Osteosynthesis in periprosthetic fractures: Indications, tips, and tricks
Preview
Currently, most periprosthetic femoral fractures (PPFF) are surgically managed. In treating PPFF, the first and a crucial decision facing the surgeon is: Is osteosynthesis or revision arthroplasty indicated for my patient? Although the current literature does not provide a black and white picture of which patients require stem revision and which require internal fixation only, correct assessment of the stability of the prosthetic implants greatly assists the decision-making process.
It is generally accepted that, in case of a simple fracture type with stable stem, osteosynthesis can be an effective management. However, a loose stem can easily be misdiagnosed as a stable stem, forcing the surgeon to change the treatment plans intraoperatively, since fracture fixation of a loose stem often results in a painful and unsatisfactory condition for the patient. In this article, Karl Stoffel, Chief Physician at the Bethesda Hospital, University Hospital Basel, will first focus on the process of diagnosing a loose stem in the Vancouver types of fractures and then share some general principles as well as some tips in performing osteosynthesis in PPFF. Since the Unified Classification System fracture types D, E, and F are rare, complicated, and have little supporting evidence in the literature, these will not be covered here.

Karl Stoffel
University Hospital Basel
Basel, Switzerland
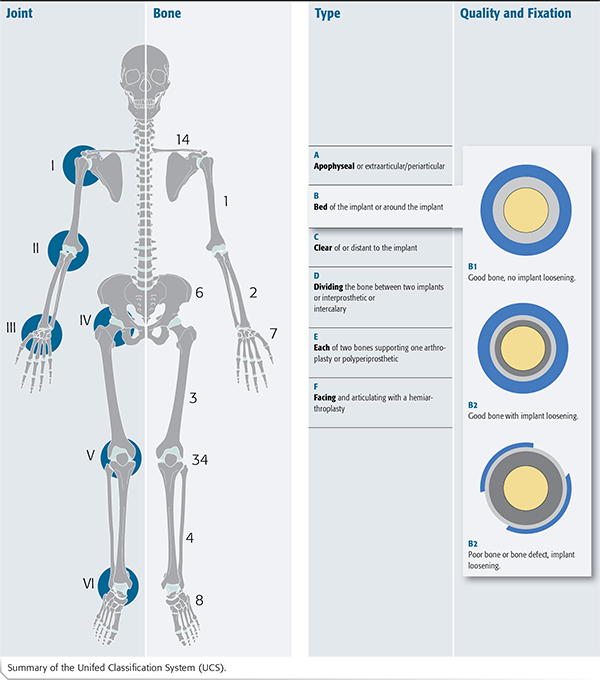
The Unified Classification System (UCS) expanded upon the Vancouver Classification system and in combination with the AO/OTA Fracture and Dislocation Classification, covers all periprosthetic fractures. The UCS fracture types are:
A, Apophyseal
B, Bed of the implant
C, Clear of the implant
D, Dividing the bone between two implants
E, Each of two bones supporting one joint replacement
F, Facing and articulating with arthroplasty
Screenshot from: Velkes S, Stoffel K. Periprosthetic fractures around the hip. In: Schutz M, Perka C, ed. Osteoporotic Fracture Care—Medical and Surgical Management. Stuttgart: Thieme; 2018. 461–478.
Stable or loose: How can we decide?
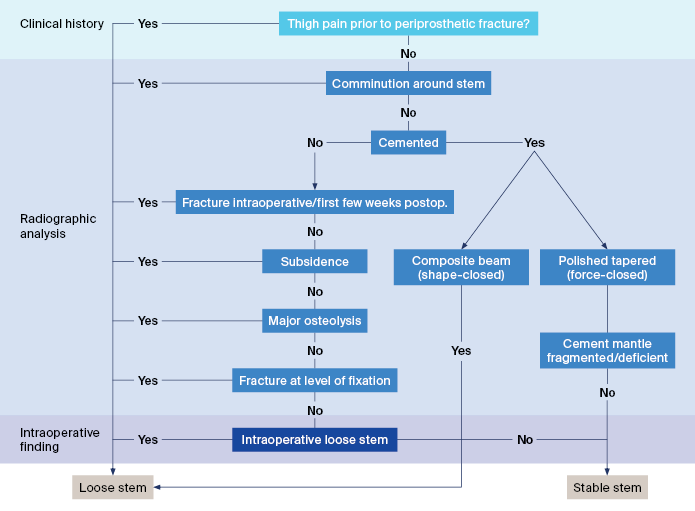
In deciding the stability of the implant, many factors must be considered. Among these are patient-specific factors, fracture patterns, and injury history. To ensure that all essential factors are considered, Karl Stoffel describes an algorithmic approach (Figure 1) that helps surgeons systematically evaluate the fractures using tools that are easily available, such as the patient history, nature of the fracture, stem design, and plain x-rays.
A history of thigh pain
In case of low-energy trauma, patients do not always recall the actual trauma event and cannot provide any trauma history except for the description of gradually increasing pain.
Should a patient describe increasing thigh pain on weight bearing or reduced mobility due to hip problems prior to the fracture, there is a high possibility that a loose stem is involved [1–3].
Read the full article with your AO login
- Radiographic signs of implant instability
- Determining the stability of cementless stems
- Determining the stability of cemented stems
- Testing stability intraoperatively
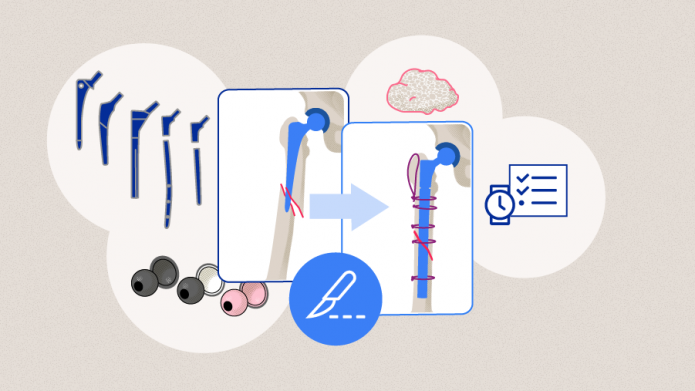
- General management principle: Importance of surgical planning
- How long should a plate be?
- How to determine the number of screws and their placement?
- How to ensure rotational stability and bicortical fixation?
- Special considerations
- Conclusion
More AO resources
Access videos, tools, and other assets to learn more about this topic:
- AO Surgery Reference
- AO Videos (AO login required)
- AO Course finder
- AO Classification (UCS) (PDF)
- AO E-book
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Baochao Ji
First Affiliated Hospital of Xinjiang Medical University
Urumqi, China

Cao Li
First Affiliated Hospital of Xinjiang Medical University
Urumqi, China

Karl Stoffel
University Hospital Basel
Basel, Switzerland

Luigi Zagra
IRCCS Galeazzi Orthopaedic Institute Milan
Milan, Italy
This issue was written by Maio Chen, AO Innovation Translation Center, Clinical Science, Switzerland.
References
- Ninan TM, Costa ML, Krikler SJ. Classification of femoral periprosthetic fractures. Injury. 2007 Jun;38(6):661–668.
- Fleischman AN, Chen AF. Periprosthetic fractures around the femoral stem: overcoming challenges and avoiding pitfalls. Ann Transl Med. 2015 Sep;3(16):234.
- Moreta J, Aguirre U, de Ugarte OS, et al. Functional and radiological outcome of periprosthetic femoral fractures after hip arthroplasty. Injury. 2015 Feb;46(2):292–298.
- Mostofi S. Fracture Classification in Clinical Practice 2nd Edition. 2nd Edition ed. London: Springer-Verlag London; 2012. 115.
- Stoffel K, Horn T, Zagra L, et al. Periprosthetic fractures of the proximal femur: beyond the Vancouver classification. EFORT Open Rev. 2020 Jul;5(7):449–456.
- Streit MR, Haeussler D, Bruckner T, et al. Early Migration Predicts Aseptic Loosening of Cementless Femoral Stems: A Long-term Study. Clinical orthopaedics and related research. 2016 Jul;474(7):1697–1706.
- Johanson PE, Antonsson M, Shareghi B, et al. Early Subsidence Predicts Failure of a Cemented Femoral Stem With Minor Design Changes. Clinical orthopaedics and related research. 2016 Oct;474(10):2221–2229.
- Munro JT, Masri BA, Garbuz DS, et al. Tapered fluted modular titanium stems in the management of Vancouver B2 and B3 peri-prosthetic fractures. Bone Joint J. 2013 Nov;95-b(11 Suppl A):17–20.
- van der Voort P, Pijls BG, Nieuwenhuijse MJ, et al. Early subsidence of shape-closed hip arthroplasty stems is associated with late revision. A systematic review and meta-analysis of 24 RSA studies and 56 survival studies. Acta Orthop. 2015;86(5):575–585.
- Berry DJ. Periprosthetic fractures associated with osteolysis: a problem on the rise. J Arthroplasty. 2003 Apr;18(3 Suppl 1):107–111.
- Marsland D, Mears SC. A review of periprosthetic femoral fractures associated with total hip arthroplasty. Geriatr Orthop Surg Rehabil. 2012 Sep;3(3):107–120.
- Howell JR MH, Ling RSM. Stem Design: The Surgeon’s Perspective. 2005th Edition ed. Breusch S MH, editor: Springer; 2005.
- Quah C, Porteous M, Stephen A. Principles of managing Vancouver type B periprosthetic fractures around cemented polished tapered femoral stems. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie. 2017 May;27(4):477–482.
- Baba T, Homma Y, Momomura R, et al. New classification focusing on implant designs useful for setting therapeutic strategy for periprosthetic femoral fractures. Int Orthop. 2015 Jan;39(1):1–5.
- Corten K, Vanrykel F, Bellemans J, et al. An algorithm for the surgical treatment of periprosthetic fractures of the femur around a well-fixed femoral component. J Bone Joint Surg Br. 2009 Nov;91(11):1424–1430.
- Velkes S, Stoffel K. Periprosthetic fractures around the hip. In: Schutz M, Perka C, ed. Osteoporotic Fracture Care—Medical and Surgical Management. Stuttgart: Thieme; 2018. 461–478.
- Stoffel K, Sommer C, Kalampoki V, et al. The influence of the operation technique and implant used in the treatment of periprosthetic hip and interprosthetic femur fractures: a systematic literature review of 1571 cases. Arch Orthop Trauma Surg. 2016 Apr;136(4):553–561.
- Zenni EJ, Jr., Pomeroy DL, Caudle RJ. Ogden plate and other fixations for fractures complicating femoral endoprostheses. Clinical orthopaedics and related research. 1988 Jun(231):83–90.
- Stoffel K SC, Meyer C, Reinhard S. Internal fixation. In: Schutz M PC, eds. Periprosthetic Fracture Management. Stuttgart: Thieme; 2013. 105–114.
- Chatziagorou G, Lindahl H, Kärrholm J. Lower reoperation rate with locking plates compared with conventional plates in Vancouver type C periprosthetic femoral fractures: A register study of 639 cases in Sweden. i. 2019 Dec;50(12):2292–2300.
- Tadross TS, Nanu AM, Buchanan MJ, et al. Dall-Miles plating for periprosthetic B1 fractures of the femur. J Arthroplasty. 2000 Jan;15(1):47–51.
- Egol KA, Kubiak EN, Fulkerson E, et al. Biomechanics of locked plates and screws. Journal of orthopaedic trauma. 2004 Sep;18(8):488–493.
- Ricci WM, Bolhofner BR, Loftus T, et al. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. J Bone Joint Surg Am. 2005 Oct;87(10):2240–2245.
- Wood GC, Naudie DR, McAuley J, et al. Locking compression plates for the treatment of periprosthetic femoral fractures around well-fixed total hip and knee implants. J Arthroplasty. 2011 Sep;26(6):886–892.
- Smith WR, Ziran BH, Anglen JO, et al. Locking plates: tips and tricks. Instructional course lectures. 2008;57:25–36.
- Bottlang M, Doornink J, Byrd GD, et al. A nonlocking end screw can decrease fracture risk caused by locked plating in the osteoporotic diaphysis. 2009 Mar 1;91(3):620–627.
- Stoffel K, Dieter U, Stachowiak G, et al. Biomechanical testing of the LCP--how can stability in locked internal fixators be controlled? Injury. 2003 Nov;34 Suppl 2:B11–19.
- Stoffel K, Stachowiak G, Forster T, et al. Oblique screws at the plate ends increase the fixation strength in synthetic bone test medium. Journal of Orthopaedic Trauma. 2004 Oct;18(9):611–616.
- Kampshoff J, Stoffel KK, Yates PJ, et al. The treatment of periprosthetic fractures with locking plates: effect of drill and screw type on cement mantles: a biomechanical analysis. Arch Orthop Trauma Surg. 2010 May;130(5):627–632.
- Fulkerson E, Koval K, Preston CF, et al. Fixation of periprosthetic femoral shaft fractures associated with cemented femoral stems: a biomechanical comparison of locked plating and conventional cable plates. Journal of Orthopaedic Trauma. 2006 Feb;20(2):89–93.
- Lenz M, Perren SM, Richards RG, et al. Biomechanical performance of different cable and wire cerclage configurations. Int Orthop. 2013 Jan;37(1):125–130.
- Wang K, Kenanidis E, Miodownik M, et al. Periprosthetic fracture fixation of the femur following total hip arthroplasty: A review of biomechanical testing - Part II. Clin Biomech (Bristol, Avon). 2019 Jan;61:144–162.
- Kim MB, Cho JW, Lee YH, et al. Locking attachment plate fixation around a well-fixed stem in periprosthetic femoral shaft fractures. Arch Orthop Trauma Surg. 2017 Sep;137(9):1193–1200.
- Lenz M, Perren SM, Gueorguiev B, et al. A biomechanical study on proximal plate fixation techniques in periprosthetic femur fractures. Injury. 2014 Jan;45 Suppl 1:S71–75.
- Buttaro MA, Farfalli G, Paredes Núñez M, et al. Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg Am. 2007 Sep;89(9):1964–1969.
- Pavlou G, Panteliadis P, Macdonald D, et al. A review of 202 periprosthetic fractures--stem revision and allograft improves outcome for type B fractures. Hip Int. 2011 Jan-Mar;21(1):21–29.
- Leonidou A, Moazen M, Skrzypiec DM, et al. Evaluation of fracture topography and bone quality in periprosthetic femoral fractures: A preliminary radiographic study of consecutive clinical data. Injury. 2013 Dec;44(12):1799–1804.
- Haddad FS, Duncan CP, Berry DJ, et al. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am. 2002 Jun;84(6):945–950.
- Schwarzkopf R, Oni JK, Marwin SE. Total hip arthroplasty periprosthetic femoral fractures: a review of classification and current treatment. Bull Hosp Jt Dis (2013). 2013;71(1):68–78.
- Solomon LB, Hussenbocus SM, Carbone TA, et al. Is internal fixation alone advantageous in selected B2 periprosthetic fractures? ANZ journal of surgery. 2015 Mar;85(3):169–173.
- Briant-Evans TW, Veeramootoo D, Tsiridis E, et al. Cement-in-cement stem revision for Vancouver type B periprosthetic femoral fractures after total hip arthroplasty. A 3-year follow-up of 23 cases. Acta Orthop. 2009 Oct;80(5):548–552.
- Stoffel K, Blauth M, Joeris A, et al. Fracture fixation versus revision arthroplasty in Vancouver type B2 and B3 periprosthetic femoral fractures: a systematic review. Arch Orthop Trauma Surg. 2020 Feb 21.