Risk factors in treatment of periprosthetic fractures
Preview
Although primary total hip replacement (THR) has, in general, excellent long-term outcomes, periprosthetic femoral fracture (PPFF) after THR is a serious complication. The treatment of PPFF is clinically challenging with high mortality, morbidity, and associated costs. In recognizing the risk factors in treatment of PPFF, surgeons can try to optimize the treatment and contribute to society with efficient and effective patient care. In this article, the general risk factors in treating PPFF patients are discussed along with the ways to ameliorate them.
Epidemiology
THR has become one of the most successful orthopedic interventions over the last decades. The excellent results have led to an expanded indication to include both younger and more elderly adults [1]. Younger patients tend to be more active and more elderly patients tend to have poorer bone quality and increased comorbidity; such factors result in the increased probability of implant loosening and increase the chance of PPFF [2–4]. Meanwhile, with the increasing longevity of the population in general, patients with hip replacement can also be expected to live longer, which means that the implants will be in service for longer, and therefore have an increased likelihood of failing [1, 5]. This has been demonstrated by data from a Swedish registry; in the Scottish and Finnish populations this has been less clear [5–7].
Concerning such discrepancies in different epidemiological studies, Cao Li, president of the Chinese Hip Society and director of the First Affiliated Hospital Xinjiang University, Urumqi, China, reminds us that, "Epidemiological studies are empirical studies. Many of them may be simply too small to give us a definitive answer. Currently, studies on intraoperative risk factors of periprosthetic acetabular fractures are still lacking."

Cao Li
First Affiliated Hospital of Xinjiang Medical University
Urumqi, China

Baochao Ji
First Affiliated Hospital of Xinjiang Medical University
Urumqi, China
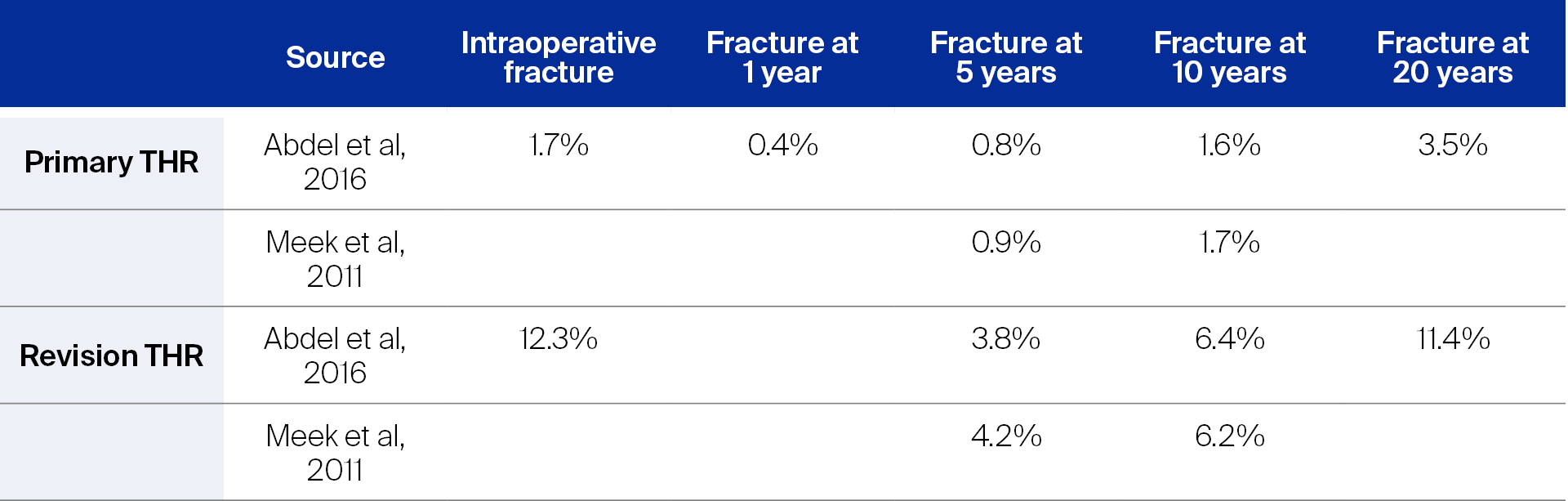
How does the outcome of revision THR compare with primary THR?
When compared with primary THRs, the risk of suffering a PPFF is much higher in revision THR, although not many studies have directly compared the incidences of PPFF between primary and revision THR. Lindahl et al reported an incidence of 0.4% in primary and 2.1% in revision THR, and Kavanagh estimated the incidence to be 1% after primary total hip arthroplasty (THA) and 4.2% after revision THA [3, 8]. In assessing 32,644 primary and 5,417 revision THR cases from 1969 to 2011 in the United States, Abdel et al showed a large increase in the incidence of intraoperative fractures in revision THR: from 1.7% for primary THR to 12.3% for revision THR. In the same study, the cumulative probability of suffering a PPFF was 0.8% for primary THR and 3.8% for revision THR at five years [1, 9] (Table 1). Meek et al came to similar results using data from a Scottish national database between 1997 and 2008 (52,136 primary THR, 8,726 revision THR); they reported a hazard ratio of revision THR being 4.4 times more likely to end in a PPFF than primary THR [5].
The mortality following surgical treatment for PPFF ranged widely from 3.3% to 34% at one year [10–13].
Injury mechanism
PPFFs often (75–84%) occur after minor trauma or ground-level falls, compared to “spontaneous” fracture (8–18%) after primary THR (the incidence of the latter can be as high as 37–50% after revision THR) [14, 15]. In a study by Bethea et al, it was shown that 75% of the patients treated for PPFF had prefracture radiographic evidence of loosening. The authors explained that, “As loosening progresses, a fibrous layer develops between the bone and the cement, increased movement at this interface results in further bone resorption.” [4]
While the fracture itself is easy to diagnose, component loosening often remains unrecognized. The history the preinjury symptoms and the knowledge of the mechanism of failure may shed light on the condition of the implants; both are therefore important for treatment decision-making. For example, spontaneous fractures in the early postoperative period should raise clinical suspicion for an unrecognized intraoperative fracture, whereas late spontaneous fractures are often associated with underlying osteolysis [15]. In case of low-energy trauma events, patients often do not provide any traumatic history but describe a gradually increasing pain [16–18]. A prodrome of thigh pain, especially start-up pain, is suggestive of a loose femoral component that may have been a contributing factor to the fracture.
What are the risk factors?
Surgical management of PPFF is technically demanding, requiring skills in both arthroplasty and trauma. Implant loosening, compromised surgical bed, osteolysis, osteoporosis, and concurrent infection are some of the challenges that often confront the surgeons. Understanding and identifying the perioperative risk factors is a key step towards reducing complications and will help with the treatment decision.
Read the full article with your AO login
- What are the risk factors?
- Patient-related risk factors: gender, age, and comorbidity
- Implant-related risk factors: cemented versus uncemented implants
- How can surgeon-related risk be reduced when treating PPFF?
- Vancouver classification system
- Surgeon-related risk: Unidentified periprosthetic joint infection
- Postoperative risk factors
- Conclusion
More AO resources
Access videos, tools, and other assets to learn more about this topic:
- AO Surgery Reference
- AO Videos (AO login required)
- AO Course finder
- AO Classification (UCS) (PDF)
- AO E-book
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Baochao Ji
First Affiliated Hospital of Xinjiang Medical University
Urumqi, China

Cao Li
First Affiliated Hospital of Xinjiang Medical University
Urumqi, China

Karl Stoffel
University Hospital Basel
Basel, Switzerland

Luigi Zagra
IRCCS Galeazzi Orthopaedic Institute Milan
Milan, Italy
This issue was written by Maio Chen, AO Innovation Translation Center, Clinical Science, Switzerland.
References
- Abdel MP, Watts CD, Houdek MT, et al. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Joint J. 2016 Apr;98-b(4):461–467.
- Cook RE, Jenkins PJ, Walmsley PJ, et al. Risk factors for periprosthetic fractures of the hip: a survivorship analysis. Clinical orthopaedics and related research. 2008 Jul;466(7):1652–1656.
- Lindahl H, Garellick G, Regnér H, et al. Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am. 2006 Jun;88(6):1215–1222.
- Bethea JS, 3rd, DeAndrade JR, Fleming LL, et al. Proximal femoral fractures following total hip arthroplasty. Clinical orthopaedics and related research. 1982 Oct(170):95–106.
- Meek RM, Norwood T, Smith R, et al. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br. 2011 Jan;93(1):96–101.
- Chatziagorou G, Lindahl H, Garellick G, et al. Incidence and demographics of 1751 surgically treated periprosthetic femoral fractures around a primary hip prosthesis. Hip Int. 2019 May;29(3):282–288.
- Sarvilinna R, Huhtala HS, Puolakka TJ, et al. Periprosthetic fractures in total hip arthroplasty: an epidemiologic study. Int Orthop. 2003;27(6):359–361.
- Kavanagh BF. Femoral fractures associated with total hip arthroplasty. The Orthopedic clinics of North America. 1992 Apr;23(2):249–257.
- Abdel MP, Houdek MT, Watts CD, et al. Epidemiology of periprosthetic femoral fractures in 5417 revision total hip arthroplasties: a 40-year experience. Bone Joint J. 2016 Apr;98-b(4):468–474.
- Bhattacharyya T, Chang D, Meigs JB, et al. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007 Dec;89(12):2658–2662.
- Phillips JR, Moran CG, Manktelow AR. Periprosthetic fractures around hip hemiarthroplasty performed for hip fracture. Injury. 2013 Jun;44(6):757–762.
- Spina M, Rocca G, Canella A, et al. Causes of failure in periprosthetic fractures of the hip at 1- to 14-year follow-up. Injury. 2014 Dec;45 Suppl 6:S85–92.
- Lindahl H, Oden A, Garellick G, et al. The excess mortality due to periprosthetic femur fracture. A study from the Swedish national hip arthroplasty register. Bone. 2007 May;40(5):1294–1298.
- Franklin J, Malchau H. Risk factors for periprosthetic femoral fracture. Injury. 2007 Jun;38(6):655–660.
- Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clinical orthopaedics and related research. 2004 Mar(420):80–95.
- Fleischman AN, Chen AF. Periprosthetic fractures around the femoral stem: overcoming challenges and avoiding pitfalls. Ann Transl Med. 2015 Sep;3(16):234.
- Moreta J, Aguirre U, de Ugarte OS, et al. Functional and radiological outcome of periprosthetic femoral fractures after hip arthroplasty. Injury. 2015 Feb;46(2):292–298.
- Ninan TM, Costa ML, Krikler SJ. Classification of femoral periprosthetic fractures. Injury. 2007 Jun;38(6):661–668.
- Drew JM, Griffin WL, Odum SM, et al. Survivorship After Periprosthetic Femur Fracture: Factors Affecting Outcome. J Arthroplasty. 2016 Jun;31(6):1283–1288.
- Sellan ME, Lanting BA, Schemitsch EH, et al. Does Time to Surgery Affect Outcomes for Periprosthetic Femur Fractures? J Arthroplasty. 2018 Mar;33(3):878–881.
- Berry DJ. Epidemiology: hip and knee. The Orthopedic clinics of North America. 1999 Apr;30(2):183–190.
- Tsiridis E, Pavlou G, Venkatesh R, et al. Periprosthetic Femoral Fractures around Hip Arthroplasty: Current Concepts in their Management. HIP International. 2009;19(2):75–86.
- Dale H, Børsheim S, Kristensen TB, et al. Fixation, sex, and age: highest risk of revision for uncemented stems in elderly women - data from 66,995 primary total hip arthroplasties in the Norwegian Arthroplasty Register. Acta Orthop. 2020 Feb;91(1):33–41.
- Marsland D, Mears SC. A review of periprosthetic femoral fractures associated with total hip arthroplasty. Geriatr Orthop Surg Rehabil. 2012 Sep;3(3):107–120.
- Selvaratnam V, Shetty V, Sahni V. Subsidence in Collarless Corail Hip Replacement. Open Orthop J. 2015;9:194–197.
- Springer BD, Berry DJ, Lewallen DG. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am. 2003 Nov;85(11):2156–2162.
- Canbora K, Kose O, Polat A, et al. Management of Vancouver type B2 and B3 femoral periprosthetic fractures using an uncemented extensively porous-coated long femoral stem prosthesis. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie. 2013 Jul;23(5):545– 552.
- O'Shea K, Quinlan JF, Kutty S, et al. The use of uncemented extensively porous-coated femoral components in the management of Vancouver B2 and B3 periprosthetic femoral fractures. J Bone Joint Surg Br. 2005 Dec;87(12):1617–1621.
- Wang Q, Li D, Kang P. Uncemented extensive porous titanium-coated long femoral stem prostheses are effective in treatment of Vancouver type B2 periprosthetic femoral fractures: A retrospective mid- to long-term follow-up study. J Orthop Surg (Hong Kong). 2019 May– Aug;27(2):2309499019857653.
- Abdel MP, Lewallen DG, Berry DJ. Periprosthetic femur fractures treated with modular fluted, tapered stems. Clinical orthopaedics and related research. 2014 Feb;472(2):599–603.
- Feng S, Zhang Y, Bao YH, et al. Comparison of modular and nonmodular tapered fluted titanium stems in femoral revision hip arthroplasty: a minimum 6-year follow-up study. Sci Rep. 2020 Aug 13;10(1):13692.
- Munro JT, Masri BA, Garbuz DS, et al. Tapered fluted modular titanium stems in the management of Vancouver B2 and B3 peri-prosthetic fractures. Bone Joint J. 2013 Nov;95-b(11 Suppl A):17–20.
- Stoffel K SC, Meyer C, Reinhard S. Internal fixation. In: Schutz M PC, eds. Periprosthetic Fracture Management. Stuttgart: Thieme; 2013. 105–114.
- Spina M, Scalvi A. Vancouver B2 periprosthetic femoral fractures: a comparative study of stem revision versus internal fixation with plate. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2018 Aug;28(6):1133–1142.
- Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instructional course lectures. 1995;44:293–304.
- Brady OH, Garbuz DS, Masri BA, et al. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000 Jan;15(1):59–62.
- Naqvi GA, Baig SA, Awan N. Interobserver and intraobserver reliability and validity of the Vancouver classification system of periprosthetic femoral fractures after hip arthroplasty. J Arthroplasty. 2012 Jun;27(6):1047–1050.
- Schwarzkopf R, Oni JK, Marwin SE. Total hip arthroplasty periprosthetic femoral fractures: a review of classification and current treatment. Bull Hosp Jt Dis (2013). 2013;71(1):68–78.
- Quah C, Porteous M, Stephen A. Principles of managing Vancouver type B periprosthetic fractures around cemented polished tapered femoral stems. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2017 May;27(4):477–482.
- Van Houwelingen AP, Duncan CP. The pseudo A(LT) periprosthetic fracture: it's really a B2. Orthopedics. 2011 Sep 9;34(9):e479–481.
- Korbel M, Sponer P, Kucera T, et al. Results of treatment of periprosthetic femoral fractures after total hip arthroplasty. Acta Medica (Hradec Kralove). 2013;56(2):67–72.
- Moazen M, Mak JH, Etchels LW, et al. The effect of fracture stability on the performance of locking plate fixation in periprosthetic femoral fractures. J Arthroplasty. 2013 Oct;28(9):1589–1595.
- Corten K, Vanrykel F, Bellemans J, et al. An algorithm for the surgical treatment of periprosthetic fractures of the femur around a well-fixed femoral component. J Bone Joint Surg Br. 2009 Nov;91(11):1424–1430.
- Bell A, Templeman D, Weinlein JC. Nonunion of the Femur and Tibia: An Update. The Orthopedic clinics of North America. 2016 Apr;47(2):365–375.
- Lindahl H, Malchau H, Odén A, et al. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br. 2006 Jan;88(1):26–30.
- Grammatopoulos G, Pandit H, Kambouroglou G, et al. A unique peri-prosthetic fracture pattern in well fixed femoral stems with polished, tapered, collarless design of total hip replacement. Injury. 2011 Nov;42(11):1271–1276.
- Chevillotte CJ, Ali MH, Trousdale RT, et al. Inflammatory laboratory markers in periprosthetic hip fractures. J Arthroplasty. 2009 Aug;24(5):722–727.
- Banit DM, Kaufer H, Hartford JM. Intraoperative frozen section analysis in revision total joint arthroplasty. Clinical orthopaedics and related research. 2002 Aug(401):230–238.
- Ko PS, Ip D, Chow KP, et al. The role of intraoperative frozen section in decision making in revision hip and knee arthroplasties in a local community hospital. J Arthroplasty. 2005 Feb;20(2):189–195.
- Zagra L, Villa F, Cappelletti L, et al. Can leucocyte esterase replace frozen sections in the intraoperative diagnosis of prosthetic hip infection? Bone Joint J. 2019 Apr;101-B(4):372–377.
- Chudyk AM, Jutai JW, Petrella RJ, et al. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil. 2009 Feb;90(2):246–262.
- Heinonen M, Karppi P, Huusko T, et al. Post-operative degree of mobilization at two weeks predicts one-year mortality after hip fracture. Aging Clin Exp Res. 2004 Dec;16(6):476–480.
- Pavone V, de Cristo C, Di Stefano A, et al. Periprosthetic femoral fractures after total hip arthroplasty: An algorithm of treatment. Injury. 2019 Jul;50 Suppl 2:S45–s51.