Managing bone defects using large acetabular cups and highly porous augments
Preview
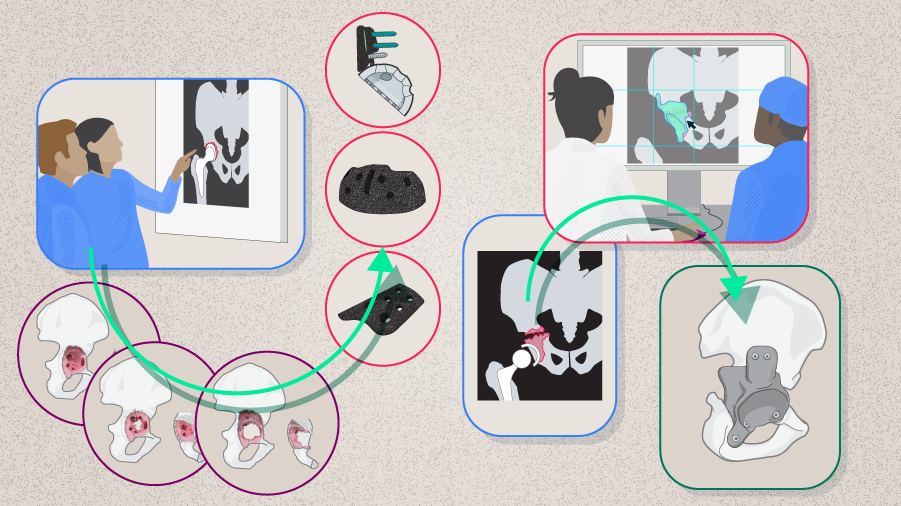
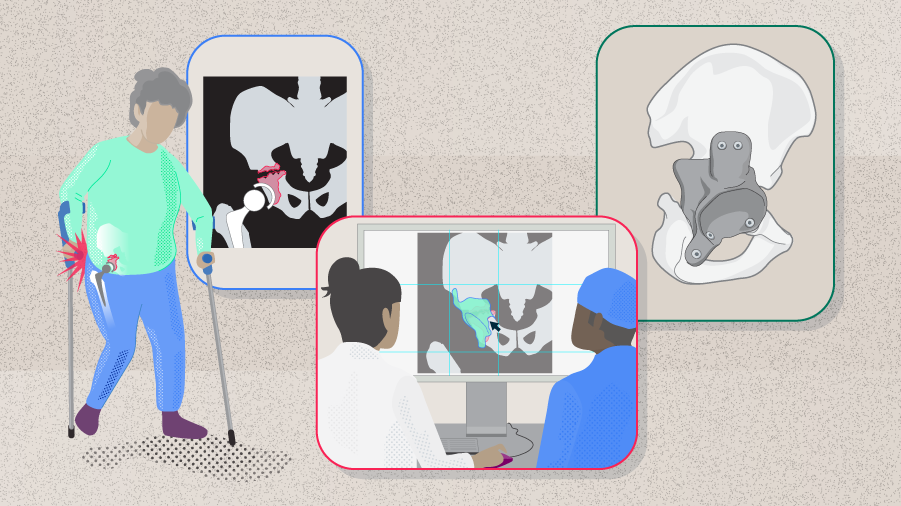
Revision total hip arthroplasty (rTHA) is a difficult surgical procedure. The key challenge of this procedure is the potentially significant bone loss and the often encountered poor bone quality. Although much advancement in surgical techniques, technologies, and materials has been made in recent years and has helped improve the treatment of complex acetabular defects, several topics remain controversial, and a systematic incorporation of the technical advancement into treatment paradigms is still needed [1]. In this article, George A Macheras, Head of the Orthopedic Department in the Henry Dunant Medical Center, Athens, Greece, shares his experience and his strategies in managing acetabular bone defects. Examples of how cases of severe bone loss were managed using advanced techniques are also presented.

George A Macheras
Henry Dunant Medical Center, Athens, Greece
The Paprosky Classification
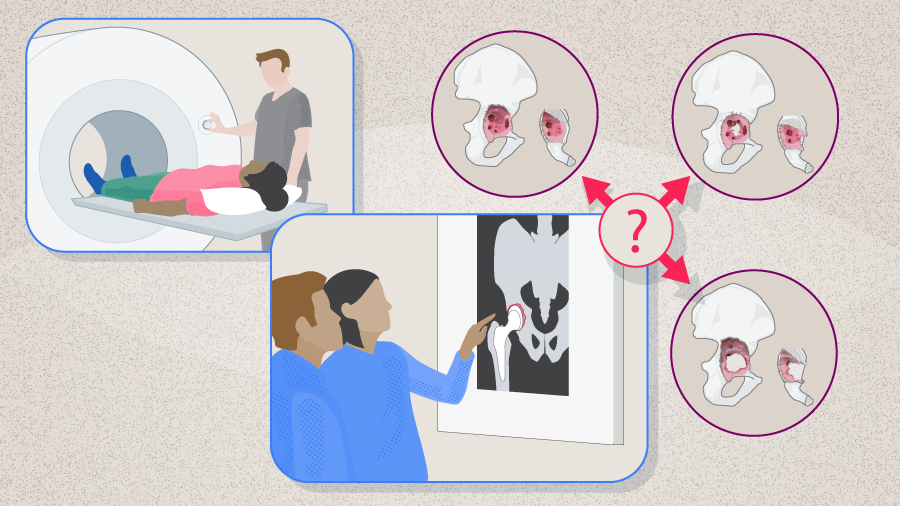
To perform a successful rTHA, it is crucial to accurately assess the severity and the pattern of bone loss so as to predict the ability of the remaining host bone to support the implants and maximize the amount of initial stability until bone ingrowth can occur [2]. The goal of an optimal solution is to restore hip biomechanics and achieve rigid fixation for long-term results.
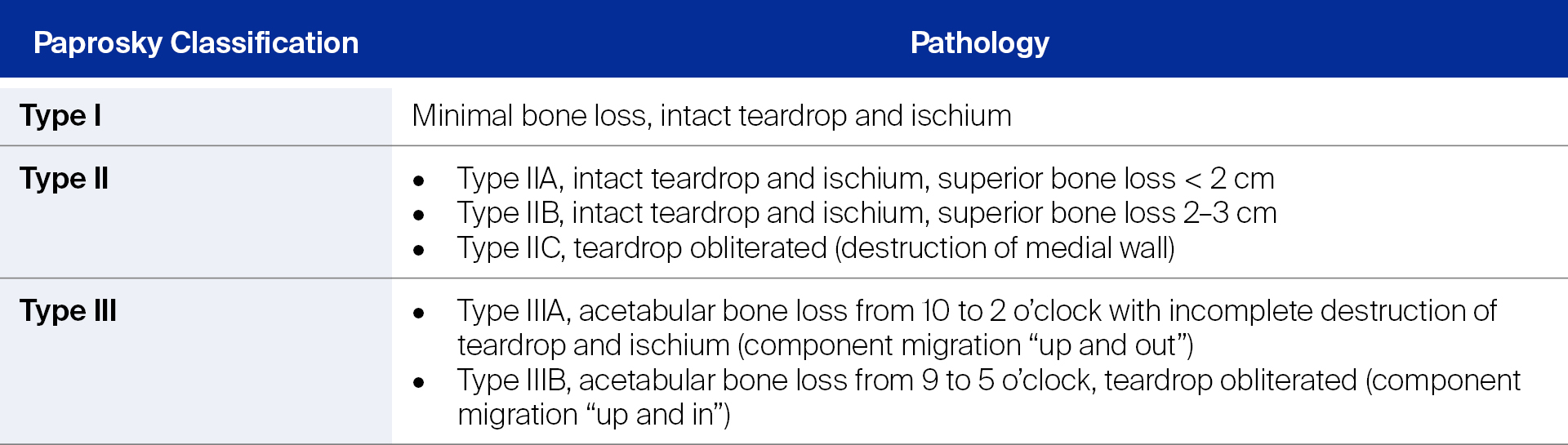
As has been addressed in Part 1, among the various classification systems, the Paprosky Classification has demonstrated good validity and moderate reliability. When a surgeon is trained in this system, it can provide good reliability [3]. It is also the most clinically oriented because it assesses both the amount of acetabular bone loss and the ability of the remaining host bone to support the initial stability of the acetabular components [4]. In case of severe bone loss, the Paprosky Classification is a particularly useful treatment guide [1, 5].
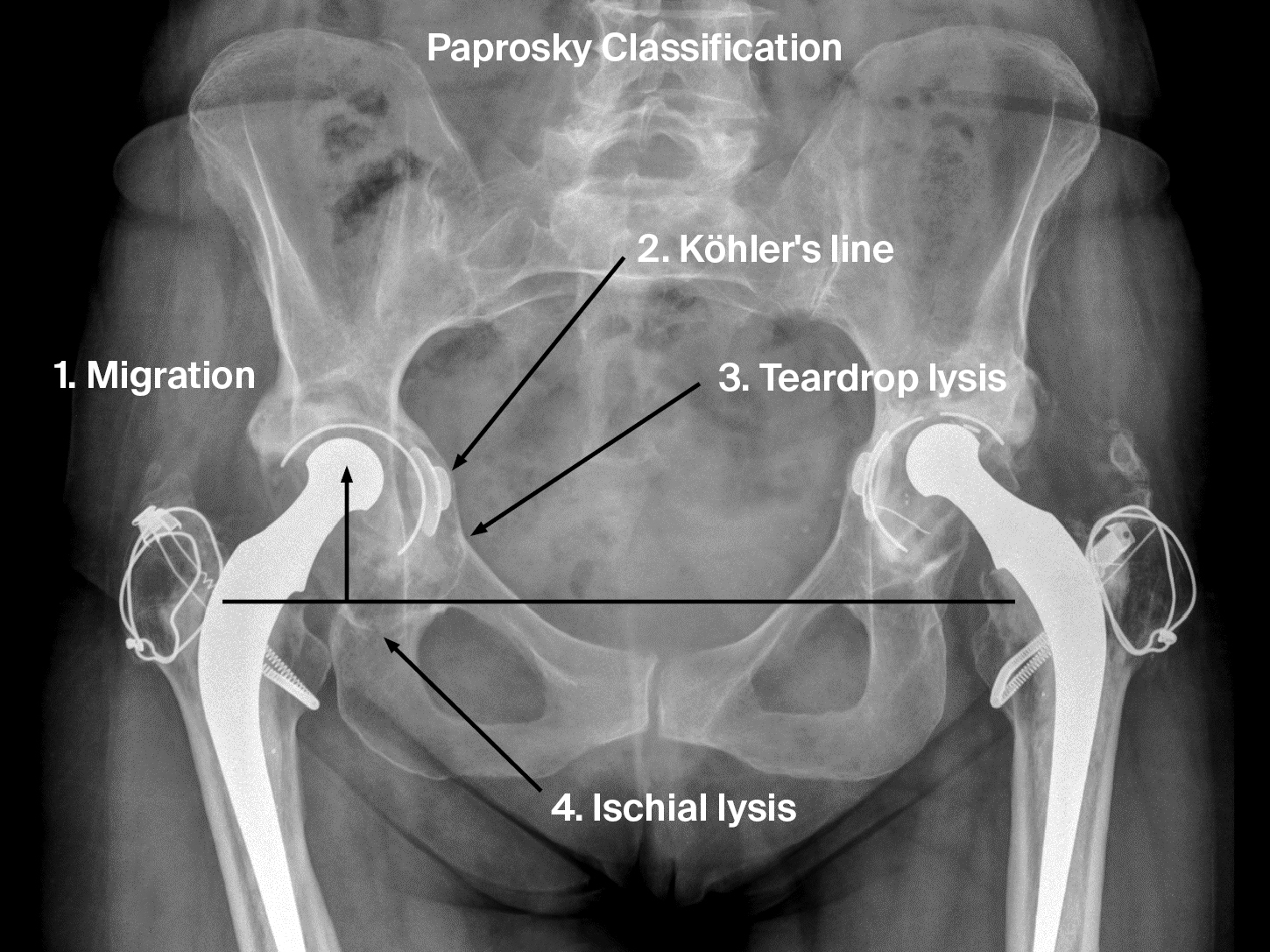
Four radiographic features are important in determining the Paprosky types, ie, the teardrop, ischium, Köhler’s line, and superior migration (Figure 1). These four features indicate the integrity of the medial wall (teardrop), posterior column (ischium), anterior column (Köhler’s line), and superior dome (superior migration of the hip center) [6]. The criteria for the Paprosky Classification are summarized in Table 1 [4].
Ask the expert
We asked George Macheras how accurate a preoperative assessment of bone loss is in general. He told us that, intraoperatively, one should always be ready to encounter greater bone loss than predicted by the preoperative assessment. A meticulous debridement that rids the acetabulum of necrotic bone and scar tissue is pivotal, which should be followed by reaming the defects until bleeding healthy bone. Only then can the true bone loss be evaluated. For this reason, one should always have more than one reconstruction option available at the time of surgery.Some general principles in treating acetabular bone loss are presented below.
Read the full article with your AO login
- The Paprosky Classification
- Did you know?
- Modern advancement to enhance biological fixation
- Jumbo cups
- Highly porous metal augments
- Type I defects
- Principles in`Paprosky type II management
- Type IIA defects
- Type IIB defects
- Type IIC defects
- Principles in Paprosky type III management
- Type IIIA defects
- Type IIIB defects
- Conclusion
AO Recon resources
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Theofilos Karachalios
University General Hospital of Larissa at the University of Thessaly, Larissa, Greece

Thomas Kostakos
Henry Dunant Medical Center, Athens, Greece

George A Macheras
Henry Dunant Medical Center, Athens, Greece
The authors thank Maio Chen, medical writer at AO Innovation Translation Center, Switzerland, for contributing to the writing and editing of the articles.
References
- Sculco PK, Wright T, Malahias MA, et al. The Diagnosis and Treatment of Acetabular Bone Loss in Revision Hip Arthroplasty: An International Consensus Symposium. HSS J. 2022 Feb;18(1):8–41.
- Sporer SM, Paprosky WG, O'Rourke M. Managing Bone Loss in Acetabular Revision. JBJS. 2005;87(7):1620–1630.
- Yu R, Hofstaetter JG, Sullivan T, et al. Validity and reliability of the Paprosky acetabular defect classification. Clin Orthop Relat Res. 2013 Jul;471(7):2259–2265.
- Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994 Feb;9(1):33–44.
- Sporer SM, O'Rourke M, Paprosky WG. The treatment of pelvic discontinuity during acetabular revision. J Arthroplasty. 2005 Jun;20(4 Suppl 2):79–84.
- Mancino F, Cacciola G, Di Matteo V, et al. Reconstruction options and outcomes for acetabular bone loss in revision hip arthroplasty. Orthop Rev (Pavia). 2020 Jun 29;12(Suppl 1):8655.
- Bobyn JD, Stackpool GJ, Hacking SA, et al. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999 Sep;81(5):907–914.
- Whitehouse MR, Masri BA, Duncan CP, Garbuz DS. Continued Good Results With Modular Trabecular Metal Augments for Acetabular Defects in Hip Arthroplasty at 7 to 11 Years. 2015;473(2):521–527.
- Russell SP, O'Neill CJ, Fahey EJ, et al. Trabecular Metal Augments for Severe Acetabular Defects in Revision Hip Arthroplasty: A Long-Term Follow-Up. The Journal of Arthroplasty. 2021 2021/05/01/;36(5):1740–1745.
- Xiong C, Meng D, Ni R, Cai H. Metal Augments Used in Revision Hip Arthroplasty: A Systematic Review and Single-Arm Meta-Analysis. The Journal of Arthroplasty. 2023;38(2):389–396.e381.
- Wang Q, Wang Q, Liu P, et al. Clinical and radiological outcomes of jumbo cup in revision total hip arthroplasty: A systematic review. Front Surg. 2022;9:929103.
- Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. 2001 Sep;83(9):1352–1357.
- Nwankwo CD, Ries MD. Do jumbo cups cause hip center elevation in revision THA? A radiographic evaluation. Clin Orthop Relat Res. 2014 Sep;472(9):2793–2798.
- Nam HJ, Lim YW, Jo WL, et al. Is the construct stability of the acetabular cup affected by the acetabular screw configuration in bone defect models? J Orthop Surg Res. 2023 May 12;18(1):354.
- Jvon Roth P, Abdel MP, Harmsen WS, Berry DJ. Uncemented jumbo cups for revision total hip arthroplasty: a concise follow-up, at a mean of twenty years, of a previous report. Bone Joint Surg Am. 2015 Feb 18;97(4):284–287.
- Meneghini RM, Meyer C, Buckley CA, et al. Mechanical stability of novel highly porous metal acetabular components in revision total hip arthroplasty. J Arthroplasty. 2010 Apr;25(3):337–341.
- Ahmad AQ, Schwarzkopf R. Clinical evaluation and surgical options in acetabular reconstruction: A literature review. J Orthop. 2015 Dec;12(Suppl 2):S238–243.