Periprosthetic joint infection in 2025—genome, microbiome, and beyond
Preview
The human microbiome plays a crucial role in shaping human’s long-term health by modulating immune responses and protecting against infection. Disruptions in these microbial communities, known as dysbiosis, can increase susceptibility to infections, including postsurgical infections. In this third part of the series, Mustafa Citak from Helios ENDO-Klinik Hamburg, Hamburg, Germany, and Armita Armina Abedi from the Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg, and the Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark, will share current knowledge on the role of the human microbiome in surgical-site infections (SSIs) and periprosthetic joint infections (PJIs), with a focus on gut microbiome dysregulation, endogenous microbial sources of infection, and emerging strategies for prevention and patient optimization.

Mustafa Citak
Helios ENDO-Klinik Hamburg, Hamburg, Germany

Armita Armina Abedi
Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg; Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark
A look from within—the emerging role of the microbiome in joint infection
Total joint arthroplasty (TJA) is a safe and effective procedure that restores function and improves quality of life in patients with end-stage osteoarthritis (OA) [1]. However, its success can be undermined by PJI, a type of SSI that occurs in 1–2% of primary total joint replacement cases [2-4]. Periprosthetic joint infection occurs when microorganisms adhere to the implant surface and form biofilms that are resistant to host immune responses and antibiotics [5], leading to prolonged hospitalization, higher readmission rates, and increased morbidity and mortality [6].
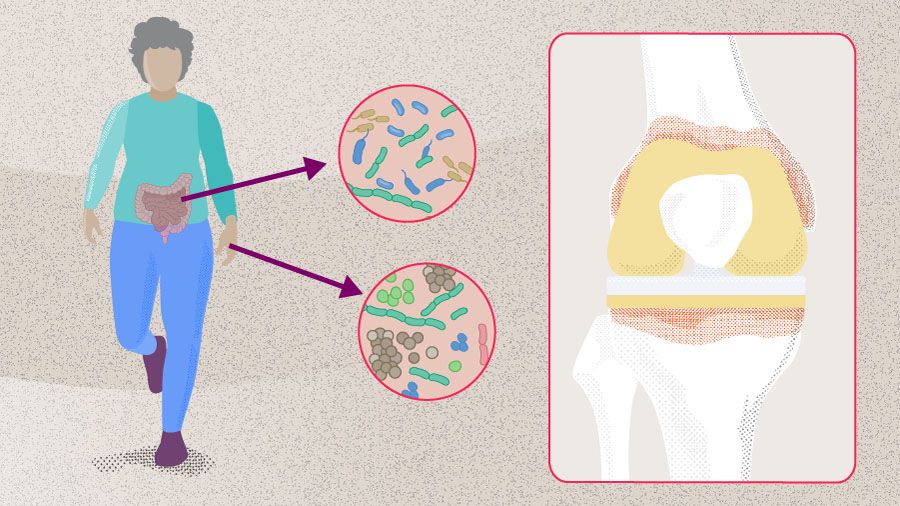
Despite advancements in operative techniques, implant manufacturing, and sterilization protocols (see Part 1 on PJI prevention), the prevalence of PJI continues to rise, largely due to the increasing number of TJA procedures performed annually [7, 8]. While most research has focused on minimizing exogenous sources of pathogens at the time of surgery, emerging evidence suggests that both SSI and PJI can originate from endogenous sources of microorganisms—particularly from the gastrointestinal (GI) tract in the context of dysbiosis and impaired gut permeability. This highlights the potential role of the human microbiome as a risk factor [9].
The human microbiome
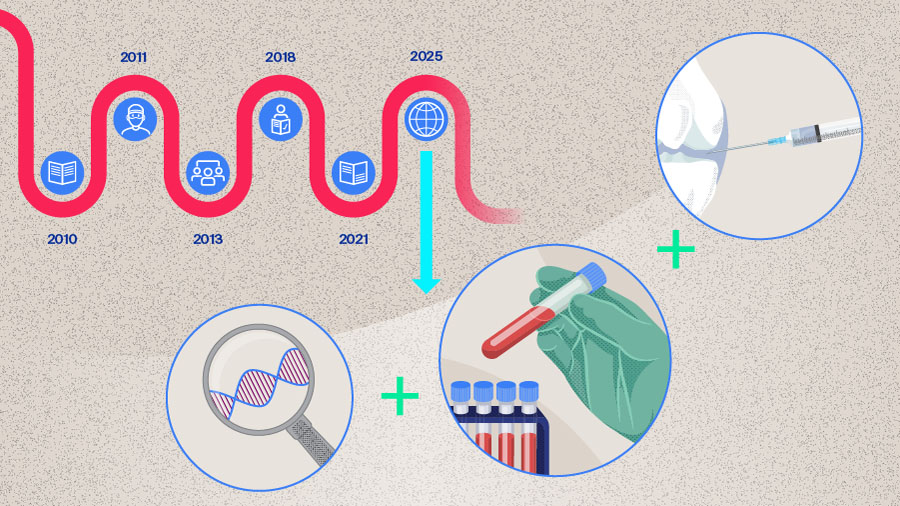
The human microbiome refers to the community of microorganisms that reside in and on our body, along with their collective genomes. It includes several species of bacteria, fungi, and viruses, with bacteria being the most abundant [10]. Evidence that microorganisms are part of the normal human system dates back to the late 19th century, when Theodor Escherich identified Escherichia coli in children’s intestinal flora and later studied the role of microbes in digestion and intestinal disease [11, 12]. Intensive study of the human microbiome began in the early 21st century and intensified after 2007 with the Human Microbiome Project (HMP), a 5-year large-scale collaborative effort to characterize microbial communities in the oral, nasal, vaginal, gut, and skin of healthy adults using 16S ribosomal RNA (rRNA) gene sequencing [10]. The HMP also included demonstration studies of disorders such as psoriasis and ulcerative colitis, revealing major differences in microbial composition between individuals and across body sites in a single individual; this supported the theory that different body sites are host to a “core microbiome” [9, 10]. Over the last decade, advances in high-throughput sequencing and computational methods have greatly improved our understanding of the human microbiota composition, function, and its role in physiology and disease [6]. Emerging evidence suggests that microbial composition varies in different areas of the body more than previously recognized. This knowledge is becoming increasingly relevant in orthopedic surgery, as recent studies implicate dysregulation of the skin and the gut microbiome as potential sources of SSI and PJI through mechanisms such as bacterial translocation or impaired immune responses [9]. In this article, we review the link between the microbiome, SSI, and PJI.
Read the full article with your AO login
- Microbiome’s emerging role
- Human microbiome
- Skin microbiome
- Joint microbiome
- Gut microbiome dysbiosis
- “Trojan Horse Hypothesis”
- Risk factors BMI and diabetes
- Clostridium difficile infection
- Conclusion
AO Recon resources
Contributing experts

Armita Armina Abedi
Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg
Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark

Kristen Barton
Midwest Orthopaedics at Rush, Rush University Medical Centre, Chicago
Department of Physical Therapy, Western University, London, Canada

Mustafa Citak
Helios ENDO-Klinik Hamburg, Hamburg, Germany

Jason Jennings
Colorado Joint Replacement, AdventHealth, Denver, Colorado
Department of Mechanical and Materials Engineering, University of Denver, Denver, Colorado
Department of Physical Therapy, University of Delaware, Newark, Delaware
This article was written by Chiara Cianciolo, AO Innovation Translation Center, Clinical Science, Switzerland.
References
-
Pulido L, Ghanem E, Joshi A, et al. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008 Jul;466(7):1710-1715.
-
Ahmed SS, Haddad FS. Prosthetic joint infection. Bone Joint Res. 2019 Nov;8(11):570-572.
-
Ong KL, Kurtz SM, Lau E, et al. Prosthetic joint infection risk after total hip arthroplasty in the Medicare population. J Arthroplasty. 2009 Sep;24(6 Suppl):105-109.
-
Corvec S, Portillo ME, Pasticci BM, et al. Epidemiology and new developments in the diagnosis of prosthetic joint infection. Int J Artif Organs. 2012 Oct;35(10):923-934.
-
Izakovicova P, Borens O, Trampuz A. Periprosthetic joint infection: current concepts and outlook. EFORT Open Reviews. 2019 29 Jul. 2019;4(7):482-494.
-
Longo UG, Lalli A, Bandini B, et al. The influence of gut microbiome on periprosthetic joint infections: State-of-the art. Journal of ISAKOS. 2024 2024/06/01/;9(3):353-361.
-
Kurtz SM, Lau EC, Son M-S, et al. Are We Winning or Losing the Battle With Periprosthetic Joint Infection: Trends in Periprosthetic Joint Infection and Mortality Risk for the Medicare Population. The Journal of Arthroplasty. 2018;33(10):3238-3245.
-
He M-C, Ferrini A, Parvizi J. Periprosthetic joint infection: Time to think outside the box. Knee Surgery, Sports Traumatology, Arthroscopy.n/a(n/a).
-
Heckmann ND, Culler MW, Mont MA, et al. Emerging Concepts in Periprosthetic Joint Infection Research: The Human Microbiome. J Arthroplasty. 2025 Jul;40(7):1821-1826.
-
Turnbaugh PJ, Ley RE, Hamady M, et al. The Human Microbiome Project. Nature. 2007 2007/10/01;449(7164):804-810.
-
Escherich T. Die darmbakterien des säuglings und ihre beziehungen zur physiologie der Verdauung: Enke; 1886.
-
Escherich T. Die Darmbacterien des Neugeborenen und Säuglings. Fortschritte der Medicin. 1885;3(16 und 17):515-554.
-
Mengistu DA, Alemu A, Abdukadir AA, et al. Global Incidence of Surgical Site Infection Among Patients: Systematic Review and Meta-Analysis. Inquiry. 2023 Jan-Dec;60:469580231162549.
-
Long DR, Bryson-Cahn C, Waalkes A, et al. Contribution of the patient microbiome to surgical site infection and antibiotic prophylaxis failure in spine surgery. Sci Transl Med. 2024 Apr 10;16(742):eadk8222.
-
Hayden HS, Joshi S, Radey MC, et al. Genome Capture Sequencing Selectively Enriches Bacterial DNA and Enables Genome-Wide Measurement of Intrastrain Genetic Diversity in Human Infections. mBio. 2022 Oct 26;13(5):e0142422.
-
Fernández-Rodríguez D, Baker CM, Tarabichi S, et al. Mark Coventry Award: Human Knee Has a Distinct Microbiome: Implications for Periprosthetic Joint Infection. J Arthroplasty. 2023 Jun;38(6s):S2-s6.
-
He M, Kolhoff F, Mont MA, Parvizi J. Is Osteoarthritis a State of Joint Dysbiosis? Antibiotics. 2025;14(6):609.
-
Arumugam M, Raes J, Pelletier E, et al. Enterotypes of the human gut microbiome. Nature. 2011 2011/05/01;473(7346):174-180.
-
Gilbert JA, Blaser MJ, Caporaso JG, et al. Current understanding of the human microbiome. Nature Medicine. 2018 2018/04/01;24(4):392-400.
-
DeGruttola AK, Low D, Mizoguchi A, Mizoguchi E. Current Understanding of Dysbiosis in Disease in Human and Animal Models. Inflamm Bowel Dis. 2016 May;22(5):1137-1150.
-
Chisari E, Cho J, Wouthuyzen-Bakker M, Parvizi J. Periprosthetic Joint Infection and the Trojan Horse Theory: Examining the Role of Gut Dysbiosis and Epithelial Integrity. The Journal of Arthroplasty. 2022;37(7):1369-1374.
-
Chisari E, D'Mello D, Sherman MB, Parvizi J. Inflammatory Bowel Diseases Increase the Risk of Periprosthetic Joint Infection. J Bone Joint Surg Am. 2022 Jan 19;104(2):160-165.
-
Zhu H, Jin H, Zhang C, Yuan T. Intestinal methicillin-resistant Staphylococcus aureus causes prosthetic infection via 'Trojan Horse' mechanism: Evidence from a rat model. Bone Joint Res. 2020 Apr;9(4):152-161.
-
Krezalek MA, Hyoju S, Zaborin A, et al. Can Methicillin-resistant Staphylococcus aureus Silently Travel From the Gut to the Wound and Cause Postoperative Infection? Modeling the "Trojan Horse Hypothesis". Ann Surg. 2018 Apr;267(4):749-758.
-
Chisari E, Cho J, Wouthuyzen-Bakker M, Parvizi J. Gut permeability may be associated with periprosthetic joint infection after total hip and knee arthroplasty. Scientific Reports. 2022 2022/09/05;12(1):15094.
-
Wilson CJ, Georgiou KR, Oburu E, et al. Surgical site infection in overweight and obese Total Knee Arthroplasty patients. Journal of Orthopaedics. 2018 2018/06/01/;15(2):328-332.
-
Chaudhry H, Ponnusamy K, Somerville L, et al. Revision Rates and Functional Outcomes Among Severely, Morbidly, and Super-Obese Patients Following Primary Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. JBJS Reviews. 2019;7(7).
-
Budin M, Sandiford NA, Gehrke T, Citak M. Body mass index matters: morbid obese patients have different microorganism profiles in the setting of periprosthetic hip joint infections. Int Orthop. 2025 Jun;49(6):1309-1317.
-
Camilleri M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut. 2019;68(8):1516-1526.
-
Pedersen AB, Mehnert F, Johnsen SP, Sørensen HT. Risk of revision of a total hip replacement in patients with diabetes mellitus: a population-based follow up study. J Bone Joint Surg Br. 2010 Jul;92(7):929-934.
-
Maradit Kremers H, Lewallen LW, Mabry TM, et al. Diabetes Mellitus, Hyperglycemia, Hemoglobin A1C and the Risk of Prosthetic Joint Infections in Total Hip and Knee Arthroplasty. The Journal of Arthroplasty. 2015 2015/03/01/;30(3):439-443.
-
Ergin M, Budin M, Canbaz SB, et al. Microbial Diversity of Periprosthetic Joint Infections in Diabetic and Nondiabetic Patients Following Hip Arthroplasty. J Arthroplasty. 2025 Feb;40(2):494-498.
-
Mada PK, Alam MU. Clostridioides difficile infection. StatPearls. Treasure Island (FL): StatPearls Publishing
Copyright © 2025, StatPearls Publishing LLC.; 2025. -
Verhey JT, Boddu SP, Tarabichi S, et al. Gut-Joint Axis: History of Clostridium Difficile Infection Increases the Risk of Periprosthetic Joint Infection After Total Knee Arthroplasty. J Arthroplasty. 2025 Aug;40(8):2126-2130.
-
Deckey DG, Boddu SP, Verhey JT, et al. Clostridium difficile Infection Prior to Total Hip Arthroplasty Independently Increases the Risk of Periprosthetic Joint Infection. The Journal of Arthroplasty. 2024;39(9):S444-S448.e441.
-
Ramasamy B, Sharma DK, Callary SA, et al. Role of gut microbiota disruption in prosthetic joint infection: a scoping review. The Lancet Microbe.
-
Atipiboonsin V, Chisari E, Megaloikonomos PD, et al., editors. G25 – Does gut microbiome have a role in the development of Surgical Site Infection (SSI) and/or Periprosthetic Joint Infection (PJI) in patients undergoing major orthopedic surgery? The International Consensus Meeting on Infection (ICMI); 2025 8-10 May, 2025; Istambul2025.
-
Shahi A, Goswami K, Drago L, et al., editors. G26: Does the Use of Probiotic Agents Have Any Role in Preventing Surgical Site Infection (SSI)/Periprosthetic Joint Infection (PJI) After Major Orthopedic Surgery? The International Consensus Meeting on Infection (ICMI); 2025 8-10 May, 2025; Istambul2025.