Osteotomy prior to total knee arthroplasty: optimizing limb alignment
Preview
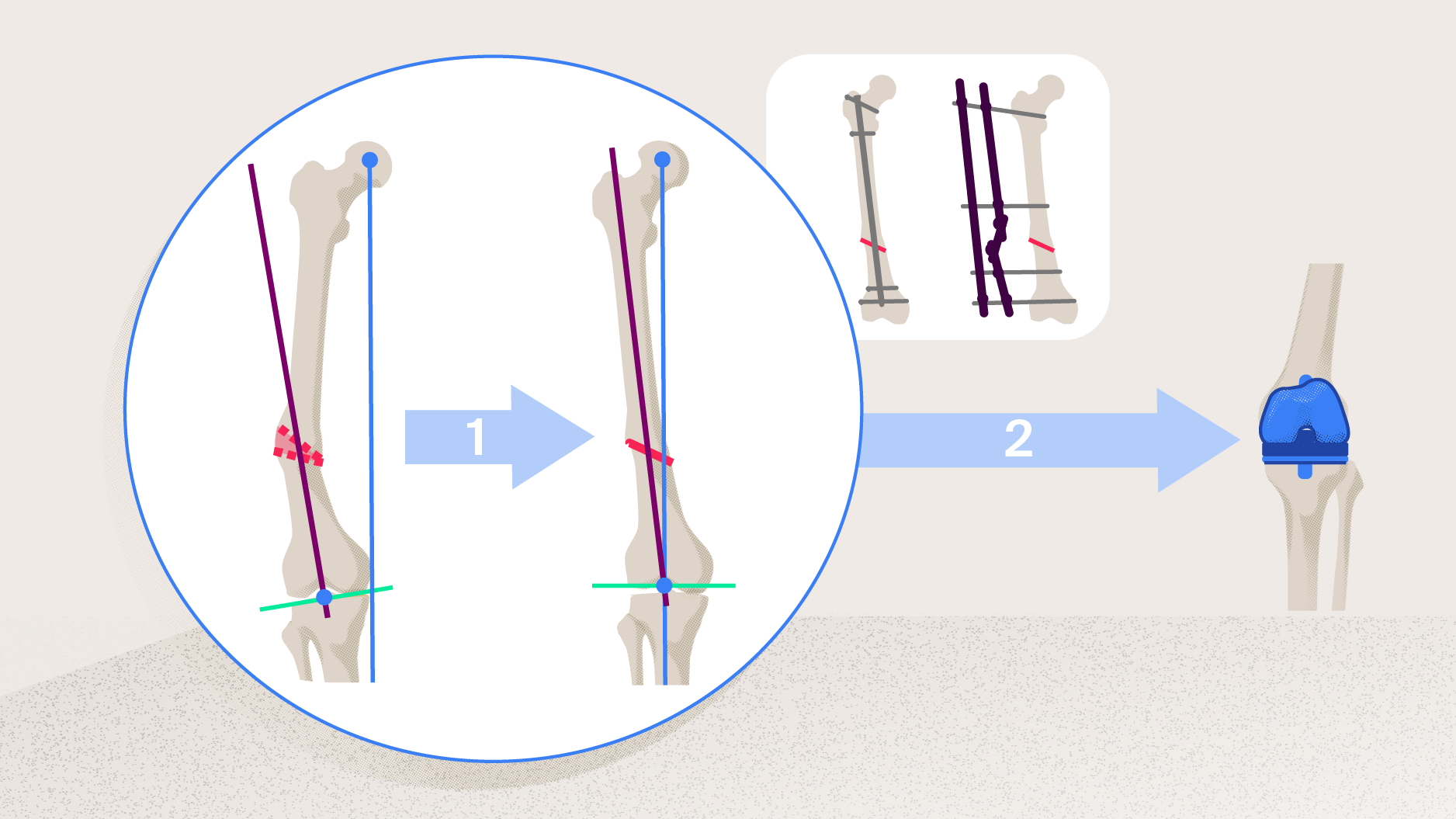
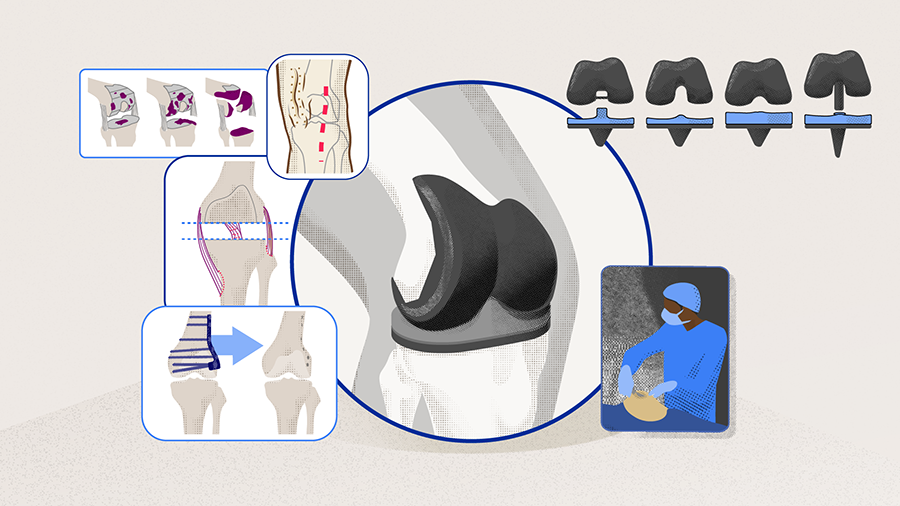
Posttraumatic osteoarthritis (PTOA) of the knee often occurs following fractures of the proximal tibia, patella, and distal femur. Nonunion or malunion of tibial or femoral fractures can translate into extraarticular deformities, which can cause a mechanical axis deviation followed by abnormal mechanical forces on the articular surfaces. Not the malunion itself, but the severity of the deformity is usually the most important determinant of overall knee function and progression of PTOA. Many surgeons attempt to correct malalignment of the lower extremity during the knee replacement surgery. This, however, is successful only when the deformity is intraarticular in origin. Correcting an extraarticular deformity through total knee arthroplasty (TKA) often results in a compromised knee, in which the deformity is not entirely corrected and the prothesis is not perfectly aligned. Therefore, a staged osteotomy prior to knee reconstruction can be the solution, as it restores limb alignment and in turn, increases the longevity of the implant. In this article, Austin T. Fragomen, Professor of Clinical Orthopaedic Surgery at New York's Special Surgery Hospital, shares some general principles of restoring lower limb alignment issues by staged osteotomies in the setting of TKA, with a particular focus on extraarticular deformities.
Austin T Fragomen
Hospital for Special Surgery
New York, USA
Mapping extraarticular deformities: origin, location, and direction
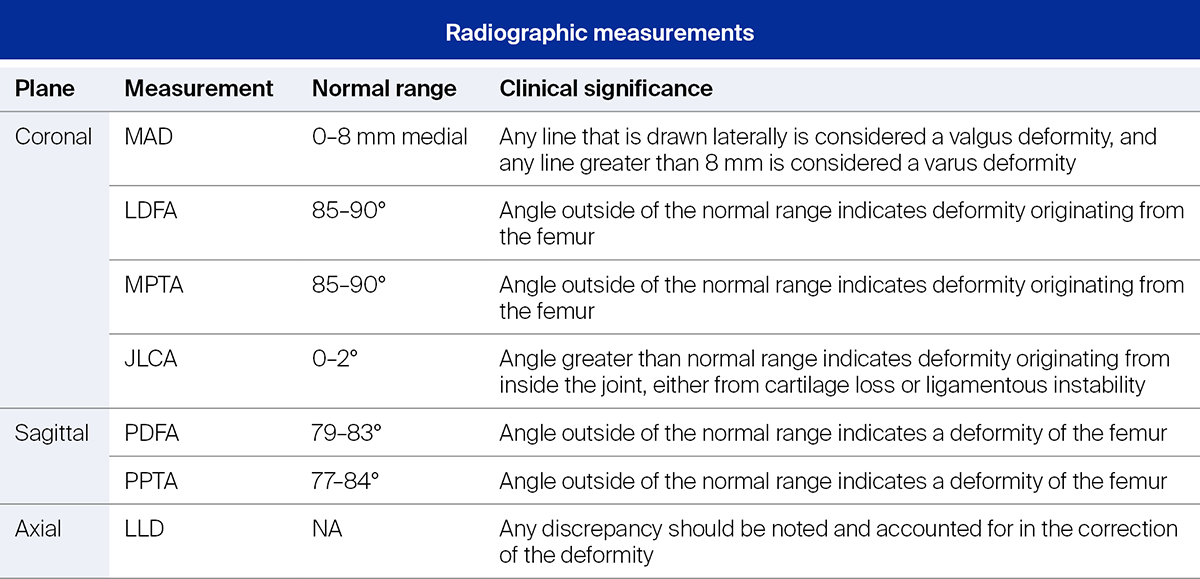
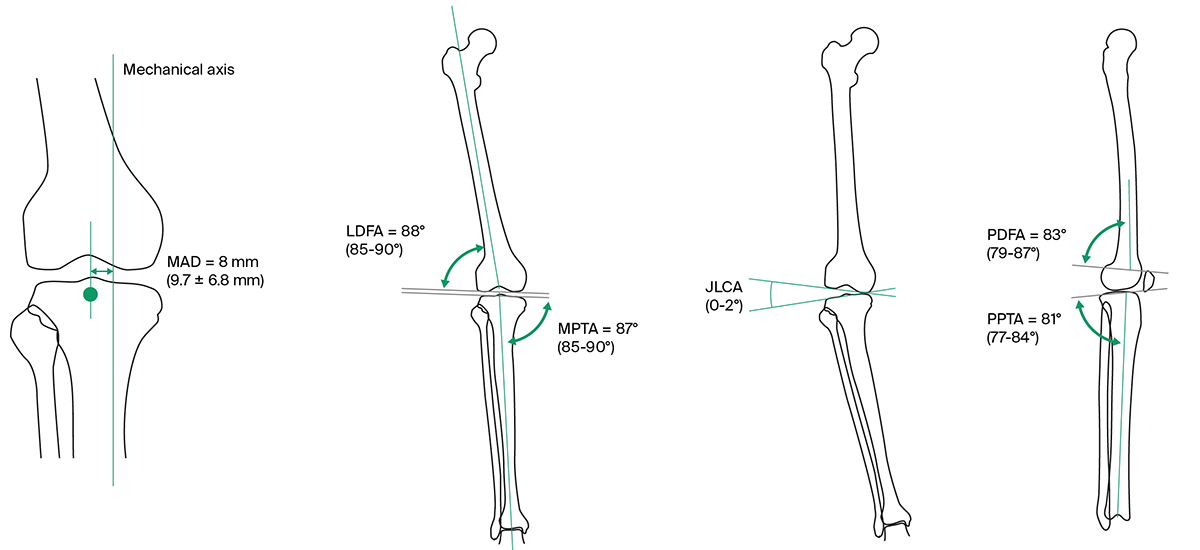
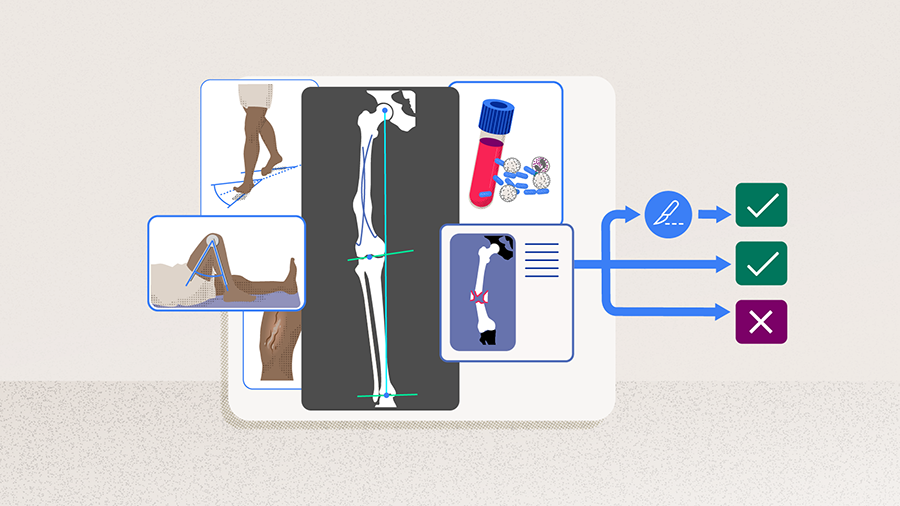
Imaging evaluation of patients showing extraarticular malignments is invaluable and should include long leg hip-to-ankle x-rays in the AP and lateral planes. To evaluate the location and extent of deformity, several preoperative measurements must be performed in the coronal, sagittal, and axial planes (Table 1 and Figure 1). In the coronal plane, measuring mechanical axis deviation (MAD) will indicate whether the deformity is a valgus or varus [1]. Analysis of the lateral distal femoral angle (LDFA), medial proximal tibial angle (MPTA), and joint line convergence angle (JLCA) allows the surgeon to trace back the origin of the deformity to the tibia, femur, or inside the joint. Similarly, examination of the posterior distal femoral angle (PDFA) and posterior proximal tibial angle (PPTA) provides the surgeon with information about the degree of the deformity in the sagittal plane [1]. A key measurement is determining the center of rotation of angulation (CORA), which is the location where the anatomical axes of the bone proximal and distal to the deformity meet (Figure 1). CORA determines whether a deformity can be successfully corrected through a knee replacement, as the deformity location directly correlates with its impact on limb alignment. As demonstrated by Wolff et al [2], the closer to the knee the deformity is, the greater its effect in overall mechanical alignment is. CORA measurements are used to determine osteotomy planning.
Read the full article with your AO login
- Surgical techniques for corrective osteotomies: which one to choose?
- Preoperative planning for corrective osteotomies and TKA
- Extraarticular osteotomies and TKA: one- or two-stage procedure?
- Internal fixation: intramedullary nailing and plate fixation
- External fixation
- Limb deformity correction after TKA: making a fresh start
- Conclusions
Additional AO resources
Access videos, tools, and other assets.
- Videos
- Books in Thieme store
- AO Surgery Reference
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Friedrich Boettner
Hospital for Special Surgery
New York, USA

Brian P Chalmers
Hospital for Special Surgery
New York, USA
Austin T Fragomen
Hospital for Special Surgery
New York, USA
The authors thank Antia Rodriguez-Villalon and Laura Kehoe, medical writers at AO Innovation Translation Center, Switzerland, for contributing to the writing and editing of the articles.
References
- Sculco PK, Kahlenberg CA, Fragomen AT, et al. Management of Extra-articular Deformity in the Setting of Total Knee Arthroplasty. J Am Acad Orthop Surg. 2019 Sep 15;27(18):e819–e830.
- Wolff AM, Hungerford DS, Pepe CL. The effect of extraarticular varus and valgus deformity on total knee arthroplasty. Clin Orthop Relat Res. 1991 Oct(271):35–51.
- Paley D, Pfeil J. [Principles of deformity correction around the knee]. Orthopade. 2000 Jan;29(1):18–38.
- Gao L, Madry H, Chugaev DV, et al. Advances in modern osteotomies around the knee : Report on the Association of Sports Traumatology, Arthroscopy, Orthopaedic surgery, Rehabilitation (ASTAOR) Moscow International Osteotomy Congress 2017. J Exp Orthop. 2019 Feb 25;6(1):9.
- Parvizi J, Hanssen AD, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Joint Surg Am. 2004 Mar;86(3):474–479.
- Ekhtiari S, Haldane CE, de Sa D, et al. Return to Work and Sport Following High Tibial Osteotomy: A Systematic Review. J Bone Joint Surg Am. 2016 Sep 21;98(18):1568–1577.
- Watanabe Y, Takenaka N, Kinugasa K, et al. Intra- and Extra-Articular Deformity of Lower Limb: Tibial Condylar Valgus Osteotomy (TCVO) and Distal Tibial Oblique Osteotomy (DTOO) for Reconstruction of Joint Congruency. Adv Orthop. 2019;2019:8605674.
- Duivenvoorden T, Brouwer RW, Baan A, et al. Comparison of closing-wedge and opening-wedge high tibial osteotomy for medial compartment osteoarthritis of the knee: a randomized controlled trial with a six-year follow-up. J Bone Joint Surg Am. 2014 Sep 3;96(17):1425–1432.
- Puddu G, Cipolla M, Cerullo G, et al. Which osteotomy for a valgus knee? Int Orthop. 2010 Feb;34(2):239–247.
- Magnussen RA, Lustig S, Demey G, et al. The effect of medial opening and lateral closing high tibial osteotomy on leg length. Am J Sports Med. 2011 Sep;39(9):1900–1905.
- Puddu G, Cipolla M, Cerullo G, et al. Osteotomies: the surgical treatment of the valgus knee. Sports Med Arthrosc Rev. 2007 Mar;15(1):15–22.
- Wylie JD, Jones DL, Hartley MK, et al. Distal Femoral Osteotomy for the Valgus Knee: Medial Closing Wedge Versus Lateral Opening Wedge: A Systematic Review. Arthroscopy. 2016 Oct;32(10):2141–2147.
- Kim YC, Yang JH, Kim HJ, et al. Distal Femoral Varus Osteotomy for Valgus Arthritis of the Knees: Systematic Review of Open versus Closed Wedge Osteotomy. Knee Surg Relat Res. 2018 Mar 1;30(1):3–16.
- Catonne Y, Khiami F, Sariali E, et al. Same-stage total knee arthroplasty and osteotomy for osteoarthritis with extra-articular deformity. Part II: Femoral osteotomy, prospective study of 6 cases. Orthop Traumatol Surg Res. 2019 Oct;105(6):1055–1060.
- Catonne Y, Sariali E, Khiami F, et al. Same-stage total knee arthroplasty and osteotomy for osteoarthritis with extra-articular deformity. Part I: Tibial osteotomy, prospective study of 26 cases. Orthop Traumatol Surg Res. 2019 Oct;105(6):1047–1054.
- de Pablos Fernández J, Arbeloa-Gutierrez L, Arenas-Miquelez A. One-Stage Total Knee Arthroplasty Plus Corrective Osteotomy for Osteoarthritis Associated With Severe Extra-articular Deformity. Arthrosc Tech. 2019 Nov;8(11):e1403–e1410.
- Sponer P, Kucera T. Total knee arthroplasty associated with tibial tubercle and simultaneous femoral and tibial osteotomies for severe extra-articular deformity: a case report. Ther Clin Risk Manag. 2019;15:597–603.
- Yagi K, Matsui Y, Nakano S, et al. Treatment of knee osteoarthritis associated with extraarticular varus deformity of the femur: staged total knee arthroplasty following corrective osteotomy. J Orthop Sci. 2006 Jul;11(4):386–389.
- Efe T, Heyse TJ, Boese C, et al. TKA following high tibial osteotomy versus primary TKA--a matched pair analysis. BMC Musculoskelet Disord. 2010 Sep 14;11:207.
- Rosa N, Marta M, Vaz M, et al. Intramedullary nailing biomechanics: Evolution and challenges. Proc Inst Mech Eng H. 2019 Mar;233(3):295–308.
- Hu L, Xiong Y, Mi B, et al. Comparison of intramedullary nailing and plate fixation in distal tibial fractures with metaphyseal damage: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2019 Jan 25;14(1):30.
- Meena RC, Meena UK, Gupta GL, et al. Intramedullary nailing versus proximal plating in the management of closed extra-articular proximal tibial fracture: a randomized controlled trial. J Orthop Traumatol. 2015 Sep;16(3):203–208.
- Wahab H, Fahad S, Noor-Us-Sabah TA, et al. Correction of lower limb deformities with fixator assisted nailing. Ann Med Surg (Lond). 2019 Sep;45:40–44.
- Fragomen AT, Rozbruch SR. The mechanics of external fixation. HSS J. 2007 Feb;3(1):13–29.
- Kani KK, Porrino JA, Chew FS. External fixators: looking beyond the hardware maze. Skeletal Radiol. 2020 Mar;49(3):359–374.
- Nozaka K, Miyakoshi N, Saito H, et al. Effectiveness of circular hexapod external fixation with soft tissue reconstruction in treating severe knee dislocation due to burn scarring: a case report. BMC Musculoskelet Disord. 2020 Sep 28;21(1):639.
- Nozaka K, Miyakoshi N, Saito H, et al. Effectiveness of Ilizarov external fixation in elderly patients with pilon fractures. J Orthop Sci. 2021 Mar;26(2):254–260.
- Seah KT, Shafi R, Fragomen AT, et al. Distal femoral osteotomy: is internal fixation better than external? Clin Orthop Relat Res. 2011 Jul;469(7):2003–2011.
- Parameswaran AD, Roberts CS, Seligson D, et al. Pin tract infection with contemporary external fixation: how much of a problem? J Orthop Trauma. 2003 Aug;17(7):503–507.
- Kazmers NH, Fragomen AT, Rozbruch SR. Prevention of pin site infection in external fixation: a review of the literature. Strategies Trauma Limb Reconstr. 2016 Aug;11(2):75–85.