Prevention of periprosthetic joint infection—have we been barking up the wrong tree?
Preview
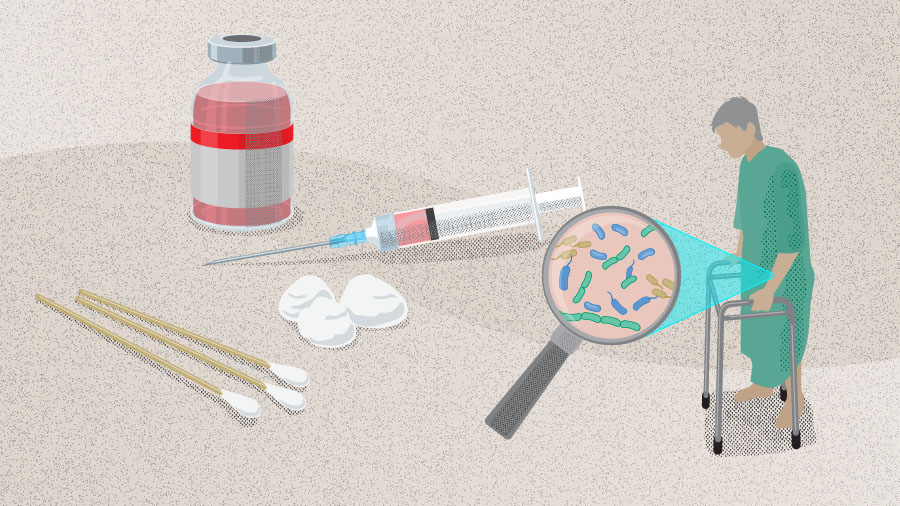
Periprosthetic joint infection (PJI) is a devastating complication of total joint arthroplasty with often poor outcomes. Many are familiar with diagnosis and treatment of PJI which is crucial as this can impact the need for future surgeries such as revision total joint arthroplasty (TJA); yet prevention of PJI is gaining importance, not only for the surgeon but also for the patient. A growing shift in clinical focus emphasizes prevention over treatment, driven by an increased awareness of risk factors, modification of risk factors, and the significant impact of PJI following TJA on patient morbidity and mortality.
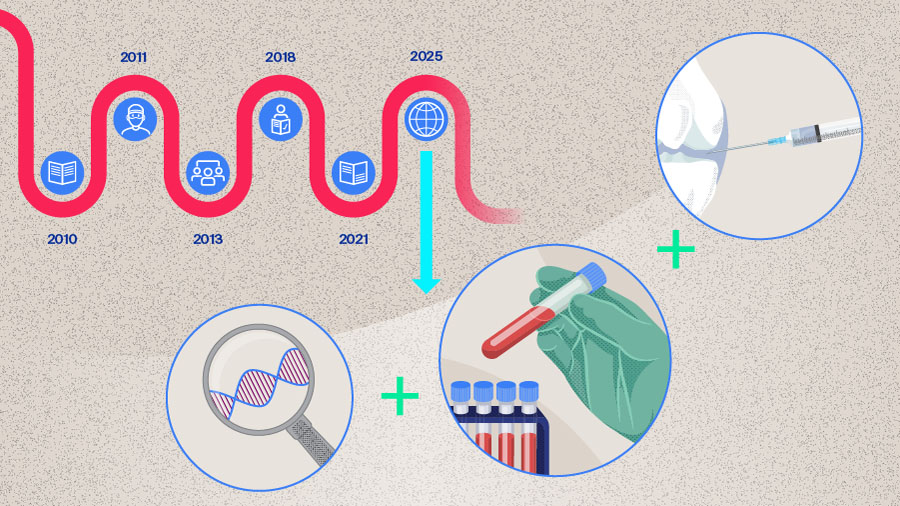
In this part of the series, Mustafa Citak from the Helios ENDO-Klinik Hamburg, Hamburg, Germany, and Armita Armina Abedi from the Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg; Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark lead us through the recently published ten steps to infection prevention, bring updates from the recent 3rd International Consensus Meeting (ICM), and provide their insights into prevention of PJI in the real world.

Mustafa Citak
Helios ENDO-Klinik Hamburg, Hamburg, Germany

Armita Armina Abedi
Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg; Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark
Periprosthetic joint infection has a wide-reaching impact
Periprosthetic joint infection is considered one of the most frequent and serious complications after TJA. According to the American Joint Replacement Registry [1], infection remained the most common indication for both revision hip arthroplasty and revision knee arthroplasty in 2024. The incidence of PJI after TJA is around 1–2%, and the number of TJAs taking place is increasing with the aging population [2]. On this topic, Citak comments, “We are seeing an increase in the number of PJIs as the number of TJAs taking place are increasing worldwide. However, the rate of PJI is still the same. This may reflect the impact of PJI prevention measures. There is a growing awareness within the surgical community regarding modifiable risk factors, such as body mass index and diabetes, and we can see that there is a definite focus on optimizing the risk factors to reduce the risk of PJI.”
According to Gehrke et al [3] PJI may lead to “surgical failure, revision surgery, amputation, or death”. This underscores the ever growing need to focus on the prevention of PJI. To this end, this article presents up-to-date knowledge on PJI prevention in TJA.
Polymicrobial infections and antibiotic resistance complicate the status quo
In patients undergoing primary and revision TJA, infections are most often detected as monomicrobial, ie, as caused by a single pathogen; however, polymicrobial infections involving two or more causative pathogens may also occur and have been associated with poorer clinical outcomes compared with infections caused by just one microbe [3]. Other issues include antimicrobial resistance and virulence, which may affect both treatment and identification of the causative pathogen [3].
In light of the complexity of both the diagnosis of PJI—discussed in Part 2 of this series— and its treatment, prevention has emerged as a central focus in TJA, not only for patients but also the surgeons [3]. It may be regarded as a change in the status quo, a shift from treatment to prevention, with infection prevention strategies now encompassing the entire surgical pathway. As Citak notes, “We are taking more care about prevention because it will not help the patient if we create an unnecessary infection, and we have the opportunity and knowledge now to consider and modify risk factors before surgery.” As Citak pointed out, “These topics are now being discussed, such as at the recent 3rd ICM in Turkey. First you identify the possible risk factors and then later you have to consider how to modify them. Now, prevention is a hot topic and the focus of avid discussion at every meeting.”
Read the full article with your AO login
- Periprosthetic joint infection
- Antibiotic resistance complications
- Infection prevention
- Patient risk factor impact
- Microbial load reduction
- Antibiotic prophylaxis
- Best practices in the OR
- Sterilization
- Wound management
- Novel methods
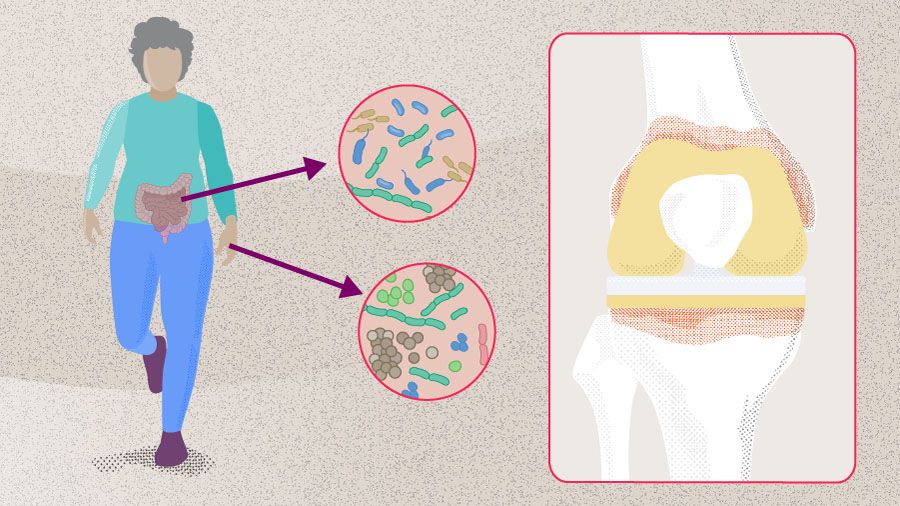
- Gut microbiome
- Conclusion
AO Recon resources
Contributing experts

Armita Armina Abedi
Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg
Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark

Kristen Barton
Midwest Orthopaedics at Rush, Rush University Medical Centre, Chicago
Department of Physical Therapy, Western University, London, Canada

Mustafa Citak
Helios ENDO-Klinik Hamburg, Hamburg, Germany

Jason Jennings
Colorado Joint Replacement, AdventHealth, Denver, Colorado
Department of Mechanical and Materials Engineering, University of Denver, Denver, Colorado
Department of Physical Therapy, University of Delaware, Newark, Delaware
This article was written by Lyndsey Kostadinov, AO Innovation Translation Center, Clinical Science, Switzerland.
References
-
American Joint Replacement Registry (AJRR): 2024 Annual Report. Rosemont, IL: American Academy of Orthopaedic Surgeons (AAOS), 2024.
-
Ayoade F, Li D, Mabrouk A, al. e. Periprosthetic Joint Infection. [Updated 2023 Oct 14]. StatPearls [Internet]. Treasure Island [FL]: StatPearls Publishing; 2025.
-
Gehrke T, Citak M, Parvizi J, Budhiparama NC, Akkaya M. Periprosthetic joint infections: state-of-the-art. Archives of Orthopaedic and Trauma Surgery. 2024;145(1):58
-
Tarabichi S, Parvizi J. Prevention of surgical site infection: a ten-step approach. Arthroplasty. 2023;5(1):21.
-
Yilmaz MK, Celik N, Tarabichi S, Abbaszadeh A, Parvizi J. Evidence-based Approach for Prevention of Surgical Site Infection. Hip Pelvis. 2024;36(3):161–167.
-
Ahmed SO, Veloso M, Sabater-Martos M, Ploegmakers J, Jennings JM, Kaplan N, et al. What are the modifiable risk factors for postoperative infection in patients undergoing major orthopaedic surgery? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
Von Rehlingen-Prinz F, Röhrs M, Sandiford N, Garcia EG, Schulmeyer J, Salber J, et al. Preoperative MRSA screening using a simple questionnaire prior elective total joint replacement. Arch Orthop Trauma Surg. 2024;144(12):5157–5164.
-
Lizcano JD, Pelt C, Norambuena GA, Martinez D, Sieidelman J, Riaz T, et al. What is the optimal nasal decolonization agent for patients undergoing major orthopaedic surgery? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
Chao CA, Khilnani TK, Jo S, Shenoy A, Bostrom MPG, Carli AV. Not All Antiseptic Solutions Are Equivalent in Removing Biofilm: A Comparison Across Different Orthopaedic Surfaces. J Bone Joint Surg Am. 2025;107(2):127–133.
-
Shahi A, Long W, Guild G, Mathis K, Uchiyama K, Uckay I, et al. Should the administration of prophylactic antibiotics be weight-based? 3rd Meeting of the International Consensus Meeting Istanbul Turkiye 2025.
-
Kubsad S, Collins AP, Dasari SP, Chansky HA, Fernando ND, Hernandez NM. Impact of Extended Prophylactic Antibiotics on Risk of Prosthetic Joint Infection in Primary Total Hip Arthroplasty: A Matched Cohort Analysis. J Am Acad Orthop Surg. 2025;33(6):307-312.
-
Gallo J, Nieslanikova E. Prevention of Prosthetic Joint Infection: From Traditional Approaches towards Quality Improvement and Data Mining. J Clin Med. 2020;9(7).
-
Ainslie-Garcia M, Anderson LA, Bloch BV, Board TN, Chen AF, Craigie S, et al. International Delphi Study on Wound Closure and Incision Management in Joint Arthroplasty Part 2: Total Hip Arthroplasty. J Arthroplasty. 2024;39(6):1524–1529.
-
Ainslie-Garcia M, Anderson LA, Bloch BV, Board TN, Chen AF, Craigie S, et al. International Delphi Study on Wound Closure and Dressing Management in Joint Arthroplasty: Part 1: Total Knee Arthroplasty. J Arthroplasty. 2024;39(4):878–883.
-
Abedi AO, Abedi AA, Parvizi J. Prevention of surgical site infection: need to focus on the enemy within. Journal of Joint Surgery and Research. 2025;3(1):73–77.