Biomechanical advantages of a short hip stem
Preview
Over the past two decades, short, cementless hip stems have increasingly been used in total hip arthroplasty (THA). The design concept of these short (hip) stems promises better bone and soft-tissue preservation without negatively affecting implant survival. What is the biomechanical basis for such promises? Do short stems of different design concepts, such as the geometry, materials, and surface finishing, differ in their biomechanical properties? How does the length of the stems affect their biomechanical properties? In this article, Marco Ezechieli (chief orthopedic surgeon at the Clinic for Orthopedics, Traumatology, and Sports traumatology, St Vincenz Hospital Ltd. Paderborn, location St. Josef's Hospital, Salzkotten, Germany) reviews the current evidence on the biomechanical advantages of short stems over traditional designs.
Are short stems in total hip arthroplasty really necessary?
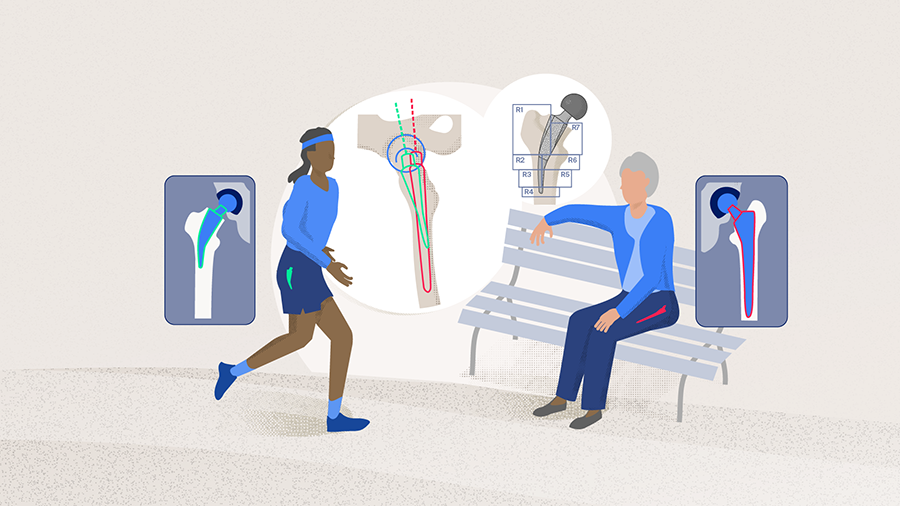
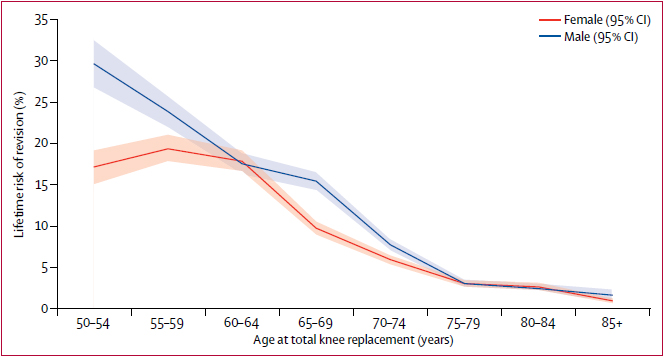
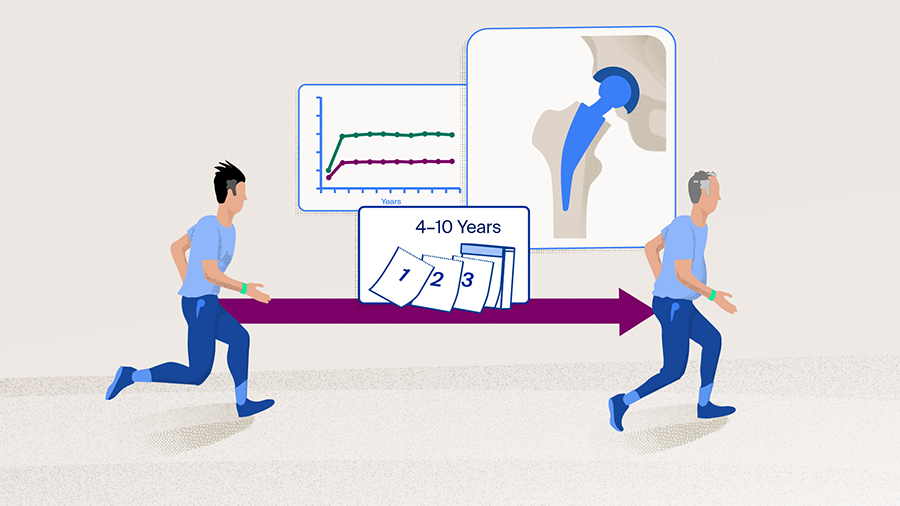
Total hip arthroplasty is one of the most popular and successful surgeries that leads to reduced pain and improved function and quality of life for patients. It is also cost-effective with a high implant survival rate [1–3]. However, the indication for THA has been widening and it has been applied in increasingly younger patients. Although national registries have shown that the 10-year implant survival rate for patients older than 75 years is about 98%, it is about 88% for patients younger than 50 years [4]. Bayliss et al [2] showed an even more concerning trend: When analyzed according to the age of the patient at the time of primary THA, the lifetime risk of implant revision (LTRR) for patients 75 years or older was about 4% or lower (Figure 1). For men 50–54 years of age, however, the LTRR was about 30% [2]. Such results caution us that patients who receive their primary THA at a younger age are more likely to require a revision surgery during their lifetime—not just because they have a longer life expectancy, but also because they are likely to be more active, and therefore, implants in young patients will have more cycles of usage and need to sustain higher load in comparison to implants in older patients.
Aiming for bone stock preservation
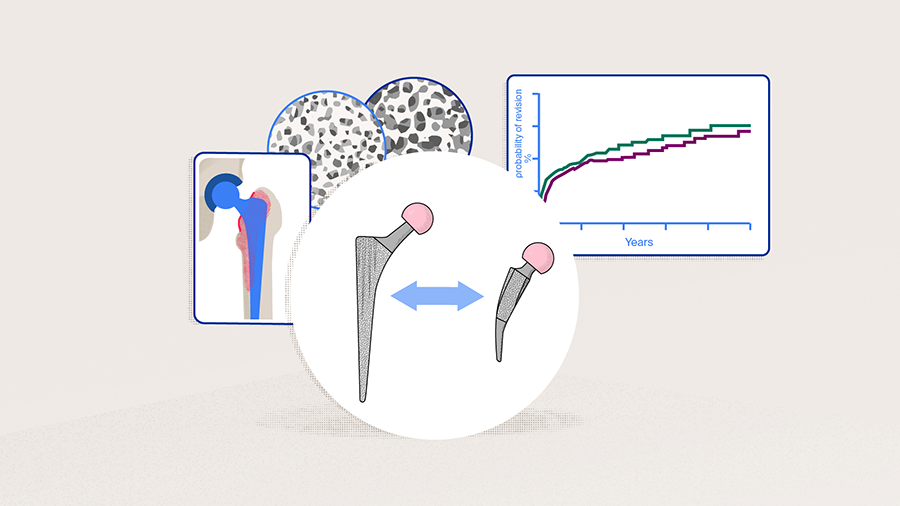
To address the need of younger and more active patients, short femoral stems were originally developed based on a bone- and soft-tissue-sparing implantation approach, with the primary concept of metaphyseal anchoring [3]. Although numerous short stems have emerged through innovative designs and modifications of standard stems through the years, the most popular short stems currently in use can be roughly divided into two groups based on their anchoring concepts, ie, calcar-loading versus shortened tapered stems [5]. The main goal of a short-stem design is to preserve proximal bone stock and to allow more physiological proximal loading, which should lead to reduced stress shielding. Since stress shielding induces demineralization of the proximal bone, the utilization of short stems in THA promises preservation of proximal bone stock over the long term (see also the section "Reduced stress shielding"). In the event of a revision, the cementless feature can lead to an easier surgery, and the retention of proximal bone stock allows anchoring and osseointegration of the revisional THA stems [1, 4–8].
Other potential advantages of short stems include more anatomical reconstruction of the hip joint [4, 9, 10], as well as preventing impingement of the femoral cortex and thigh pain by avoiding the extension of the stem into the diaphysis [6]. In addition, the modern calcar-guided short stems are inserted by following the calcar of the femoral neck, this allows for an individualized reconstruction based on the patient’s anatomy [3].

Marco Ezechieli
Vincenz Group Paderborn, St Josefs Hospital Salzkotten, Germany
Read the full article with your AO login
- Classification of short stems
- Biomechanical advantages of femoral neck conservation
- Key biomechanical considerations: primary implant stability and stress shielding
- Primary stability: Is it a trade-off for stress shielding?
- Reduced stress shielding
- Gruen zones
- Not all short stems are the same
- Anatomical reconstruction
- Potential for further development
- Conclusion
Additional AO resources
Access videos, tools, and other assets.
- Videos
- Books in Thieme store
- AO Surgery Reference
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Martin Buttaro
Italian Hospital Buenos Aires, Argentina

Marco Ezechieli
Vincenz Group Paderborn, St Josefs Hospital Salzkotten, Germany
Carlos Martin Lucero
Italian Hospital Buenos Aires, Argentina
References
- Falez F, Casella F, Panegrossi G, et al. Perspectives on metaphyseal conservative stems. J Orthop Traumatol. 2008 Mar;9(1):49–54.
- Bayliss LE, Culliford D, Monk AP, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017 Apr 8;389(10077):1424–1430.
- Kutzner KP. Calcar-guided short-stem total hip arthroplasty: Will it be the future standard? Review and perspectives. World J Orthop. 2021 Aug 18;12(8):534–547.
- Ezechieli M, Windhagen H, Matsubara M, et al. A neck-preserving short stem better reconstructs the centre of rotation than straight stems: a computed tomography-based cadaver study. Arch Orthop Trauma Surg. 2021 Jul 6.
- Freitag T, Bieger R, Kiefer H, et al. Biomechanics of a calcar loading and a shortened tapered femoral stem: Comparative in-vitro testing of primary stability and strain distribution. J Exp Orthop. 2021 Sep 7;8(1):74.
- Kim Y-H. Ultra-Short Bone Conserving Cementless Femoral Stem. Hip Pelvis. 2021 12/;33(4):181–189.
- van Oldenrijk J, Molleman J, Klaver M, et al. Revision rate after short-stem total hip arthroplasty: a systematic review of 49 studies. Acta Orthop. 2014 Jun;85(3):250–258.
- Falez F, Casella F, Papalia M. Current concepts, classification, and results in short stem hip arthroplasty. Orthopedics. 2015 Mar;38(3 Suppl):S6–13.
- Mihalko WM, Assaf D, Sungu M. Reproducing the hip center with a femoral neck-retaining implant. Orthopedics. 2015 Mar;38(3 Suppl):S21–26.
- Windhagen H, Chincisan A, Choi HF, et al. Soft-tissue balance in short and straight stem total hip arthroplasty. Orthopedics. 2015 Mar;38(3 Suppl):S14–20.
- Khanuja HS, Banerjee S, Jain D, et al. Short bone-conserving stems in cementless hip arthroplasty. J Bone Joint Surg Am. 2014 Oct 15;96(20):1742–1752.
- Yan SG, Weber P, Steinbrück A, et al. Periprosthetic bone remodelling of short-stem total hip arthroplasty: a systematic review. Int Orthop. 2018 Sep;42(9):2077–2086.
- Freeman MA. Why resect the neck? J Bone Joint Surg Br. 1986 May;68(3):346–349.
- Carlson L, Albrektsson B, Freeman MA. Femoral neck retention in hip arthroplasty. A cadaver study of mechanical effects. Acta Orthop Scand. 1988 Feb;59(1):6–8.
- Yamako G, Chosa E, Totoribe K, et al. Trade-off between stress shielding and initial stability on an anatomical cementless stem shortening: in-vitro biomechanical study. Med Eng Phys. 2015 Aug;37(8):820–825.
- Freitag T, Kutzner KP, Bieger R, et al. Biomechanics of a cemented short stem: a comparative in vitro study regarding primary stability and maximum fracture load. Archives of Orthopaedic and Trauma Surgery. 2021 2021/10/01;141(10):1797–1806.
- Bieger R, Ignatius A, Reichel H, et al. Biomechanics of a short stem: In vitro primary stability and stress shielding of a conservative cementless hip stem. J Orthop Res. 2013 Aug;31(8):1180–1186.
- Bieger R, Ignatius A, Decking R, et al. Primary stability and strain distribution of cementless hip stems as a function of implant design. Clin Biomech (Bristol, Avon). 2012 Feb;27(2):158–164.
- Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979 Jun(141):17–27.
- Yan SG, Chevalier Y, Liu F, et al. Metaphyseal anchoring short stem hip arthroplasty provides a more physiological load transfer: a comparative finite element analysis study. J Orthop Surg Res. 2020 Oct 29;15(1):498.
- Burchard R, Braas S, Soost C, et al. Bone preserving level of osteotomy in short-stem total hip arthroplasty does not influence stress shielding dimensions - a comparing finite elements analysis. BMC Musculoskelet Disord. 2017 Aug 7;18(1):343.
- Schmidutz F, Beirer M, Weber P, et al. Biomechanical reconstruction of the hip: comparison between modular short-stem hip arthroplasty and conventional total hip arthroplasty. Int Orthop. 2012 Jul;36(7):1341–1347.