Unicompartmental knee arthroplasty versus high tibial osteotomy
Preview
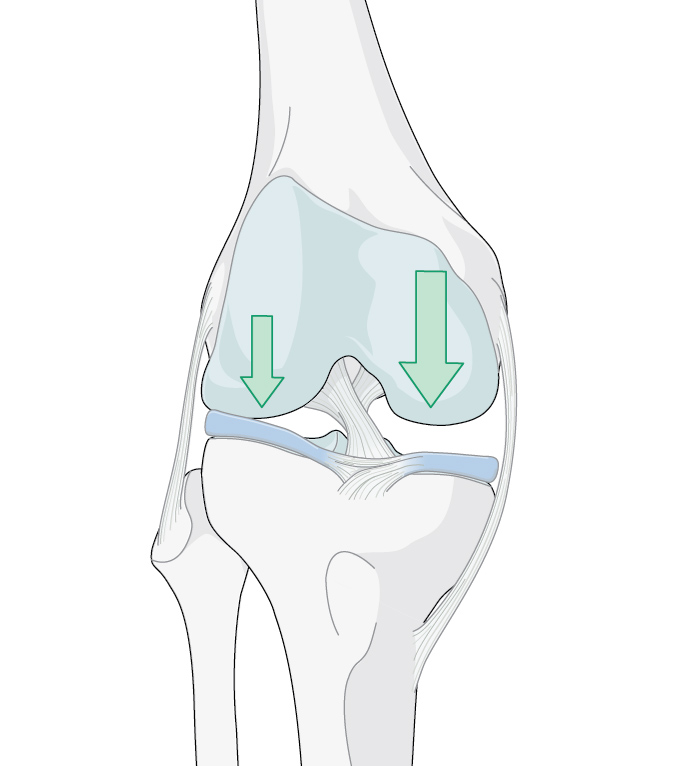
Each step you take sends forces that amount to three to eight times your body weight between your femur and tibia, through your knee [1]. Considering this, it is no wonder that the most common type of arthritis is osteoarthritis (OA) of the knee [2]. It is associated with “wear and tear”, injury, and genetic predisposition, and is more likely to occur in people over 50 years old (although younger individuals can also have OA) [3]. Surgical treatment options are available that aim to support improved mobility, reduce pain, and facilitate active lives, including sports—which is a priority, especially for many younger people with knee OA.
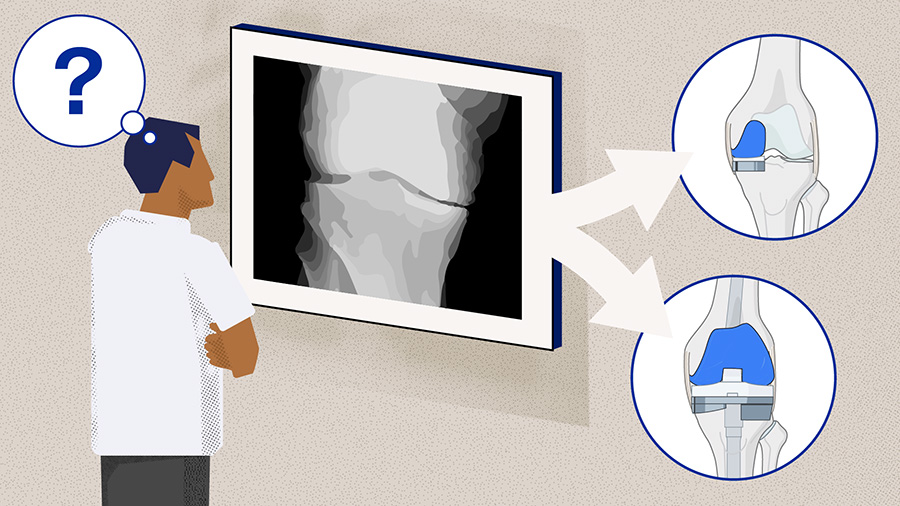
Three procedures that seek to surgically manage degenerative OA are HTO, UKA, and total knee arthroplasty (TKA). Successful HTO and UKA can delay a TKA, allowing patients to retain more aspects of their native knee(s) for longer [4, 5].
As Georg Matziolis, Chief Physician at the German Centre for Orthopedics in Eisenberg, Germany, points out, “TKA has the best long-term survival of all the options but the worst functional outcomes and patient reported outcomes measures (PROMs). TKA replaces all compartments (medial, lateral, and patellofemoral) and is therefore indicated for end-stage arthritis in a minimum of two compartments. If arthritis is secondary to systemic diseases such as rheumatoid arthritis, gout, and pseudogout, TKA is recommended even if only one knee compartment seems to be affected.”

Georg Matziolis
Waldkliniken Eisenberg—German Center of Orthopedics
Eisenberg, Germany
Part 1 explored UKA in relation to TKA. This article focuses on similar questions applied to HTO and UKA, comparing these two procedures and examining the indications that would prompt surgeons to select one over the other.
Matziolis reminds us that, “HTO, UKA, and TKA are all viable options to treat degenerative arthritis of the knee but each of these procedures is appropriate for different kinds and degrees of OA.”
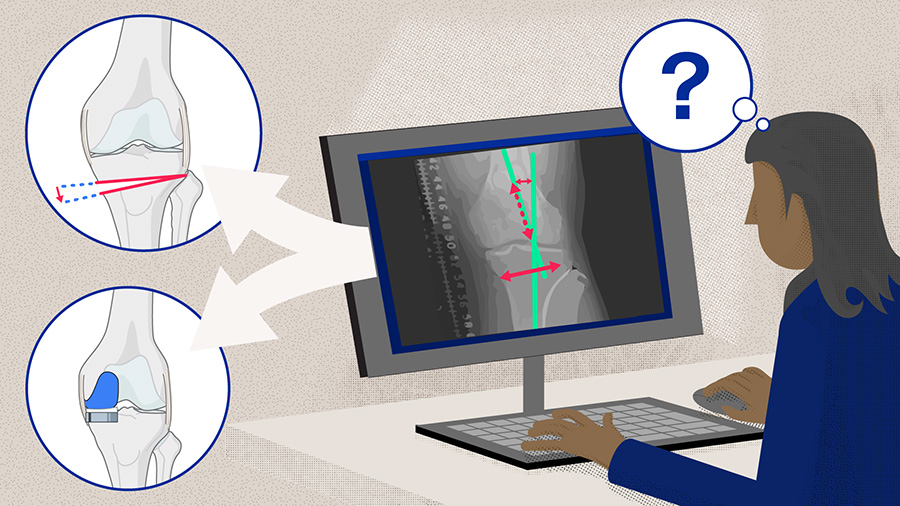
Figure 1. TKA, HTO, and UKA are all viable options to address osteoarthritis of the knee. However, there are situations that indicate the selection of one over the others.
HTO
Since 1958, when the procedure was first performed by Jackson [6], and popularized by Coventry [7] starting in the 1960s [8], HTO has been used to treat unicompartmental OA in knees. Whereas UKA and TKA replace elements of the knee joint with prostheses, either in part or in full, respectively, HTO takes a biomechanical approach and is viewed as a realignment procedure. “HTO does not replace the knee joint but optimizes the joint biomechanics by reducing the pressure on one compartment,” says Georg Matziolis. Patient-specific alignment is widely recognized as “the foundation step when planning any surgical intervention” [9].
It is not only a useful treatment for certain cases of single compartment knee OA, but also knee instability. It is sometimes paired with ligament reconstruction (anterior cruciate ligament [ACL]) to address stability issues [10]. Generally, ACL reconstruction accompanies an HTO if there is a posterior slope of more than 12° or severe varus malalignment [11].
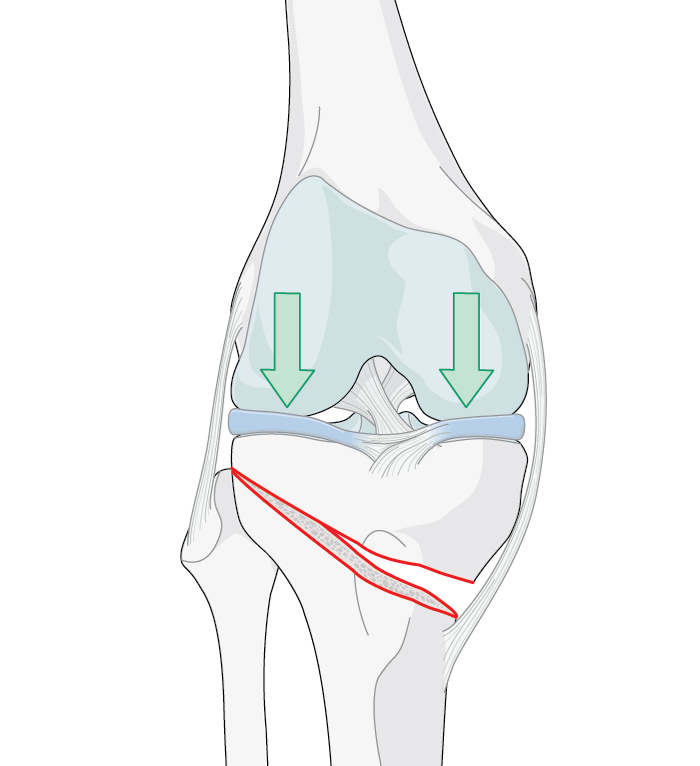
Figure 2. Arrows indicate the load distribution before (left) and after (center) the procedure (medial open wedge osteotomy with locked plate osteosynthesis)(right). Used under CC BY-SA 3.0 de license. Source. Image (right) by J Lengerke.
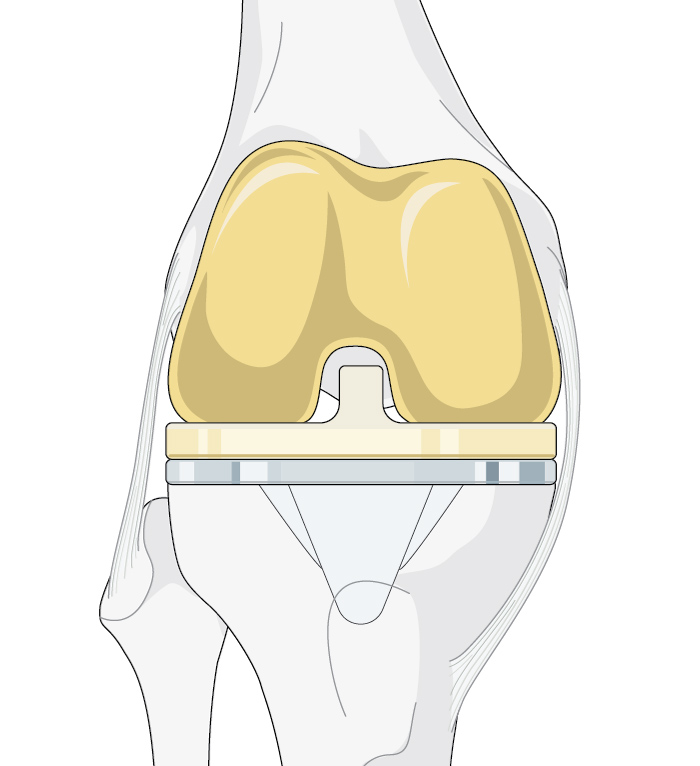
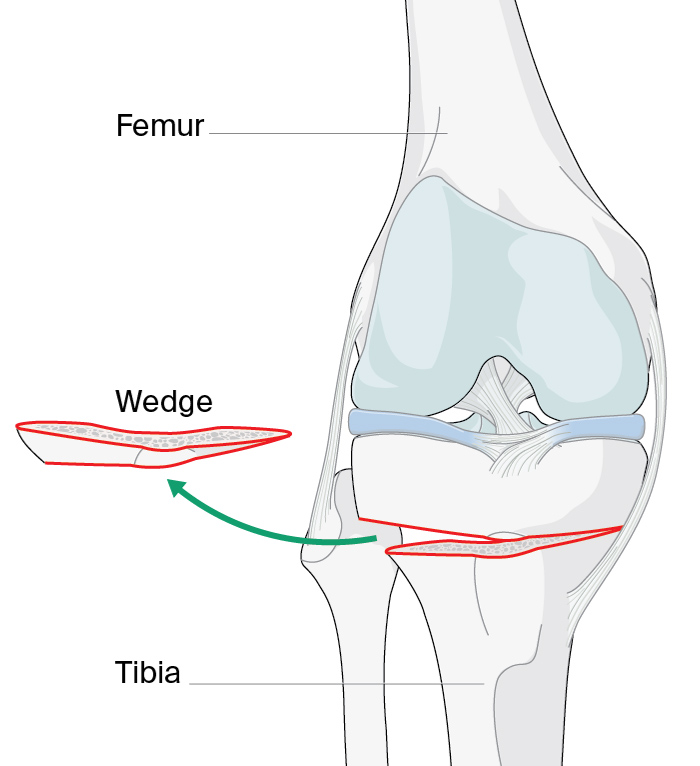
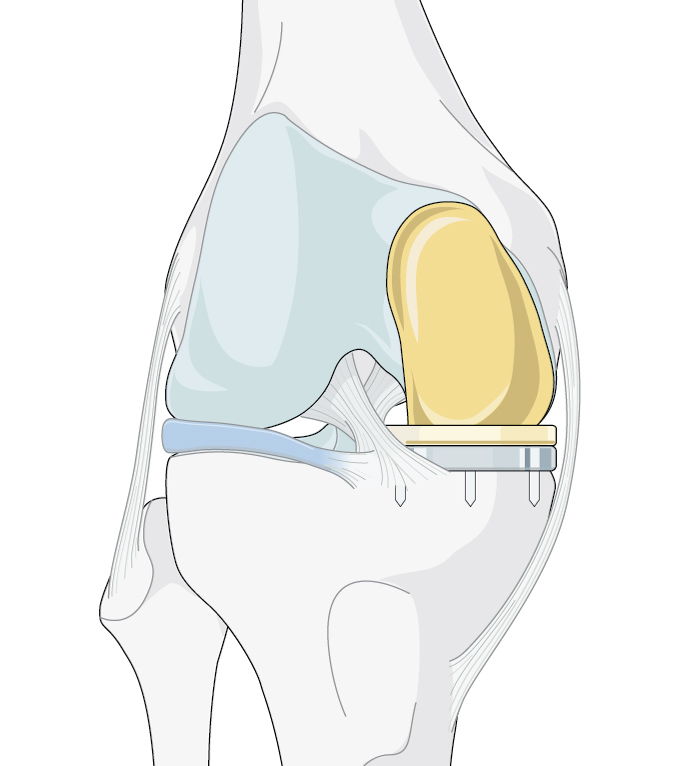
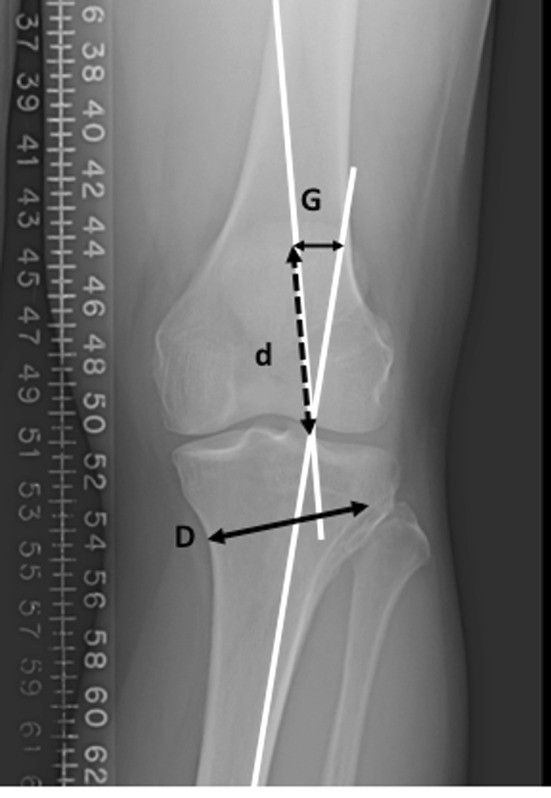
A wedge-shaped cut (see Figure 1) is made in the top of the tibia to change the alignment of the knee by shifting the weight/loading of the arthritic part of the joint to the healthier part (see Figure 2) [12]. It is mostly performed for varus deformities, less commonly for valgus deformities [13]. Preoperative planning using imaging helps surgeons to calculate the size of the wedge/osteotomy needed to correct the weight-bearing axis (see Figure 3). For best results, it is critical that correct alignment is achieved [14]. There is controversy around what constitutes the ideal mechanical alignment but generally the recommended alignment range is between 2° and 6° of mechanical valgus [15].
Figure 3. Line D shows the distance of the proposed osteotomy site and the same length (line d) is drawn over one of the mechanical axes. The distance between the two mechanical axes at this point (line G) indicates what size of the gap at the posterior aspect of the osteotomy should be in order to correct the weight-bearing axis to the correction point. Used under CC BY 4.0 license. Source: Herman BV, Giffin JR. High tibial osteotomy in the ACL-deficient knee with medial compartment osteoarthritis. J Orthop Traumatol. 2016 Sep;17(3):277–285.
Read the full article with your AO login
- HTO: closed wedge or open wedge
- HTO: Which patients benefits most?
- HTO and cartilage regeneration: a helping hand
- HTO: What are the drawbacks?
- UKA
- UKA: fixed and mobile bearings
- UKA: Which patients are best suited?
- UKA: potential complications
- UKA or HTO: Which one to use?
- Consideration of future risk
- Appropriate Use Criteria
- In summary
- References
More AO resources
Access videos, tools, and other assets to learn more about this topic:
- AO Surgery Reference
- AO Videos (AO login required)
- AO Course finder
- AO Classification (UCS) (PDF)
- AO E-book
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Jean-Noël Argenson
University Hospital of Marseille
Marseille, France

Robert Hube
OCM—Orthopedic Surgery Center Munich
Munich, Germany

Georg Matziolis
Waldkliniken Eisenberg—German Center of Orthopedics
Eisenberg, Germany
This issue was created by Word+Vision Media Productions, Switzerland
References
- Hospital for Special Surgery. Knee surgery: High tibial osteotomy. https://www.hss.edu/conditions_knee-surgery-high-tibial-osteotomy.asp. Published 2018. Accessed August 1, 2020.
- Harvard Men‘s Health Watch. Moving away from knee osteoarthritis. Harvard Health Publishing. https://www.health.harvard.edu/pain/moving-away-from-knee-osteoarthritis. Published 2018. Accessed July 22, 2020.
- OrthoInfo. Arthritis of the knee. American Academy of Orthopedic Surgeons. https://orthoinfo.aaos.org/en/diseases--conditions/arthritis-of-the-knee/. Updated June 2014. Accessed July 22, 2020.
- Jones GG, Jaere M, Clarke S, et al. 3D printing and high tibial osteotomy. EFORT Open Rev. 2018 May;3(5):254–259.
- Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am. 1993 Feb;75(2):196–201.
- Jackson JP. Osteotomy for osetoarthritis of the knee. J Bone Joint Surg Br. 1958 40.
- Coventry MB. OSTEOTOMY OF THE UPPER PORTION OF THE TIBIA FOR DEGENERATIVE ARTHRITIS OF THE KNEE. A PRELIMINARY REPORT. J Bone Joint Surg Am. 1965 Jul;47:984–990.
- Herman BV, Giffin JR. High tibial osteotomy in the ACL-deficient knee with medial compartment osteoarthritis. J Orthop Traumatol. 2016 Sep;17(3):277–285.
- Smith JO, Wilson AJ, Thomas NP. Osteotomy around the knee: evolution, principles and results. Knee Surg Sports Traumatol Arthrosc. 2013 Jan;21(1):3–22.
- McNamara I, Birmingham TB, Fowler PJ, et al. High tibial osteotomy: evolution of research and clinical applications--a Canadian experience. Knee Surg Sports Traumatol Arthrosc. 2013 Jan;21(1):23–31.
- Gupta A, Tejpal T, Shanmugaraj A, et al. Surgical Techniques, Outcomes, Indications, and Complications of Simultaneous High Tibial Osteotomy and Anterior Cruciate Ligament Revision Surgery: A Systematic Review. Hss j. 2019 Jul;15(2):176–184.
- RebalanceMD. High Tibial Osteotomy: A Guide to Recovery After Surgery. Musculoskeletal Care Ltd. http://rebalancemd.com/wp-content/uploads/2017/08/HTO_Recovery_Guide.pdf. Published 2015. Accessed August 2, 2020.
- Abbasai D. OrthoBullets: High Tibial Osteotomy. Lineage Medical Inc. https://www.orthobullets.com/recon/3135/high-tibial-osteotomy. Updated July 16, 2020. Accessed August 1, 2020.
- Dettoni F, Bonasia DE, Castoldi F, et al. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J. 2010 30:131–140.
- Tunggal JA, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy. Int Orthop. 2010 Feb;34(2):255–261.
- Liu X, Chen Z, Gao Y, et al. High Tibial Osteotomy: Review of Techniques and Biomechanics. J Healthc Eng. 2019 2019:8363128.
- Aglietti P, Rinonapoli E, Stringa G, et al. Tibial osteotomy for the varus osteoarthritic knee. Clin Orthop Relat Res. 1983 Jun;(176):239–251.
- Hernigou P, Medevielle D, Debeyre J, et al. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987 Mar;69(3):332–354.
- Holden DL, James SL, Larson RL, et al. Proximal tibial osteotomy in patients who are fifty years old or less. A long-term follow-up study. J Bone Joint Surg Am. 1988 Aug;70(7):977–982.
- Sabzevari S, Ebrahimpour A, Roudi MK, et al. High Tibial Osteotomy: A Systematic Review and Current Concept. Arch Bone Jt Surg. 2016 Jun;4(3):204–212.
- Lobenhoffer P, Agneskirchner JD. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2003 May;11(3):132–138.
- Brinkman JM, Lobenhoffer P, Agneskirchner JD, et al. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br. 2008 Dec;90(12):1548–1557.
- Yasuda K, Majima T, Tsuchida T, et al. A ten- to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis. Clin Orthop Relat Res. 1992 Sep;(282):186–195.
- Agarwala S, Sobti A, Naik S, et al. Comparison of closing-wedge and opening-wedge high tibial osteotomies for medial compartment osteoarthritis of knee in Asian population: Mid-term follow-up. J Clin Orthop Trauma. 2016 Oct-Dec;7(4):272–275.
- Tabrizi A, Soleimanpour J, Sadighi A, et al. A short term follow up comparison of genu varum corrective surgery using open and closed wedge high tibial osteotomy. Malays Orthop J. 2013 Mar;7(1):7–12.
- Smith TO, Sexton D, Mitchell P, et al. Opening- or closing-wedged high tibial osteotomy: a meta-analysis of clinical and radiological outcomes. Knee. 2011 Dec;18(6):361–368.
- Sun H, Zhou L, Li F, et al. Comparison between Closing-Wedge and Opening-Wedge High Tibial Osteotomy in Patients with Medial Knee Osteoarthritis: A Systematic Review and Meta-analysis. J Knee Surg. 2017 Feb;30(2):158–165.
- Han SB, Kyung HS, Seo IW, et al. Better clinical outcomes after unicompartmental knee arthroplasty when comparing with high tibial osteotomy. Medicine (Baltimore). 2017 Dec;96(50):e9268.
- Malinowski K, Sibilska A, Góralczyk A, et al. Superficial Medial Collateral Ligament Reattachment During High Tibial Osteotomy: Regulate Tension, Preserve Stability! Arthrosc Tech. 2019 Nov;8(11):e1339–e1343.
- van Egmond N, Hannink G, Janssen D, et al. Relaxation of the MCL after an Open-Wedge High Tibial Osteotomy results in decreasing contact pressures of the knee over time. Knee Surg Sports Traumatol Arthrosc. 2017 Mar;25(3):800–807.
- van Lieshout WAM, Martijn CD, van Ginneken BTJ, et al. Medial collateral ligament laxity in valgus knee deformity before and after medial closing wedge high tibial osteotomy measured with instrumented laxity measurements and patient reported outcome. J Exp Orthop. 2018 Dec 10;5(1):49.
- Konopka JF, Gomoll AH, Thornhill TS, et al. The cost-effectiveness of surgical treatment of medial unicompartmental knee osteoarthritis in younger patients: a computer model-based evaluation. J Bone Joint Surg Am. 2015 May 20;97(10):807–817.
- Santoso MB, Wu L. Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review. J Orthop Surg Res. 2017 Mar 28;12(1):50.
- Flecher X, Parratte S, Aubaniac JM, et al. A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res. 2006 Nov;452:91–96.
- Gstöttner M, Pedross F, Liebensteiner M, et al. Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg. 2008 Jan;128(1):111–115.
- Niinimäki TT, Eskelinen A, Mann BS, et al. Survivorship of high tibial osteotomy in the treatment of osteoarthritis of the knee: Finnish registry-based study of 3195 knees. J Bone Joint Surg Br. 2012 Nov;94(11):1517–1521.
- Trieb K, Grohs J, Hanslik-Schnabel B, et al. Age predicts outcome of high-tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2006 Feb;14(2):149–152.
- Witjes S, Gouttebarge V, Kuijer PP, et al. Return to Sports and Physical Activity After Total and Unicondylar Knee Arthroplasty: A Systematic Review and Meta-Analysis. Sports Med. 2016 Feb;46(2):269–292.
- Khan M, Adili A, Winemaker M, et al. Management of osteoarthritis of the knee in younger patients. Cmaj. 2018 Jan 22;190(3):e72–e79.
- van Zaanen Y, van Geenen RCI, Pahlplatz TMJ, et al. Three Out of Ten Working Patients Expect No Clinical Improvement of Their Ability to Perform Work-Related Knee-Demanding Activities After Total Knee Arthroplasty: A Multicenter Study. J Occup Rehabil. 2019 Sep;29(3):585–594.
- Jacquet C, Gulagaci F, Schmidt A, et al. Opening wedge high tibial osteotomy allows better outcomes than unicompartmental knee arthroplasty in patients expecting to return to impact sports. Knee Surg Sports Traumatol Arthrosc. 2020 Feb 1.
- Hoorntje A, Kuijer P, van Ginneken BT, et al. Predictors of Return to Work After High Tibial Osteotomy: The Importance of Being a Breadwinner. Orthop J Sports Med. 2019 Dec;7(12):2325967119890056.
- Messier SP, Gutekunst DJ, Davis C, et al. Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum. 2005 Jul;52(7):2026–2032.
- Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop. 2010 Feb;34(2):155–160.
- Naudie D, Bourne RB, Rorabeck CH, et al. The Install Award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin Orthop Relat Res. 1999 Oct;(367):18–27.
- Akizuki S, Shibakawa A, Takizawa T, et al. The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Joint Surg Br. 2008 May;90(5):592–596.
- Howells NR, Salmon L, Waller A, et al. The outcome at ten years of lateral closing-wedge high tibial osteotomy: determinants of survival and functional outcome. Bone Joint J. 2014 Nov;96-b(11):1491–1497.
- Loia MC, Vanni S, Rosso F, et al. High tibial osteotomy in varus knees: indications and limits. Joints. 2016 Apr-Jun;4(2):98–110.
- Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000 May-Jun;28(3):282–296.
- Rossi R, Bonasia DE, Amendola A. The role of high tibial osteotomy in the varus knee. J Am Acad Orthop Surg. 2011 Oct;19(10):590–599.
- Savarese E, Bisicchia S, Romeo R, et al. Role of high tibial osteotomy in chronic injuries of posterior cruciate ligament and posterolateral corner. J Orthop Traumatol. 2011 Mar;12(1):1–17.
- Badhe NP, Forster IW. High tibial osteotomy in knee instability: the rationale of treatment and early results. Knee Surg Sports Traumatol Arthrosc. 2002 Jan;10(1):38–43.
- Berman AT, Bosacco SJ, Kirshner S, et al. Factors influencing long-term results in high tibial osteotomy. Clin Orthop Relat Res. 1991 Nov;(272):192–198.
- Bonasia DE, Dettoni F, Sito G, et al. Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med. 2014 Mar;42(3):690–698.
- Knipe H, Mudgal P. Ahlbäck classification of knee osteoarthritis. Radiopaedia.org. https://radiopaedia.org/articles/ahlback-classification-of-knee-osteoarthritis. Accessed August 3, 2020.
- Makris EA, Gomoll AH, Malizos KN, et al. Repair and tissue engineering techniques for articular cartilage. Nat Rev Rheumatol. 2015 Jan;11(1):21–34.
- Song JS, Hong KT, Kong CG, et al. High tibial osteotomy with human umbilical cord blood-derived mesenchymal stem cells implantation for knee cartilage regeneration. World J Stem Cells. 2020 Jun 26;12(6):514–526.
- Wu LD, Hahne HJ, Hassenpflug T. A long-term follow-up study of high tibial osteotomy for medial compartment osteoarthrosis. Chin J Traumatol. 2004 Dec;7(6):348–353.
- Aglietti P, Buzzi R, Vena LM, et al. High tibial valgus osteotomy for medial gonarthrosis: a 10- to 21-year study. J Knee Surg. 2003 Jan;16(1):21–26.
- Bauer T, Hardy P, Lemoine J, et al. Drop foot after high tibial osteotomy: a prospective study of aetiological factors. Knee Surg Sports Traumatol Arthrosc. 2005 Jan;13(1):23–33.
- van Raaij TM, Brouwer RW, de Vlieger R, et al. Opposite cortical fracture in high tibial osteotomy: lateral closing compared to the medial opening-wedge technique. Acta Orthop. 2008 Aug;79(4):508–514.
- Sprenger TR, Doerzbacher JF. Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Joint Surg Am. 2003 Mar;85(3):469–474.
- Campbell WC. Interposition of vitallium plates in arthroplasties of the knee: preliminary report. Am J Surg. 1940 47:639–641.
- Marmor L. Marmor modular knee in unicompartmental disease. Minimum four-year follow-up. J Bone Joint Surg Am. 1979 Apr;61(3):347–353.
- Bruni D, Iacono F, Akkawi I, et al. Unicompartmental knee replacement: a historical overview. Joints. 2013 Apr-Jun;1(2):45–47.
- Rodríguez-Merchán EC, Gómez-Cardero P. Unicompartmental knee arthroplasty: Current indications, technical issues and results. EFORT Open Rev. 2018 Jun;3(6):363–373.
- Ollivier M, Abdel MP, Parratte S, et al. Lateral unicondylar knee arthroplasty (UKA): contemporary indications, surgical technique, and results. Int Orthop. 2014 Feb;38(2):449–455.
- Kendall R. Unicompartmental Knee Arthroplasty: Mobile vs Fixed -Bearing. Orthogate. https://www.orthogate.org/articles/hip-and-knee/unicompartmental-knee-arthroplasty-mobile-vs-fixed-bearing. Published 2006. Accessed August 3, 2020.
- International Congress for Joint Construction. Point/Counterpoint: Which Bearing Type Is Best for UKA? https://icjr.net/articles/pointcounterpoint-which-bearing-type-is-best-for-uka. Published 2015. Accessed August 3, 2020.
- Inoue A, Arai Y, Nakagawa S, et al. Comparison of Alignment Correction Angles Between Fixed-Bearing and Mobile-Bearing UKA. J Arthroplasty. 2016 Jan;31(1):142–145.
- Parratte S, Pauly V, Aubaniac JM, et al. No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2012 Jan;470(1):61–68.
- Zuiderbaan HA, van der List JP, Kleeblad LJ, et al. Modern Indications, Results, and Global Trends in the Use of Unicompartmental Knee Arthroplasty and High Tibial Osteotomy in the Treatment of Isolated Medial Compartment Osteoarthritis. Am J Orthop (Belle Mead NJ). 2016 Sep/Oct;45(6):E355–e361.
- W.Dahl A, Robertsson O, Lidgren L, et al. Unicompartmental knee arthroplasty in patients aged less than 65. Acta Orthop. 2010 Feb;81(1):90–94.
- Panni AS, Vasso M, Cerciello S, et al. Unicompartmental knee replacement provides early clinical and functional improvement stabilizing over time. Knee Surg Sports Traumatol Arthrosc. 2012 Mar;20(3):579–585.
- Vasso M, Antoniadis A, Helmy N. Update on unicompartmental knee arthroplasty: Current indications and failure modes. EFORT Open Rev. 2018 Aug;3(8):442–448.
- Siman H, Kamath AF, Carrillo N, et al. Unicompartmental Knee Arthroplasty vs Total Knee Arthroplasty for Medial Compartment Arthritis in Patients Older Than 75 Years: Comparable Reoperation, Revision, and Complication Rates. J Arthroplasty. 2017 Jun;32(6):1792–1797.
- Koh IJ, Kim MS, Sohn S, et al. Predictive factors for satisfaction after contemporary unicompartmental knee arthroplasty and high tibial osteotomy in isolated medial femorotibial osteoarthritis. Orthop Traumatol Surg Res. 2019 Feb;105(1):77–83.
- Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989 Jan;71(1):145–150.
- Molloy J, Kennedy J, Jenkins C, et al. Obesity should not be considered a contraindication to medial Oxford UKA: long-term patient-reported outcomes and implant survival in 1000 knees. Knee Surg Sports Traumatol Arthrosc. 2019 Jul;27(7):2259–2265.
- Lum ZC, Crawford DA, Lombardi AV, Jr., et al. Early comparative outcomes of unicompartmental and total knee arthroplasty in severely obese patients. Knee. 2018 Jan;25(1):161–166.
- Hernandez NM, Petis SM, Hanssen AD, et al. Infection After Unicompartmental Knee Arthroplasty: A High Risk of Subsequent Complications. Clin Orthop Relat Res. 2019 Jan;477(1):70–77.
- Ji JH, Park SE, Song IS, et al. Complications of medial unicompartmental knee arthroplasty. Clin Orthop Surg. 2014 Dec;6(4):365–372.
- Nwachukwu BU, McCormick FM, Schairer WW, et al. Unicompartmental knee arthroplasty versus high tibial osteotomy: United States practice patterns for the surgical treatment of unicompartmental arthritis. J Arthroplasty. 2014 Aug;29(8):1586–1589.
- Tuncay I, Bilsel K, Elmadağ M, et al. Evaluation of mobile bearing unicompartmental knee arthroplasty, opening wedge, and dome-type high tibial osteotomies for knee arthritis. Acta Orthop Traumatol Turc. 2015 49(3):280–287.
- Cao Z, Mai X, Wang J, et al. Unicompartmental Knee Arthroplasty vs High Tibial Osteotomy for Knee Osteoarthritis: A Systematic Review and Meta-Analysis. J Arthroplasty. 2018 Mar;33(3):952–959.
- Kim MS, Koh IJ, Sohn S, et al. Unicompartmental knee arthroplasty is superior to high tibial osteotomy in post-operative recovery and participation in recreational and sports activities. Int Orthop. 2019 Nov;43(11):2493–2501.
- Petersen W, Metzlaff S. Open wedge high tibial osteotomy (HTO) versus mobile bearing unicondylar medial joint replacement: five years results. Arch Orthop Trauma Surg. 2016 Jul;136(7):983–989.
- Song SJ, Bae DK, Kim KI, et al. Long-term survival is similar between closed-wedge high tibial osteotomy and unicompartmental knee arthroplasty in patients with similar demographics. Knee Surg Sports Traumatol Arthrosc. 2019 Apr;27(4):1310–1319.
- Schlumberger M, Oremek D, Brielmaier M, et al. Prior high tibial osteotomy is not a contraindication for medial unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020 Jul 15.
- El-Galaly A, Nielsen PT, Kappel A, et al. Reduced survival of total knee arthroplasty after previous unicompartmental knee arthroplasty compared with previous high tibial osteotomy: a propensity-score weighted mid-term cohort study based on 2,133 observations from the Danish Knee Arthroplasty Registry. Acta Orthop. 2020 Apr;91(2):177–183.
- Lee YS, Kim HJ, Mok SJ, et al. Similar Outcome, but Different Surgical Requirement in Conversion Total Knee Arthroplasty following High Tibial Osteotomy and Unicompartmental Knee Arthroplasty: A Meta-Analysis. J Knee Surg. 2019 Jul;32(7):686–700.
- Robertsson O, A WD. The risk of revision after TKA is affected by previous HTO or UKA. Clin Orthop Relat Res. 2015 Jan;473(1):90–93.
- Ahmed GO, K EL, Ahmed AF. Usability of the AAOS Appropriate Use Criteria (AUC) for the surgical management of knee osteoarthritis in clinical practice. Knee Surg Sports Traumatol Arthrosc. 2020 Jul;28(7):2077–2081.
- Riddle DL, Perera RA. Appropriateness and total knee arthroplasty: an examination of the American Academy of Orthopaedic Surgeons appropriateness rating system. Osteoarthritis Cartilage. 2017 Dec;25(12):1994–1998.
- Rodriguez-Merchan EC. Unicompartmental Knee Osteoarthritis (UKOA): Unicompartmental Knee Arthroplasty (UKA) or High Tibial Osteotomy (HTO)? Arch Bone Jt Surg. 2016 Oct;4(4):307–313.