and superior stability under immediate full weight bearing.
The project goals were to evaluate (1) the potential benefit of combined lateral plating and retrograde intramedullary nailing, and (2) the added primary stability via distal interlocking of the two implants with a single screw, in comminuted distal femoral fractures by means of finite element analysis, considering the nail fixation as baseline.
Materials and Methods
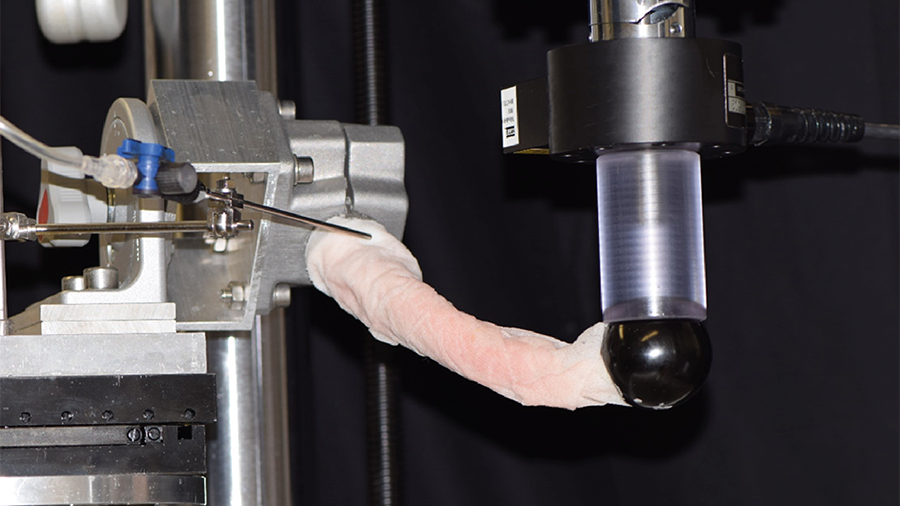
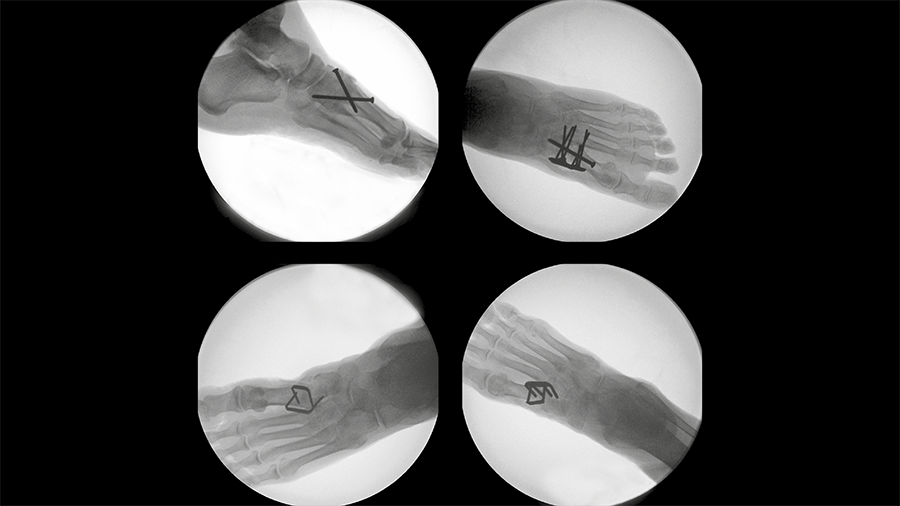
A finite element model was generated from the computed tomographic (CT) scan of a left intact osteoporotic distal femur from a 64-year-old woman donor weighing 57 kg. A transverse osteotomy with a 40 mm gap was cut 45 mm proximally to the distal end of the femur to mimic an AO/OTA 33-A33 fracture. A fixation with an 11 mm non-reamed retrograde intramedullary femoral nail (Expert R/AFN Retrograde/Antegrade Femoral Nail) and a proximally truncated lateral variable-angle (VA) condylar locking plate (VA-LCP Condylar Plate 4.5/5.0) was simulated using computer-aided design (CAD) models of both implants (Fig 1).
The nail was bicortically locked in the distal fragment occupying its two most distal screw holes, and proximally with two anteroposterior screws. The plate was applied by occupying its three most distal VA locking holes for monocortical fixation of the distal fragment and inserting three bicortical VA locking screws in the shaft adjacent to the osteotomy. The two implants were positioned so that they could be interlinked with one common distal lateromedial (LM) screw.
Three different fixation configurations were simulated using (1) intramedullary nail only, (2) intramedullary nail and lateral plate without interlinking (the distal LM screw was only connected to the nail, but not to the plate), and (3) intramedullary nail and lateral plate, interlinked with the distal LM screw.
All materials were simulated as linear elastic. The Young's moduli of the bone elements were scaled according to the underlying local volumetric bone mineral density measured from the CT scan. All screws were modeled without threads bonded at the bone-screw and nail/plate-screw interfaces. Contact with friction was set between the nail and bone.
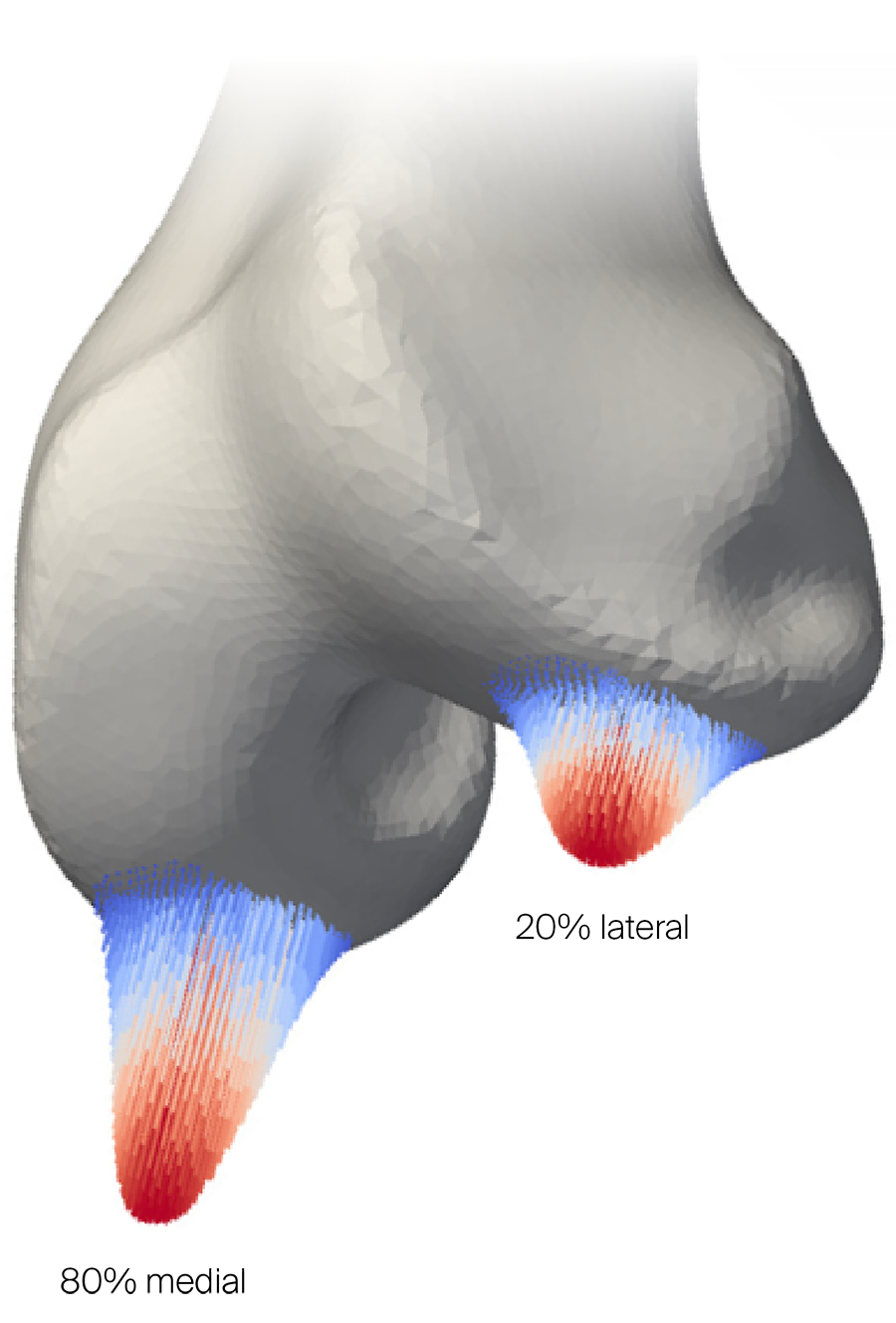
The distal femoral joint surface was loaded with 570 N, split over the lateral and medial condyles at a ratio of 20–80% to simulate a physiologically relevant full weight bearing situation with worst case scenario. The forces were directed toward the femoral head center with both condyle surfaces loaded according to a Gaussian distribution (Fig 2). The displacement of the femoral head was fully constrained, whereas the central point between the condyles was constrained in the transverse plane but free to move longitudinally. Primary stability of all three fixation configurations was evaluated by calculating the magnitude of the interfragmentary movement at the medial aspect of the fracture gap.
Results
Combining retrograde intramedullary nail and lateral plate fixation without interlinking could increase primary stability by 39%, whereas interlinking the two implants with a single distal LM screw provides 57% increase in stability compared with nailing alone.
Discussion
From a clinical perspective, combined nail and plate fixation could be biomechanically beneficial for treatment of native or periprosthetic osteoporotic comminuted distal femoral fractures with desired immediate full weight bearing. Further in vivo corroboration is needed to utilize this implant combination in the clinical practice.
You might also be interested in
Peri-implant fractures
Short vs long cephalomedullary nails following pertrochanteric fracture consolidation.
Rib fracture plating comparison
Intrathoracic plate fixation demonstrates significantly higher stiffness versus extrathoracic plating.
Tarsometatarsal joint fusion
Nitinol stables might demonstrate comparable performance to established techniques for fusion of the first TMT joint.
Improving fixation stability with ASL
The novel TN-A delivers new approaches to treating unstable distal tibia fractures.