Patellar fractures after total knee arthroplasty
Preview
Etiology
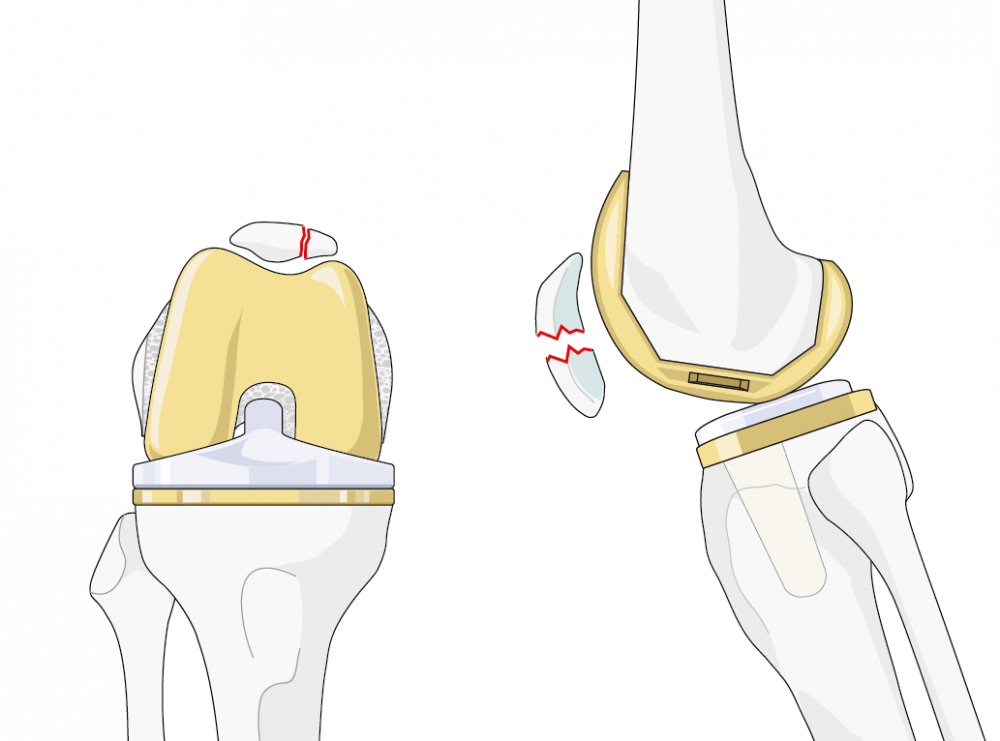
Patellar fractures (Figure 1) are one of the most common periprosthetic fractures [1]. Their incidence after primary TKA is overall approximately 1% [1, 2], but may be as high as 20% in certain patellar implants [3]. After revision surgery, incidences are roughly twice as high as after primary surgery [4].
Their etiology is multifactorial. In the minority of cases, the fractures are preceded by a traumatic event [2, 5, 6]. Often, they are asymptomatic [6, 7]. Usually, they emerge within 2 or 3 years after surgery [6, 8]. Broadly speaking, the risk factors can be categorized into patient-related, implant related, and technical.
Patient-related factors are primarily linked to bone quality, bone quantity, and loading of the implant. Besides the obvious osteoporosis and osteopenia linked to aging, they can also be induced by rheumatoid arthritis, which is thus an important risk factor [2]. This is particularly important in the presence of a very thin and eroded patella [9]. Moreover, prosthetic wear and loosening can lead to progressive osteolysis [8].
Did you know?
Most orthopedic and trauma surgeons are painfully aware of the poor bone quality they often find when operating on patients with rheumatoid arthritis. But why is this so? Clemens Gwinner, head of knee endoprosthetics at the university hospital Charité in Berlin, Germany, explains: “Rheumatoid arthritis is a systemic disease which causes joint inflammation. The inflammatory cytokine release is, amongst other effects, responsible for the increase in osteoclast activity, which ultimately leads to bone degradation.”

Clemens Gwinner
Charité—University Medicine Berlin
Berlin, Germany
Loading of the implant in the presence of correctly aligned components is mainly affected by the patient's weight, activity level [9, 10], and range of motion [11]. Of note, male sex has been identified as a risk factor for periprosthetic patellar fracture by some authors [6]. However, a likely explanation for this otherwise unexplained finding is the higher body weight and higher activity level usually found in men [6, 12]. A high degree of knee flexion has also been shown to be a risk factor [9]. The biomechanical mechanism is, that during active flexion, the stresses in the patellofemoral joint increase gradually as the knee bends. At 45–60° of flexion, the pressures on the proximal part of the patella are the highest. While deep active bending occurs less often with Western lifestyles, it is essential for activities of daily living in many Asian societies.
Read the full article with your AO login
- Implant-related factors
- Technical factors
- Management
- Indications for nonsurgical treatment
- Indications for surgery and surgical techniques
- Outcomes and conclusions
Additional AO resources on this topic
Access videos, tools, and other assets to learn more about this topic.
- Video: Extensor Mechanism Problems after Total Knee Arthroplasty
- Video: Managing Deformity in Total Knee Arthroplasty
- Video: The Difficult Primary Total Knee Arthroplasty
- Video: Tips and Tricks to Improve Total Knee Arthroplasty Outcomes
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Guillermo Bonilla
Fundación Santa Fe de Bogotá University Hospital
Bogotá, Colombia

Clemens Gwinner
Charité—University Medicine Berlin
Berlin, Germany

Yixin Zhou
Beijing Jishuitan Hospital
Beijing, China
This issue was written by Elke Rometsch, AO Innovation Translation Center, Clinical Science, Switzerland.
References
- Mulcahy H, Chew FS. Current concepts in knee replacement: complications. AJR Am J Roentgenol. 2014 Jan;202(1):W76–86.
- Chalidis BE, Tsiridis E, Tragas AA, et al. Management of periprosthetic patellar fractures. A systematic review of literature. Injury. 2007 Jun;38(6):714–724.
- Chan JY, Giori NJ. Uncemented Metal-Backed Tantalum Patellar Components in Total Knee Arthroplasty Have a High Fracture Rate at Midterm Follow-Up. J Arthroplasty. 2017 Aug;32(8):2427–2430.
- Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999 Apr;30(2):183–190.
- Assiotis A, To K, Morgan-Jones R, et al. Patellar complications following total knee arthroplasty: a review of the current literature. Eur J Orthop Surg Traumatol. 2019 Dec;29(8):1605–1615.
- Ortiguera CJ, Berry DJ. Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am. 2002 Apr;84(4):532–540.
- Bourne RB. Fractures of the patella after total knee replacement. Orthop Clin North Am. 1999 Apr;30(2):287–291.
- Roth A, Ghanem M, Fakler J. [Patella fractures in knee arthroplasty]. Orthopade. 2016 May;45(5):416–424.
- Parvizi J, Kim KI, Oliashirazi A, et al. Periprosthetic patellar fractures. Clin Orthop Relat Res. 2006 May;446:161–166.
- Papalia R, Vasta S, D'Adamio S, et al. Complications involving the extensor mechanism after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015 Dec;23(12):3501–3515.
- Insall JN, Lachiewicz PF, Burstein AH. The posterior stabilized condylar prosthesis: a modification of the total condylar design. Two to four-year clinical experience. J Bone Joint Surg Am. 1982 Dec;64(9):1317–1323.
- Tharani R, Nakasone C, Vince KG. Periprosthetic fractures after total knee arthroplasty. J Arthroplasty. 2005 Jun;20(4 Suppl 2):27–32.
- Healy WL, Wasilewski SA, Takei R, et al. Patellofemoral complications following total knee arthroplasty. Correlation with implant design and patient risk factors. J Arthroplasty. 1995 Apr;10(2):197–201.
- Sheth NP, Pedowitz DI, Lonner JH. Periprosthetic patellar fractures. J Bone Joint Surg Am. 2007 Oct;89(10):2285–2296.
- Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984 Jun;66(5):715–724.
- Mouton J, Gaillard R, Bankhead C, et al. Increased Patellar Fracture Rate in Total Knee Arthroplasty With Preoperative Varus Greater Than 15°: A Case-Control Study. J Arthroplasty. 2018 Dec;33(12):3685–3693.
- Goldberg VM, Figgie HE, 3rd, Inglis AE, et al. Patellar fracture type and prognosis in condylar total knee arthroplasty. Clin Orthop Relat Res. 1988 Nov(236):115–122.
- Rorabeck CH, Angliss RD, Lewis PL. Fractures of the femur, tibia, and patella after total knee arthroplasty: decision making and principles of management. Instr Course Lect. 1998;47:449–458.
- Sarmah SS, Patel S, Reading G, et al. Periprosthetic fractures around total knee arthroplasty. Ann R Coll Surg Engl. 2012 Jul;94(5):302–307.
- Windsor RE, Scuderi GR, Insall JN. Patellar fractures in total knee arthroplasty. J Arthroplasty. 1989;4 Suppl:S63–67.
- Laskin RS. Management of the patella during revision total knee replacement arthroplasty. Orthop Clin North Am. 1998 Apr;29(2):355–360.
- Keating EM, Haas G, Meding JB. Patella fracture after post total knee replacements. Clin Orthop Relat Res. 2003 Nov(416):93–97.
- Insall JN, Dorr LD, Scott RD, et al. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989 Nov(248):13–14.
- Hozack WJ, Goll SR, Lotke PA, et al. The treatment of patellar fractures after total knee arthroplasty. Clin Orthop Relat Res. 1988 Nov(236):123–127.
- Dennis DA. Periprosthetic fractures following total knee arthroplasty. Instr Course Lect. 2001;50:379–389.