Spinopelvic mechanics and dislocation risk
Preview
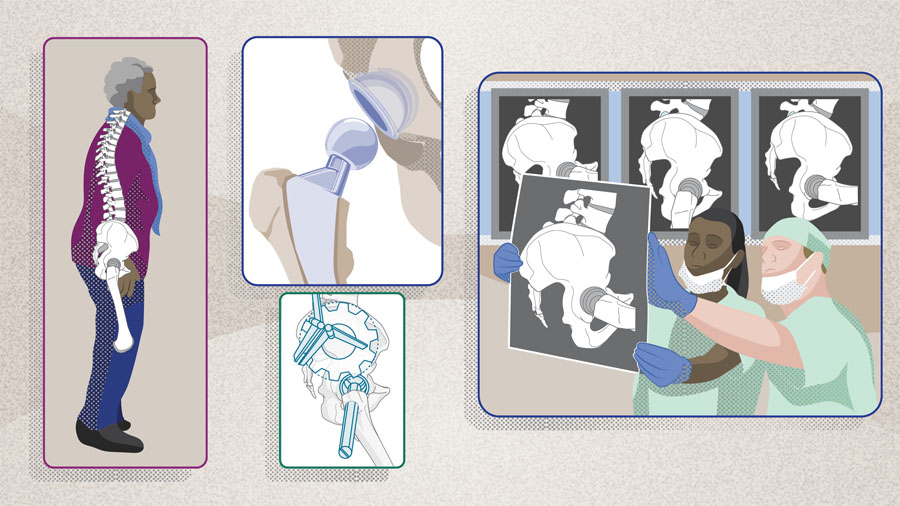
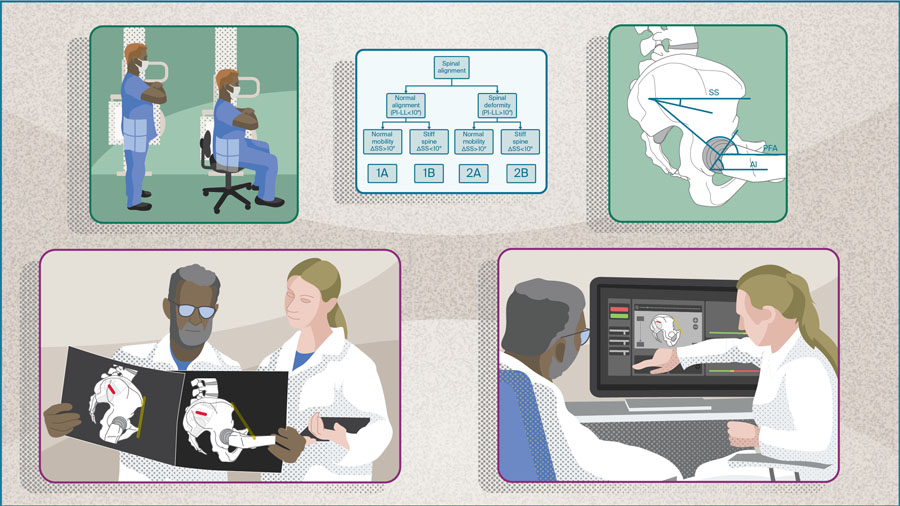
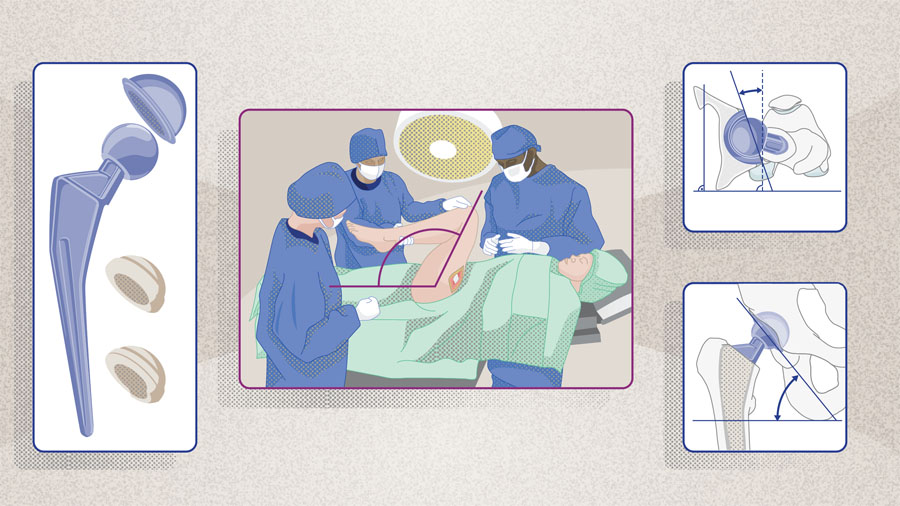
Postoperative dislocation remains a significant complication following total hip arthroplasty (THA), with growing evidence highlighting the critical role of spinopelvic mechanics in implant stability. Abnormal spinopelvic alignment and mobility—whether due to spinal stiffness or hypermobility—can result in compensatory mechanics that place the hip at greater risk of instability, particularly during postural changes.
In Part 1 of our three-part series, Nathanael D Heckmann from the Keck Medical Centre of the University of Southern California, Los Angeles, California, United States, explores the evolving epidemiology of hip instability, with a particular focus on the often-overlooked issue of late dislocations. He also discusses strategies for identifying at-risk patients, and highlights approaches to ultimately reduce dislocation rates in the short and long-term.

Nathanael D Heckmann
Keck Medical Centre, University of Southern California, Los Angeles, California, United States
Risk factors and common complications following total hip arthroplasty
Total hip arthroplasty (THA) ranks among the most effective interventions in orthopedic and trauma surgery [1]. For patients with hip osteoarthritis, it offers significant pain relief, improved quality of life, and increased mobility in both the medium and long term [2]. However, despite improvements in surgical methods and prosthetic technology, postoperative complications remain a challenge for patients and surgeons alike [3].
Common complications following primary THA include aseptic loosening, dislocation, prosthetic joint infection, periprosthetic fracture, wound complications, and adverse reaction to metal debris [4]. Among these, dislocation—defined as the complete loss of articular contact between the femoral head and the acetabular cup—remains one of the most frequent complications and is a leading cause of revision surgery in the United States [3, 5].
The etiology of hip instability is multifactorial. Procedure- and implant-related factors such as hospital and surgeon case volume, surgical approach, and implant components have all been shown to influence the risk of dislocation [6–8]. Several patient-related factors have also been associated with increased risk, including age, sex, body mass index (BMI), underlying indications for THA such as inflammatory conditions and developmental dysplasia of the hip (DDH), history of prior hip surgery, and coexisting medical conditions such as neurological or neuromuscular disorders, as well as previous spinal surgery or spinal disease [9].
Read the full article with your AO login
- Risk factors and complications after THA
- Spinopelvic biomechanics and THA
- Spinopelvic mechanics, compensation patterns
- Postoperative late dislocation in THA
- Lateral imaging to identify high-risk patients
- Conclusion
AO Recon resources
Contributing experts

George Grammatopoulos
The Ottawa Hospital, University of Ottawa, Ottawa, Ontario, Canada

Nathanael D Heckmann
Keck Medical Centre, University of Southern California, Los Angeles, California, United States

Jonathan M Vigdorchik
Hospital for Special Surgery, New York, New York, United States
This article was written by Chiara Cianciolo, AO Innovation Translation Center, Clinical Evidence, Switzerland.
References
-
Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. The Lancet. 2007;370(9597):1508–1519.
-
Mariconda M, Galasso O, Costa GG, et al. Quality of life and functionality after total hip arthroplasty: a long-term follow-up study. BMC Musculoskelet Disord. 2011 Oct 6;12:222.
-
Bozic KJ, Kurtz SM, Lau E, et al. The Epidemiology of Revision Total Hip Arthroplasty in the United States. JBJS. 2009;91(1):128–133.
-
Taljanovic MS, Jones MD, Hunter TB, et al. Joint arthroplasties and prostheses. Radiographics. 2003 Sep-Oct;23(5):1295-1314.
-
Gwam CU, Mistry JB, Mohamed NS, et al. Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J Arthroplasty. 2017 Jul;32(7):2088–2092.
-
Kishimoto Y, Kato Y, Kishi T, et al. Dislocation is a Leading Cause of Decreased Survival Rate in Primary Total Hip Arthroplasty Performed by Low-Volume Surgeons: Long-Term Retrospective Cohort Study. J Arthroplasty. 2020 Nov;35(11):3237–3241.
-
Dargel J, Oppermann J, Brüggemann GP, Eysel P. Dislocation following total hip replacement. Dtsch Arztebl Int. 2014 Dec 22;111(51-52):884–890.
-
Brooks PJ. Dislocation following total hip replacement: causes and cures. Bone Joint J. 2013 Nov;95-b(11 Suppl A):67–69.
-
Wyles CC, Maradit-Kremers H, Larson DR, et al. Creation of a Total Hip Arthroplasty Patient-Specific Dislocation Risk Calculator. J Bone Joint Surg Am. 2022 Jun 15;104(12):1068–1080.
-
Esposito CI, Carroll KM, Sculco PK, et al. Total Hip Arthroplasty Patients With Fixed Spinopelvic Alignment Are at Higher Risk of Hip Dislocation. J Arthroplasty. 2018 May;33(5):1449–1454.
-
Heckmann N, McKnight B, Stefl M, et al. Late Dislocation Following Total Hip Arthroplasty: Spinopelvic Imbalance as a Causative Factor. J Bone Joint Surg Am. 2018 Nov 7;100(21):1845–1853.
-
Heckmann ND, Lieberman JR. Spinopelvic Biomechanics and Total Hip Arthroplasty: A Primer for Clinical Practice. J Am Acad Orthop Surg. 2021 Sep 15;29(18):e888–e903.
-
Abdel MP, von Roth P, Jennings MT, et al. What Safe Zone? The Vast Majority of Dislocated THAs Are Within the Lewinnek Safe Zone for Acetabular Component Position. Clin Orthop Relat Res. 2016 Feb;474(2):386–391.
-
Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978 Mar;60(2):217–220.
-
Esposito CI, Gladnick BP, Lee YY, et al. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty. 2015 Jan;30(1):109–113.
-
Vigdorchik J, Eftekhary N, Elbuluk A, et al. Evaluation of the spine is critical in the workup of recurrent instability after total hip arthroplasty. Bone Joint J. 2019 Jul;101-b(7):817–823.
-
Gausden EB, Parhar HS, Popper JE, et al. Risk Factors for Early Dislocation Following Primary Elective Total Hip Arthroplasty. J Arthroplasty. 2018 May;33(5):1567–1571.e1562.
-
Behery OA, Vasquez-Montes D, Cizmic Z, et al. Can Flexed-Seated and Single-Leg Standing Radiographs Be Useful in Preoperative Evaluation of Lumbar Mobility in Total Hip Arthroplasty? J Arthroplasty. 2020 Aug;35(8):2124–2130.
-
Berliner JL, Esposito CI, Miller TT, et al. What preoperative factors predict postoperative sitting pelvic position one year following total hip arthroplasty? Bone Joint J. 2018 Oct;100-b(10):1289–1296.
-
Sculco PK, Windsor EN, Jerabek SA, et al. Preoperative spinopelvic hypermobility resolves following total hip arthroplasty. Bone Joint J. 2021 Dec;103-b(12):1766–1773.
-
Mills ES, Wang JC, Sanchez J, et al. The Correlation Between Pelvic Motion and Lumbar Motion in Patients Presenting With a Lumbar Spinal Pathology: Implications for Assessing Dislocation Risk in Total Hip Arthroplasty. Arthroplast Today. 2023 Apr;20:101105.
-
Sharma AK, Grammatopoulos G, Pierrepont JW, et al. Sacral Slope Change From Standing to Relaxed-Seated Grossly Overpredicts the Presence of a Stiff Spine. J Arthroplasty. 2023 Apr;38(4):713-718.e711.
-
Heckmann ND, Chung BC, Wier JR, et al. The Effect of Hip Offset and Spinopelvic Abnormalities on the Risk of Dislocation Following Total Hip Arthroplasty. J Arthroplasty. 2022 Jul;37(7s):S546–s551.
-
Buckland AJ, Puvanesarajah V, Vigdorchik J, et al. Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Joint J. 2017 May;99-b(5):585–591.
-
Innmann MM, Verhaegen JCF, Reichel F, et al. Spinopelvic Characteristics Normalize 1 Year After Total Hip Arthroplasty: A Prospective, Longitudinal, Case-Controlled Study. J Bone Joint Surg Am. 2022 Apr 20;104(8):675–683.
-
Vigdorchik JM, Shafi KA, Kolin DA, et al. Does Low Back Pain Improve Following Total Hip Arthroplasty? The Journal of arthroplasty. 2022 2022/08//;37(8S):S937–S940.
-
Mills ES, Bouz GJ, Kang HP, et al. Preoperative radiographic findings associated with postoperative spinopelvic risk factors for instability following total hip arthroplasty. J Orthop Res. 2023 Sep;41(9):2026–2031.
-
Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982 Dec;64(9):1295–1306.
-
Ali Khan MA, Brakenbury PH, Reynolds IS. Dislocation following total hip replacement. J Bone Joint Surg Br. 1981;63-b(2):214–218.
-
Pulido L, Restrepo C, Parvizi J. Late instability following total hip arthroplasty. Clin Med Res. 2007 Jun;5(2):139–142.
-
von Knoch M, Berry DJ, Harmsen WS, Morrey BF. Late dislocation after total hip arthroplasty. J Bone Joint Surg Am. 2002 Nov;84(11):1949–1953.
-
Meek RM, Allan DB, McPhillips G, et al. Late dislocation after total hip arthroplasty. Clin Med Res. 2008 May;6(1):17–23.
-
Berry DJ, von Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004 Jan;86(1):9–14.
-
Itokawa T, Nakashima Y, Yamamoto T, et al. Late dislocation is associated with recurrence after total hip arthroplasty. Int Orthop. 2013 Aug;37(8):1457–1463.
-
Brennan SA, Khan F, Kiernan C, et al. Dislocation of primary total hip arthroplasty and the risk of redislocation. Hip Int. 2012 Sep-Oct;22(5):500–504.
-
Langston J, Pierrepont J, Gu Y, Shimmin A. Risk factors for increased sagittal pelvic motion causing unfavourable orientation of the acetabular component in patients undergoing total hip arthroplasty. Bone Joint J. 2018 Jul;100-b(7):845–852.
-
Grammatopoulos G, Falsetto A, Sanders E, et al. Integrating the Combined Sagittal Index Reduces the Risk of Dislocation Following Total Hip Replacement. J Bone Joint Surg Am. 2022 Mar 2;104(5):397–411.
-
Heckmann ND, Plaskos C, Wakelin EA, et al. Excessive posterior pelvic tilt from preoperative supine to postoperative standing after total hip arthroplasty. Bone Joint J. 2024 Mar 1;106-b(3 Supple A):74–80.