Adopting lateralization techniques in reverse shoulder arthroplasty
Preview
Shoulder joint replacement surgery has revolutionized the treatment options for patients with various etiologies affecting the shoulder. Furthermore, the technique of reverse shoulder arthroplasty (RSA) emerged as a game changer for patients that could not be fitted with traditional implant designs due to abnormal anatomical issues or muscle function instability. For years, the Grammont concept using a medialized approach provided relief to patients and excellent survival rates; however, its drawbacks have paved the way for a more lateralized approach. Here, Markus Scheibel (Chief Physician of the Shoulder and Elbow Surgery Department at Schulthess Clinic Zurich, Switzerland and visiting professor at Charité—University Medicine, Berlin, Germany) and Jan-Philipp Imiolczyk (assistant orthopedic trauma surgeon at Charité—University Medicine, Berlin, Germany) explain the concept and practice of lateralization and the current data on its outcomes and complications.
Markus Scheibel
AO Recon Shoulder Curriculum
Taskforce
Schulthess Clinic
Zurich, Switzerland

Jan-Philipp Imiolczyk
Charité—University Medicine
Berlin, Germany
Concept transition: Why shift from the classic Grammont concept?
Although first designs for shoulder arthroplasty have been in use since the 1970s, it was not until the late 1980s when Paul Grammont (Dijon, France) published his concept with a hemisphere directly attached to the glenoid surface. This design provided reliable, good clinical results with relatively low initial complication rates compared to the prosthesis used in the past. It was based on a medialized and distalized approach for RSA [1], with survivorship of about 90% at long-term follow-ups of 8–10 years [2]. The approach followed four main principles (summarized by Werthel et al [3]):
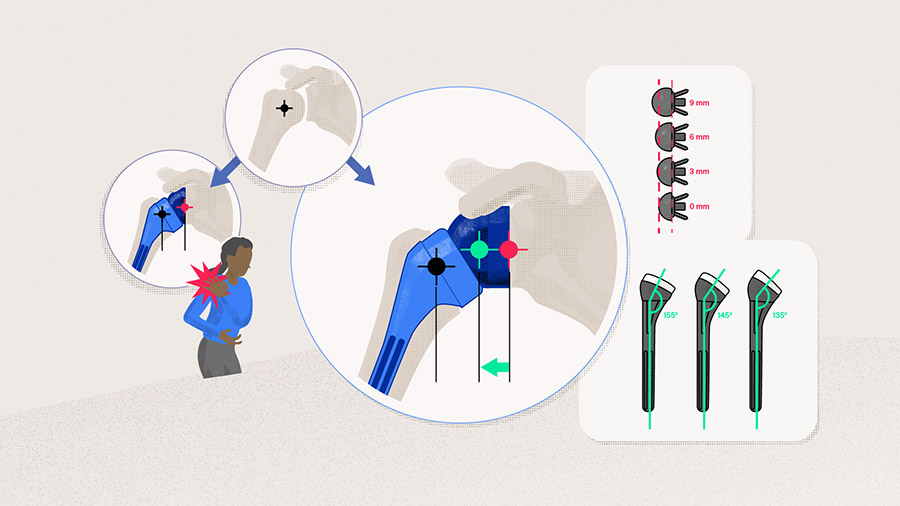
- Medialization of the joint center of rotation (JCOR) on the glenoid and the humerus with a straight stem and a 155° neck-shaft angle (NSA), which aims to increase the lever arm of the deltoid in active elevation and abduction
- Positioning the JCOR at the bone-implant interface minimizes shear forces on the glenoid component
- Distalization of the humerus, which helps to recruit more fibers of the anterior and posterior deltoid to act as abductors
- A semi-constrained configuration to provide static stability and a stable fulcrum
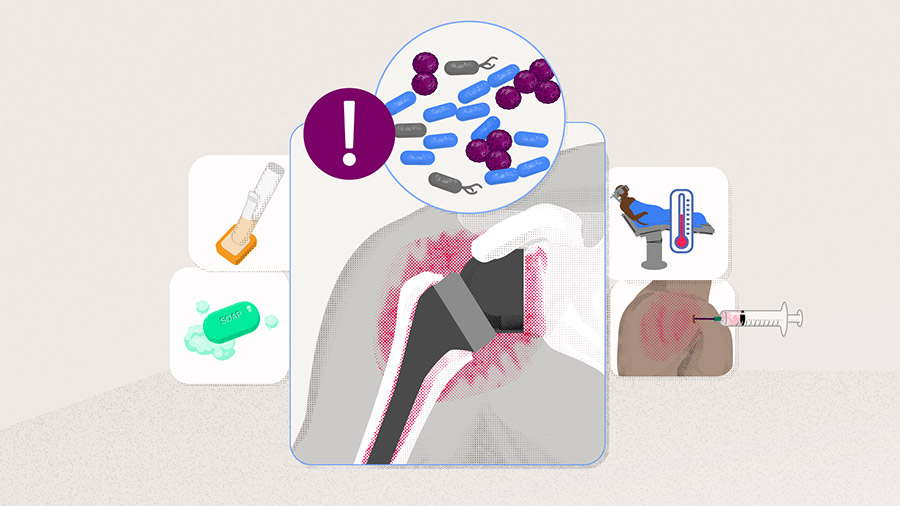
Despite the success of this approach, especially in cuff-deficient shoulders, its design has been reported to have several drawbacks. One of the main complications associated with RSA is prothesis instability; with 38% of patients undergoing revision surgery after a Grammont design RSA [4], two key factors for implant stability are the correct restoration of deltoid length and lateralization, as this provides sufficient tensioning of the soft tissues [5]. Moreover, a high number of patients undergoing Grammont design RSA suffer from scapular notching, as well as limited range of passive internal rotation and in particular no improvement in active external rotation capacity, and loss of normal shoulder contour [6, 7]. Notching is not just a radiographic phenomenon but has been shown to be progressive over time. One study analyzed notching in a Grammont design RSA and showed the notch incidence as a function increased from 58% occurring in the first 2–3 years after surgery to 87% at 6–10 years; however, in some cases, no notching was reported or notches stabilized rapidly after their appearance [8]. Overall, the study found the incidence of notching in 68% of cases with a mean follow-up of 51 months and a range of 50–96% at the 31–84 months follow-up. The study also found that the more active patients had a higher rate of notch incidence as well as original diagnosis of cuff tear arthroplasty (71%) and osteoarthritis (OA) (47%) with cuff deficiency influencing the incidence of notching [8]. When comparing cemented and uncemented components of the Grammont RSA over a mean 9.6-year follow-up, Melis et al [9] found scapular notching in 88% of shoulders, which was associated with the superolateral approach. Furthermore, they also found glenoid radiolucency, bony scapular spur, subsidence of the stem, and humeral radiolucency in three and four zones in cemented and one and two zones in uncemented components, with more signs of radiological stress shielding and resorption in uncemented components [9]. Attention should be paid when classifying notching on x-rays because the positioning and view of the x-ray when grading the notching are essential. It is clear, though, that scapular notching in the Grammont design is a complication that should be avoided. So, how have surgeons tried to compensate for these drawbacks that occur in the Grammont concept?
Read the full article with your AO login
- The arrival of lateralization
- Glenoid-sided lateralization
- Humeral-sided lateralization
- Global bipolar lateralization
- Proposed technique: What works for us?
- Is lateralized reverse shoulder arthroplasty performing?
- Future perspectives
- Conclusion
Additional AO resources
Access videos, tools, and other assets.
- Videos
- Upcoming events: AO Recon Course finder
Contributing experts

Ashish Gupta
Queensland Orthopedic Clinic
Brisbane, Australia

Simon Lambert
AO Recon Shoulder Curriculum Taskforce
University College London Hospital
London, United Kingdom
Markus Scheibel
AO Recon Shoulder Curriculum Taskforce
Schulthess Clinic
Zurich, Switzerland

Jan-Philipp Imiolczyk
Charité—University Medicine
Berlin, Germany
This article was written by Laura Kehoe, AO Innovation Translation Center, Clinical Science, Switzerland.
References
- Hatzidakis AM, Norris TR, Boileau P. Reverse shoulder arthroplasty indications, technique, and results. Techniques in Shoulder & Elbow Surgery. 2005;6(3):135–149.
- Bacle G, Nové-Josserand L, Garaud P, et al. Long-Term Outcomes of Reverse Total Shoulder Arthroplasty: A Follow-up of a Previous Study. J Bone Joint Surg Am. 2017 Mar 15;99(6):454–461.
- Werthel JD, Walch G, Vegehan E, et al. Lateralization in reverse shoulder arthroplasty: a descriptive analysis of different implants in current practice. Int Orthop. 2019 Oct;43(10):2349–2360.
- Boileau P. Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res. 2016 Feb;102(1 Suppl):S33–43.
- Guarrella V, Chelli M, Domos P, et al. Risk factors for instability after reverse shoulder arthroplasty. Shoulder Elbow. 2021 Feb;13(1):51–57.
- Seebauer L. Total reverse shoulder arthroplasty: European lessons and future trends. Am J Orthop (Belle Mead NJ). 2007 Dec;36(12 Suppl 1):22–28.
- Boileau P, Watkinson DJ, Hatzidakis AM, et al. Grammont reverse prosthesis: Design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005 Jan–Feb;14(1 Suppl S):147s–161s.
- Lévigne C, Garret J, Boileau P, et al. Scapular notching in reverse shoulder arthroplasty: is it important to avoid it and how? Clin Orthop Relat Res. 2011 Sep;469(9):2512–2520.
- Melis B, DeFranco M, Lädermann A, et al. An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg Br. 2011 Sep;93(9):1240–1246.
- Bauer S, Corbaz J, Athwal GS, et al. Lateralization in Reverse Shoulder Arthroplasty. J Clin Med. 2021 Nov 18;10(22).
- Boileau P, Moineau G, Roussanne Y, et al. Bony increased-offset reversed shoulder arthroplasty: minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res. 2011 Sep;469(9):2558–2567.
- Boileau P, Moineau G, Roussanne Y, et al. Bony Increased Offset-Reversed Shoulder Arthroplasty (BIO-RSA). JBJS Essent Surg Tech. 2017 Dec 28;7(4):e37.
- Boileau P, Morin-Salvo N, Bessière C, et al. Bony increased-offset-reverse shoulder arthroplasty: 5 to 10 years' follow-up. J Shoulder Elbow Surg. 2020 Oct;29(10):2111–2122.
- Greiner S, Schmidt C, Herrmann S, et al. Clinical performance of lateralized versus non-lateralized reverse shoulder arthroplasty: a prospective randomized study. J Shoulder Elbow Surg. 2015 Sep;24(9):1397–1404.
- Franceschetti E, Ranieri R, Giovanetti de Sanctis E, et al. Clinical results of bony increased-offset reverse shoulder arthroplasty (BIO-RSA) associated with an onlay 145° curved stem in patients with cuff tear arthropathy: a comparative study. J Shoulder Elbow Surg. 2020 Jan;29(1):58–67.
- Jones RB, Wright TW, Roche C. Bone Grafting the Glenoid Versus Use of Augmented Glenoid Baseplates with Reverse Shoulder Arthroplasty. Bull Hosp Jt Dis (2013). 2015 Dec;73 Suppl 1:S129–135.
- Liuzza L, Mai DH, Grey S, et al. Reverse Total Shoulder Arthroplasty with a Superior Augmented Glenoid Component for Favard Type-E1, E2, and E3 Glenoids. J Bone Joint Surg Am. 2020 Nov 4;102(21):1865–1873.
- Virk M, Yip M, Liuzza L, et al. Clinical and radiographic outcomes with a posteriorly augmented glenoid for Walch B2, B3, and C glenoids in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2020 May;29(5):e196–e204.
- Kirsch JM, Patel M, Singh A, et al. Early clinical and radiographic outcomes of an augmented baseplate in reverse shoulder arthroplasty for glenohumeral arthritis with glenoid deformity. J Shoulder Elbow Surg. 2021 Jul;30(7s):S123–s130.
- Werner BC, Lederman E, Gobezie R, et al. Glenoid lateralization influences active internal rotation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2021 Nov;30(11):2498–2505.
- Endell D, Imiolczyk J-P, Grob A, et al. Full-wedge metallic reconstruction of glenoid bone deficiency in reverse shoulder arthroplasty. Obere Extremität. 2020;15:213–216.
- Imiolczyk JP, Audigé L, Harzbecker V, et al. Metallic humeral and glenoid lateralized implants in reverse shoulder arthroplasty for cuff tear arthropathy and primary osteoarthritis. JSES Int. 2022 Mar;6(2):221–228.
- Beltrame A, Di Benedetto P, Cicuto C, et al. Onlay versus Inlay humeral steam in Reverse Shoulder Arthroplasty (RSA): clinical and biomechanical study. Acta Biomed. 2019 Dec 5;90(12-s):54–63.
- Ascione F, Kilian CM, Laughlin MS, et al. Increased scapular spine fractures after reverse shoulder arthroplasty with a humeral onlay short stem: an analysis of 485 consecutive cases. J Shoulder Elbow Surg. 2018 Dec;27(12):2183–2190.
- Ferle M, Pastor MF, Hagenah J, et al. Effect of the humeral neck-shaft angle and glenosphere lateralization on stability of reverse shoulder arthroplasty: a cadaveric study. J Shoulder Elbow Surg. 2019 May;28(5):966–973.
- Gruber MD, Kirloskar KM, Werner BC, et al. Factors Associated with Internal Rotation Following Reverse Shoulder Arthroplasty: A Narrative Review. JSES Reviews, Reports, and Techniques. 2022;2:117–124.
- Freislederer F, Toft F, Audigé L, et al. Lateralized vs. classic Grammont-style reverse shoulder arthroplasty for cuff deficiency Hamada stage 1-3: does the design make a difference? J Shoulder Elbow Surg. 2022 Feb;31(2):341–351.
- Helmkamp JK, Bullock GS, Amilo NR, et al. The clinical and radiographic impact of center of rotation lateralization in reverse shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2018 Nov;27(11):2099–2107.