Common modifiable risk factors in total joint arthroplasty: a 2021 update—obesity
Preview
In a 2019 clinical practice guideline published by the American Academy of Orthopaedic Surgeons, it was stated that, among all risk factors evaluated, only obesity could be deemed as having reached the level of moderate strength evidence as a risk factor for periprosthetic joint infection (PJI) [1]. In the guideline, all three moderate-quality studies used body mass index (BMI) as a global measure of obesity, and all three determined that a statistically significant increase in adverse outcomes was associated with a BMI greater than 35 kg/m2. Is BMI the best indicator of obesity and surgical difficulty? Are there other ways to determine if an obese patient is suitable for an arthroplasty? What does the proper management of obese patients look like? Michael A Mont, MD, Orthopaedic Surgeon, Rubin Institute for Advanced Orthopedics, introduces the evidence on this topic and shares his experience with us.

Michael A Mont
Rubin Institute for Advanced Orthopedics
Baltimore, United States
High BMI: a cause for delaying or denying obese patients of arthroplasty?
As patients who have BMIs ≥ 40–50 kg/m2 (ie, morbidly obese and super obese patients) are increasingly among the arthroplasty patients, more evidence is now available that these patients are at risk for increased complications and worse outcomes [2–6]. Various reasons have been theorized for the cause for unfavorable outcomes in obese patients, and these include underdosing of preoperative antibiotics, thicker subcutaneous adipose tissue at the surgical site (leading to poor perfusion and lower oxygen tension in tissues, technical difficulties during surgery, as well as longer surgical times), and more frequent nasal Staphyloccocus aureus colonization [2, 7].
The exact BMI cutoff that marks a significant rise of worse outcome after TJA is still controversial [2, 8, 9]. While the balance of benefits and risks in delaying or denying patients with BMIs is still being debated, institutional (or individual) restrictions have already been applied to some obese patients in their access to TJA. In fact, other weight risk factors, such as patients who have BMI lower than 18 kg/m2 may sometimes be at a greater risk of negative outcomes due to malnutrition and low albumin [7, 10–12].
Evolving BMI thresholds of increased adverse outcomes after total joint arthroplasty
Before 2011, comparisons of BMI above and below 30 kg/m2 were frequently made in studying these relationships and the occurrence of infection after TJA [13–15]. Since then, much effort has been made in finding a BMI value that can serve as a clear threshold above which a significant increase of negative outcomes, whether it be PJI, readmission, reoperation, or a long list of other complications, can be expected. A few examples from recent publications are given below:
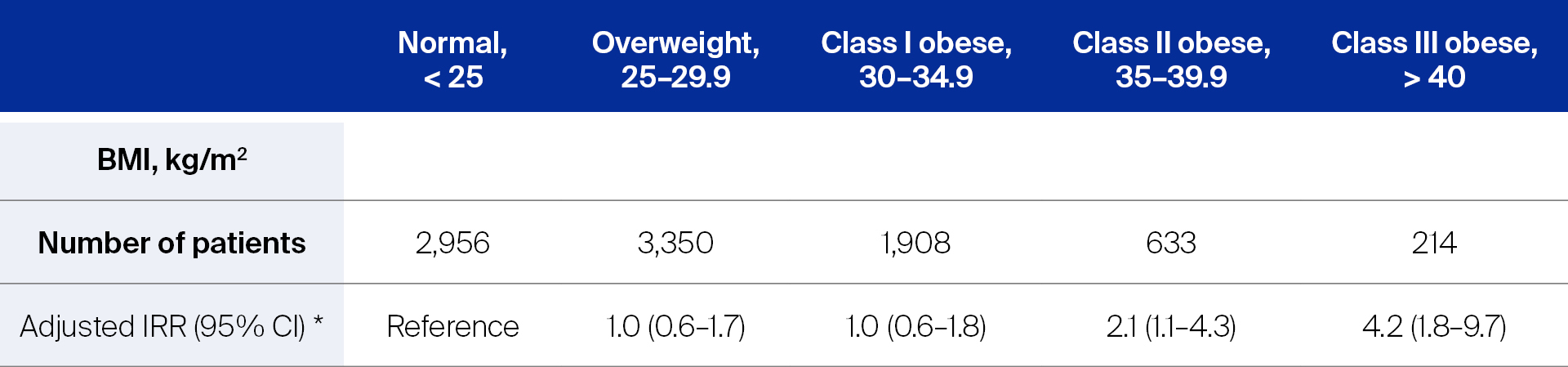
- For the purpose of prophylactic antibiotic dosing for patients undergoing TJA, Lübbeke et al [2] conducted a study in a prospective, hospital-based cohort (9,061 patients) of primary TJA patients to investigate the influence of obesity on the incidence of PJI. Dividing the patients into five BMI categories according to the World Health Organization (WHO) definition, the adjusted incidence rate ratio (IRR) of PJI was calculated using patients who had normal BMI as the reference for the four other BMI categories. As can be seen in Table 1 below, while the IRR of PJI in the overweight and Class I obese patients remained similar to the patients who had normal BMI, it was clearly higher in Class II and III obese patients.
Lübekke et al [2] concluded that after primary TJA, patients who had a BMI of ≥ 35 had more than double the rate of PJI than patients who had a BMI < 35.
Abbreviations: BMI, body mass index; IRR, incidence rate ratio; CI, confidence interval.
* Cox regression analyses performed with adjustments for covariates such as age, sex, smoking status, diabetes, and use of antibiotic-laden cement.
Read the full article with your AO login
- Do obese patients benefit from arthroplasties as much as patients who have normal BMI?
- Central versus peripheral obesity
- A patient-centered approach: allowing and motivating patients to invest in their own medical future
- Conclusion
Additional AO resources
Access videos, tools, and other assets.
- Videos
- AOF books in Thieme store
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Matthew P Abdel
Mayo Clinic
Rochester, United States

Steven MacDonald
University of Western Ontario
London, Canada

Michael A Mont
Rubin Institute for Advanced Orthopedics
Baltimore, United States
This article was compiled by Maio Chen, Senior Project Manager Medical Writing, AO Foundation, Switzerland.
References
- AAOS. Diagnosis and Prevention of Periprosthetic Joint Infections, Evidence-Based Clinical Practice Guideline2019 July 28, 2021.
- Lübbeke A, Zingg M, Vu D, et al. Body mass and weight thresholds for increased prosthetic joint infection rates after primary total joint arthroplasty. Acta Orthop. 2016;87(2):132–138.
- Issa K, Harwin SF, Malkani AL, et al. Bariatric Orthopaedics: Total Hip Arthroplasty in Super-Obese Patients (Those with a BMI of ≥50 kg/m2). J Bone Joint Surg Am. 2016 Feb 3;98(3):180–185.
- Wagner ER, Kamath AF, Fruth K, et al. Effect of Body Mass Index on Reoperation and Complications After Total Knee Arthroplasty. J Bone Joint Surg Am. 2016 Dec 21;98(24):2052–2060.
- George J, Piuzzi NS, Jawad MM, et al. Reliability of International Classification of Diseases, Ninth Edition, Codes to Detect Morbid Obesity in Patients Undergoing Total Hip Arthroplasty. J Arthroplasty. 2018 Sep;33(9):2770–2773.
- George J, Piuzzi NS, Ng M, et al. Association Between Body Mass Index and Thirty-Day Complications After Total Knee Arthroplasty. J Arthroplasty. 2018 Mar;33(3):865–871.
- Boyce L, Prasad A, Barrett M, et al. The outcomes of total knee arthroplasty in morbidly obese patients: a systematic review of the literature. Arch Orthop Trauma Surg. 2019 Apr;139(4):553–560.
- Adhikary SD, Liu WM, Memtsoudis SG, et al. Body Mass Index More Than 45 kg/m(2) as a Cutoff Point Is Associated With Dramatically Increased Postoperative Complications in Total Knee Arthroplasty and Total Hip Arthroplasty. J Arthroplasty. 2016 Apr;31(4):749–753.
- Kwasny MJ, Edelstein AI, Manning DW. Statistical Methods Dictate the Estimated Impact of Body Mass Index on Major and Minor Complications After Total Joint Arthroplasty. Clinical orthopaedics and related research. 2018;476(12):2418–2429.
- Roth A, Anis HK, Emara AK, et al. The Potential Effects of Imposing a Body Mass Index Threshold on Patient-Reported Outcomes After Total Knee Arthroplasty. J Arthroplasty. 2021 Jul;36(7s):S198–s208.
- Giori NJ, Amanatullah DF, Gupta S, et al. Risk Reduction Compared with Access to Care: Quantifying the Trade-Off of Enforcing a Body Mass Index Eligibility Criterion for Joint Replacement. J Bone Joint Surg Am. 2018 Apr 4;100(7):539–545.
- Statz JM, Odum SM, Johnson NR, et al. Failure to Medically Optimize Before Total Hip Arthroplasty: Which Modifiable Risk Factor Is the Most Dangerous? Arthroplast Today. 2021 Aug;10:18–23.
- Haverkamp D, Klinkenbijl MN, Somford MP, et al. Obesity in total hip arthroplasty--does it really matter? A meta-analysis. Acta Orthop. 2011 Aug;82(4):417–422.
- Kerkhoffs GM, Servien E, Dunn W, et al. The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review. J Bone Joint Surg Am. 2012 Oct 17;94(20):1839–1844.
- Issa K, Pivec R, Kapadia BH, et al. Does obesity affect the outcomes of primary total knee arthroplasty? J Knee Surg. 2013 Apr;26(2):89–94.
- Roth A, Khlopas A, George J, et al. The Effect of Body Mass Index on 30-day Complications After Revision Total Hip and Knee Arthroplasty. J Arthroplasty. 2019 Jul;34(7s):S242–s248.
- Giesinger K, Giesinger JM, Hamilton DF, et al. Higher body mass index is associated with larger postoperative improvement in patient-reported outcomes following total knee arthroplasty. BMC Musculoskelet Disord. 2021 Jul 24;22(1):635.
- Baker P, Petheram T, Jameson S, et al. The association between body mass index and the outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2012 Aug 15;94(16):1501–1508.
- Lash H, Hooper G, Hooper N, et al. Should a Patients BMI Status be Used to Restrict Access to Total Hip and Knee Arthroplasty? Functional Outcomes of Arthroplasty Relative to BMI - Single Centre Retrospective Review. Open Orthop J. 2013;7:594–599.
- Elkins JM, Simoens KJ, Callaghan JJ. Lower Extremity Geometry in Morbid Obesity-Considerations for Total Knee Arthroplasty. J Arthroplasty. 2018 Oct;33(10):3304–3312.
- Armstrong JG, Morris TR, Sebro R, et al. Prospective Study of Central versus Peripheral Obesity in Total Knee Arthroplasty. Knee Surg Relat Res. 2018 Dec 1;30(4):319–325.