Diagnosis of periprosthetic joint infection—what is the current thinking?
Preview
Diagnosing a periprosthetic joint infection (PJI) may be easy for a clinician when a patient presents with a purulent wound. But what about the patient with a chronic, more indolent infection? Periprosthetic joint infection presents in many ways, so how can it be best diagnosed? In this part of the series, Jason Jennings from the Department of Mechanical and Materials Engineering, University of Denver, Colorado, and the Department of Physical Therapy, University of Delaware, Delaware and Kristen Barton from Midwest Orthopaedics at Rush, Rush University Medical Centre, Chicago, and the Department of Physical Therapy, Western University, Canada, walk us through the known diagnostic criteria for PJI, explaining PJI testing, and the history of the guidelines, while giving us first-hand insights into the latest changes from the recently convened 2025 International Consensus Meeting (ICM).

Jason Jennings
Colorado Joint Replacement, AdventHealth, Denver, Colorado
Department of Mechanical and Materials Engineering, University of Denver, Denver, Colorado
Department of Physical Therapy, University of Delaware, Newark, Delaware

Kristen Barton
Midwest Orthopaedics at Rush, Rush University Medical Centre, Chicago
Department of Physical Therapy, Western University, London, Canada
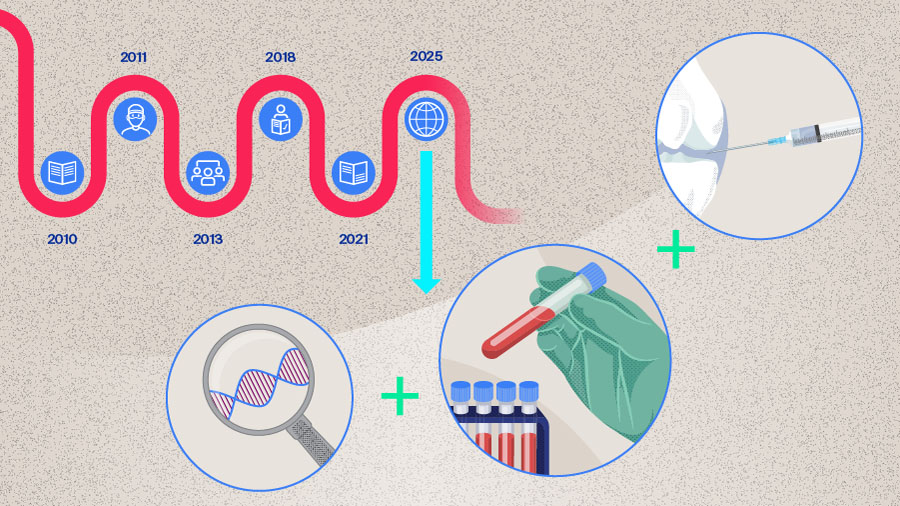
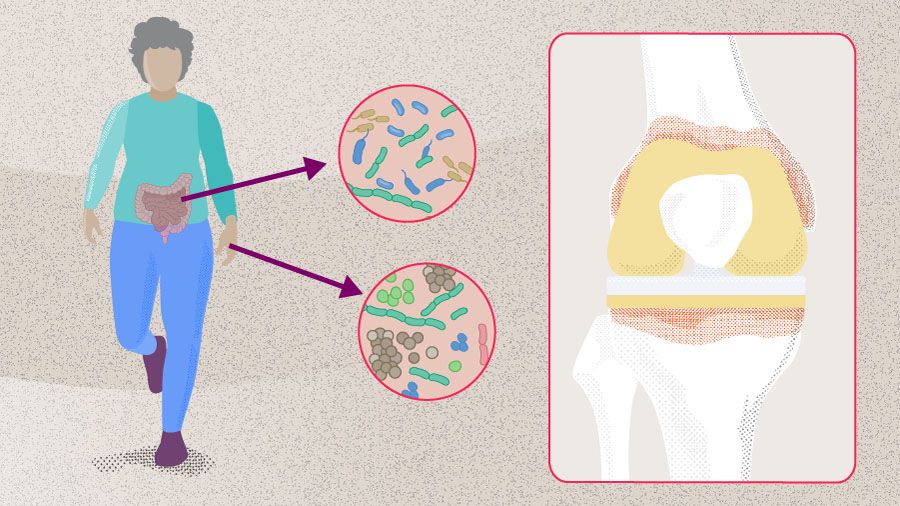
Periprosthetic joint infection is a challenging clinical phenomenon, for which no gold standard diagnostic test is available [1, 2] and for which proposed definitions are closely linked to the fulfilment of PJI diagnostic criteria [1, 3–5]. Over the last several years, these diagnostic criteria have undergone multiple iterations from different groups and have achieved varying levels of acceptance in the clinical landscape [5]. Having a good understanding of how the guidelines have evolved and their differences may help the clinician better diagnose PJI by increasing awareness of the practicalities and subtleties of the diagnostic criteria. At the same time it also provides great insight into the challenges that a clinician may face when confronted with a patient with potential PJI, a potentially complex situation that may lead to invasive treatment with a risk of significant adverse events [5].
A brief history of the periprosthetic joint infection diagnostic guidelines
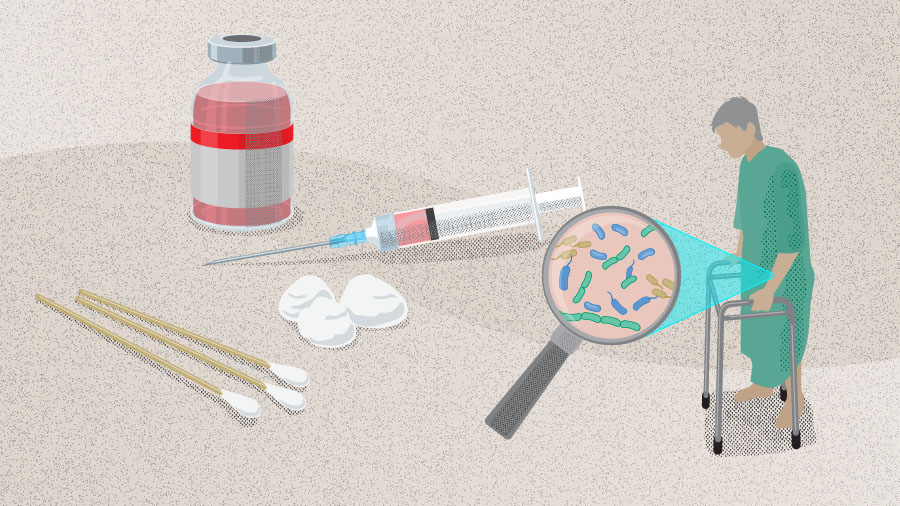
In 2010, Della Valle et al [6] published a clinical practice guideline approved by the American Academy of Orthopaedic Surgeons (AAOS) on the diagnosis of PJI of the hip and knee. The goal at the time was to improve PJI treatment based on the evidence available, and as a result the authors produced two practical diagnostic algorithms, one for patients with a high probability of hip or knee PJI and one for those with a low probability [6]. The authors also included 15 recommendations for the diagnosis of PJI [6]. The outgoing question for both algorithms was based on elevated erythrocyte sedimentation rate (ESR) or C-reactive protein level (CRP), followed by joint aspiration to assess cell count, differential, culture, and later frozen sections and/or intraoperative synovial fluid white blood cell (WBC) count and differential [6]. In high probability PJI patients, nuclear imaging was also recommended, with modalities including labeled leukocyte imaging combined with bone or bone marrow imaging, fluorine-18 fluorodeoxyglucose positron-emission tomography, gallium imaging, or labeled leukocyte imaging [6]. Around the same time, the Musculoskeletal Infection Society (MSIS), convened a workgroup to propose a new definition for PJI [3] aiming to achieve a “gold standard” definition. In addition to the two clear-cut major criteria (1) a sinus tract communicating with the prosthesis or (2) pathogen isolated by culture from at least two separate tissue or fluid samples from the affected prosthetic joint, there were six minor criteria based on serum and synovial tests as well as histology [3]. Similar to Della Valle et al’s AAOS guidelines [6], the first three of these minor criteria were (1) elevated serum ESR and CRP (where elevated pertained to an ESR of > 30 mm/h and a CRP of > 10 mg/L), followed by (2) elevated synovial leukocyte count and (3) elevated synovial neutrophil percentage (synovial leukocyte count of 1100–4000 cells/µL and polymorphonuclear neutrophils [PMN]% of 64–69%) [3]. It was noted in this guideline that, firstly, there is variance in laboratory tests that should be taken into account when performing serum tests, and secondly, the PMN% corresponds to chronically infected knee arthroplasties, whereas acute infections (defined as less than 3 months from index surgery or from symptom onset) can lead to much higher levels (synovial leukocyte count of 27,800 cells/µL and PMN% of 89%, based on primary total knee arthroplasties with knee aspiration within 6 weeks of surgery in a study by Bedair et al [7]) [3]. Other minor criteria involved (4) purulence of the affected joint, (5) isolation of a microorganism in one culture of periprosthetic tissue or fluid, or (6) histological examination of periprosthetic tissue for the presence of neutrophils [3]. Here, the presence of four or more minor criteria indicated a PJI. These diagnostic tests became the “gold standard” of PJI diagnosis and became ingrained in clinical practice.
Over time, as diagnostic capabilities evolved, new biomarkers for PJI were identified and were introduced into diagnostic testing. Moving forward, in 2013 an expert group convened to form the first International Consensus Meeting (ICM) on PJI [1]. The group endorsed the definition of PJI from the MSIS but added a new test to the minor criteria—the leukocyte esterase (LE) test—while defining thresholds for the minor diagnostic criteria and modifying the AAOS algorithms [1]. The LE test is a rapid test which is used to identify the presence of LE, an enzyme produced by activated neutrophils in response to inflammation (Table 1).
Read the full article with your AO login
- PJI diagnostic guidelines history
- PJI diagnostic tests:
- Serological testing
- Synovial testing - Novel biomarkers:
- Calprotectin
- Fibrinolytic markers
- Procalcitonin - Genetic testing:
- mPCR technique
- Next-gen sequencing - Intraoperative PJI diagnosis
- Future diagnostic criteria set
- Conclusion
AO Recon resources
Contributing experts

Armita Armina Abedi
Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg
Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark

Kristen Barton
Midwest Orthopaedics at Rush, Rush University Medical Centre, Chicago
Department of Physical Therapy, Western University, London, Canada

Mustafa Citak
Helios ENDO-Klinik Hamburg, Hamburg, Germany

Jason Jennings
Colorado Joint Replacement, AdventHealth, Denver, Colorado
Department of Mechanical and Materials Engineering, University of Denver, Denver, Colorado
Department of Physical Therapy, University of Delaware, Newark, Delaware
This article was written by Lyndsey Kostadinov, AO Innovation Translation Center, Clinical Science, Switzerland.
References
-
Parvizi J, Gehrke T. Definition of periprosthetic joint infection. J Arthroplasty. 2014;29(7):1331.
-
Quinlan ND, Jennings JM. Joint aspiration for diagnosis of chronic periprosthetic joint infection: when, how, and what tests? Arthroplasty. 2023;5(1):43.
-
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469(11):2992–2994.
-
Shohat N, Bauer T, Buttaro M, Budhiparama N, Cashman J, Della Valle CJ, et al. Hip and Knee Section, What is the Definition of a Periprosthetic Joint Infection (PJI) of the Knee and the Hip? Can the Same Criteria be Used for Both Joints?: Proceedings of International Consensus on Orthopedic Infections. J Arthroplasty. 2019;34(2s):S325–s327.
-
McNally M, Sousa R, Wouthuyzen-Bakker M, Chen AF, Soriano A, Vogely HC, et al. The EBJIS definition of periprosthetic joint infection. Bone Joint J. 2021;103-b(1):18–25.
-
Della Valle C, Parvizi J, Bauer TW, Dicesare PE, Evans RP, Segreti J, et al. Diagnosis of periprosthetic joint infections of the hip and knee. J Am Acad Orthop Surg. 2010;18(12):760–770.
-
Bedair H, Ting N, Jacovides C, Saxena A, Moric M, Parvizi J, et al. The Mark Coventry Award: diagnosis of early postoperative TKA infection using synovial fluid analysis. Clin Orthop Relat Res. 2011;469(1):34–40.
-
Mont MA, Backstein DJ, Krebs VE, Mason JB, Taunton MJ, Callaghan JJ. Evidence-Based Validation of Diagnostic Criteria for Periprosthetic Joint Infection: A Major Step Forward! J Arthroplasty. 2018;33(5):1307–1308.
-
Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, et al. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J Arthroplasty. 2018;33(5):1309–1314.e1302.
-
Sigmund IK, Luger M, Windhager R, McNally MA. Diagnosing periprosthetic joint infections : a comparison of infection definitions: EBJIS 2021, ICM 2018, and IDSA 2013. Bone Joint Res. 2022;11(9):608–618.
-
Sebastian S, Parvizi J, Hofstaetter JG. Diagnostic Guidelines for Periprosthetic Joint Infection: Know the Differences. J Arthroplasty. 2025.
-
Pupaibool J, Plate JF, Hoffman A, Sebastian S, Birinci M, Kuiper J, et al. Is there a role for joint specific (hip vs knee) cut-offs for serological tests in diagnosis of prosthetic joint infection (PJI)? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
Plate JF, Hoffman A, Lin RT, Sebastian S, Klaber I, Grzelecki D, et al. Is there a role for joint specific (hip vs knee) cut-offs for synovial tests in diagnosis of periprosthetic joint infection? . 3rd Meeting of the International Concensus Meeting; Istanbul, Turkiye2025.
-
Linton A, Behairy W, Laoruengthana A, Ponzio D, Prieto H, Zhang X, et al. Is the accuracy of serum and/or synovial biomarkers for the diagnosis of periprosthetic joint infection (PJI) affected by the presence of inflammatory conditions? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
Grzelecki D, Sypień P, Birlutiu R-M, Abdelnasser MK, Bue M, von Eisenhart-Rothe R, et al. Is there a role for synovial calprotectin in the diagnosis of periprosthetic joint infection (PJI)? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
Shahi A, Sánchez RA, Davis C, Mathis K, Martinez S, Girones LB, et al. Is there a role for fibrinolytic serological markers, such as fibrinogen and D-dimer, in the diagnosis of periprosthetic joint infection (PJI)? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
Abdelnasser MK, Bayam L, Ponnampalavanar S, Lumban-Gaol I, Chinoy MA, Birlutiu R-M, et al. Is there a role for serum procalcitonin for diagnosis of periprosthetic joint infection (PJI).? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
Hao L, Wen P, Song W, Zhang B, Wu Y, Zhang Y, et al. Direct detection and identification of periprosthetic joint infection pathogens by metagenomic next-generation sequencing. Scientific Reports. 2023;13(1):7897.
-
Mortazavi SMJ, Hosseini-Monfared P, Abdelnasser MK, Karim MMA, M. E, Dao TT, et al. In doubtful cases for periprosthetic joint infection, what is the best intraoperative test to confirm or refute the diagnosis? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
American Joint Replacement Registry (AJRR): 2024 Annual Report. Rosemont, IL: American Academy of Orthopaedic Surgeons (AAOS), 2024.