Unicompartmental knee arthroplasties: Tips and tricks
Preview
The number of unicompartmental knee arthroplasties (UKAs) being performed is increasing. This is due in part to the prevalence of osteoarthritis and expanded indications for the procedure. UKA poses technical demands that requires experience and surgical frequency for best outcomes. Surgeons should keep proper patient selection, biomechanics, and alignment front of mind when undertaking an UKA.
Unicompartmental knee arthroplasty (UKA) is less forgiving in terms of surgical error and surgeons need sufficient training and experience for good results—this is only achieved with a significant annual volume of procedures.
Robert Hube, Professor of Orthopedic Surgery Charité—University Medicine, Berlin, Germany, and Past President of the German Knee Society, acknowledges the challenges but also asserts that it is possible to achieve excellent UKA outcomes. “The surgical priorities for UKAs are achieving the correct alignment based on preoperative planning, correctly positioning the components, and securing sufficient fixation of the implants.”

Robert Hube
OCM—Orthopedic Surgery Center Munich
Munich, Germany
Patient selection is key
As discussed in Part 1 and Part 2 of this article series, proper patient selection is critical for UKA success. Over time, indications and contraindications for the procedure have evolved from patient characteristics such as body mass index (BMI) and age, among others [1] to the consideration of more pathoanatomical indications.
To see if published contraindications to UKA actually generated poorer outcomes, Hamilton et al looked at 1000 mobile-bearing UKAs (818 patients), comparing the outcomes at 10- and 15-years follow-up of 322 traditionally indicated knees and 678 contraindicated knees. They concluded that for their study group, there was “evidence that patients with the previously reported contraindications do as well as, or even better than, those without contraindications” [2].
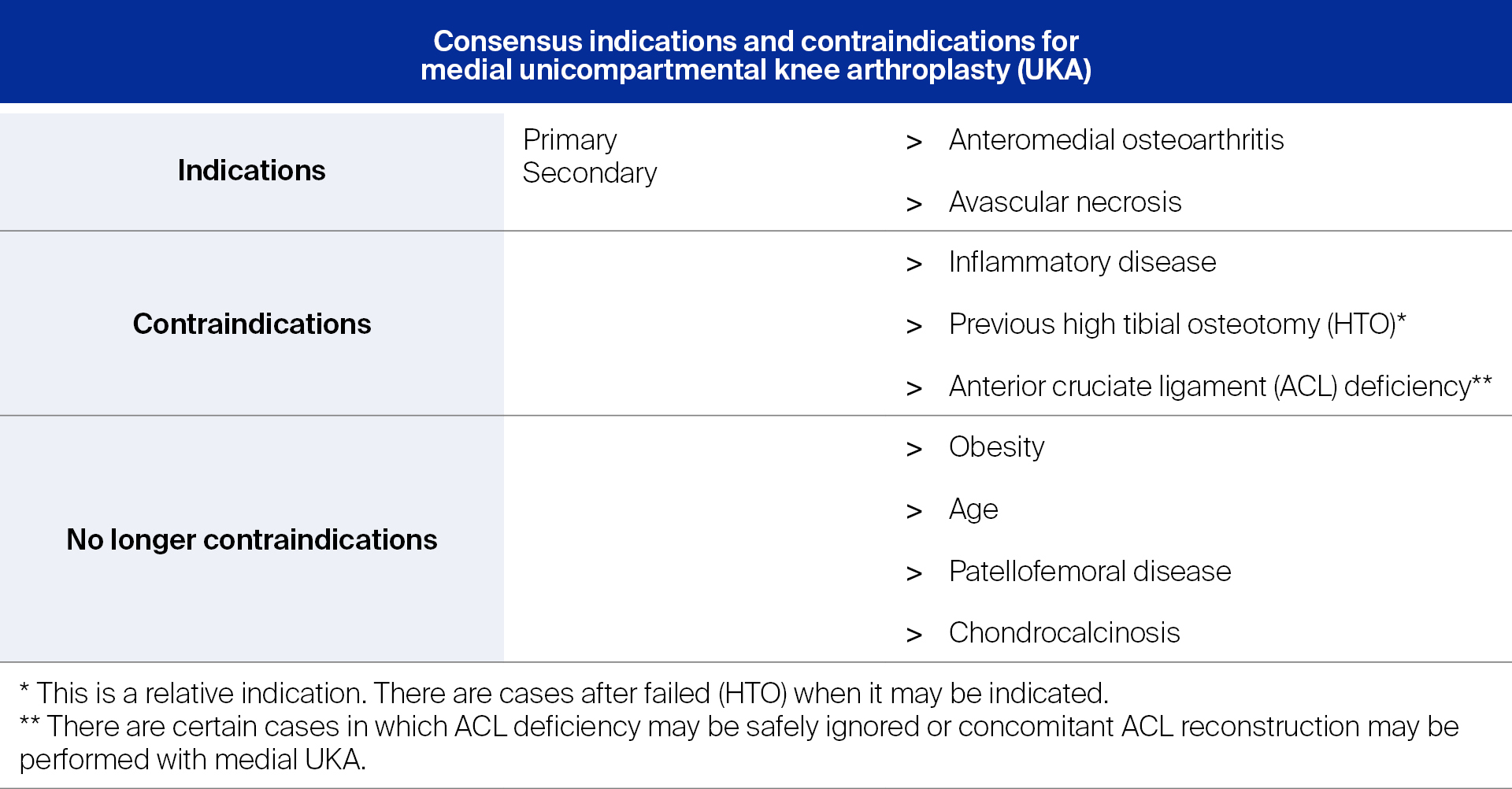
In 2015, six surgeons with combined experience of 8,000 UKAs (representing between 10% to 50% of their primary knee practices) published a consensus statement in the Journal of Surgical Orthopedic Advances on the indications and contraindications for medial UKA (see Table 1).
All the same, consensus is no substitute for a surgeon’s experience and does not take into account the need for patients to be involved in the decision-making to a certain degree. When choosing between options, for example UKA or total knee arthroplasty (TKA), lifestyle, activity levels, scarring, and other factors may be weighted differently by a patient than by their surgeon [3].
Does anterior cruciate ligament stability make a difference?
On the matter of the stability of the anterior cruciate ligament (ACL), Robert Hube says, “A successful UKA requires a stable knee. If the muscles have compensated for the compromised ACL, and the knee is about functionally stable, in my opinion the patient is still a candidate for a UKA.”
A cadaveric study of 15 knees looked how fixed-bearing UKA in ACL-intact, partial ACL, and ACL-deficient knees would affect the posterior tibial slope’s restoration of knee stability and flexion. The researchers determined that a slope of just 1° in ACL-deficient knees almost doubled the degree of translation compared to ACL-intact knees, leading them to conclude that UKA in ACL-deficient knees was “challenging” [4].
Of course, UKA is not limited to the medial compartment; lateral UKA accounts for roughly 10% of cases [5]. In this situation, Robert Hube says that there is insufficient data to indicate whether medial or lateral UKA is a better candidate if there is also a compromised ACL. “If the knee is functionally stable, I would go for both, medial and lateral UKA. The problem is that most of the knees with a deficient ACL are not stable. In these cases, we would go for a TKA. However, this is in contrast to data for high tibia osteotomies. Here, we can achieve good results even with insufficient ACL.”
Even if the “right” patients are selected for UKA, another important factor that has been shown to impact outcomes: surgeon experience.
Read the full article with your AO login
- Surgeon experience makes a difference
- Preoperative planning to limit intraoperative decisions
- Mobile or fixed bearing?
- Biomechanical basics
- Proper sizing and positioning are important
- Undercorrect is correct
- A word on osteophytes
- Tibial slope considerations
- Fixation
- In summary
- References
More AO resources
Access videos, tools, and other assets to learn more about this topic:
- AO Surgery Reference
- AO Videos (AO login required)
- AO Course finder
- AO Classification (UCS) (PDF)
- AO E-book
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Jean-Noël Argenson
University Hospital of Marseille
Marseille, France

Robert Hube
OCM—Orthopedic Surgery Center Munich
Munich, Germany

Georg Matziolis
Waldkliniken Eisenberg—German Center of Orthopedics
Eisenberg, Germany
This issue was created by Word+Vision Media Productions, Switzerland
References
- Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989 Jan;71(1):145–150.
- Hamilton TW, Pandit HG, Jenkins C, et al. Evidence-Based Indications for Mobile-Bearing Unicompartmental Knee Arthroplasty in a Consecutive Cohort of Thousand Knees. J Arthroplasty. 2017 Jun;32(6):1779–1785.
- Wilson HA, Middleton R, Abram SGF, et al. Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ. 2019 Feb 21;364:l352.
- Adulkasem N, Rojanasthien S, Siripocaratana N, et al. Posterior tibial slope modification in osteoarthritis knees with different ACL conditions: Cadaveric study of fixed-bearing UKA. J Orthop Surg (Hong Kong). 2019 May-Aug;27(2):2309499019836286.
- Sah AP, Scott RD. Lateral unicompartmental knee arthroplasty through a medial approach. Study with an average five-year follow-up. J Bone Joint Surg Am. 2007 Sep;89(9):1948–1954.
- Bini S, Khatod M, Cafri G, et al. Surgeon, implant, and patient variables may explain variability in early revision rates reported for unicompartmental arthroplasty. J Bone Joint Surg Am. 2013 Dec 18;95(24):2195–2202.
- Liddle AD, Pandit H, Judge A, et al. Effect of Surgical Caseload on Revision Rate Following Total and Unicompartmental Knee Replacement. J Bone Joint Surg Am. 2016 Jan 6;98(1):1–8.
- Baker P, Jameson S, Critchley R, et al. Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am. 2013 Apr 17;95(8):702–709.
- Murray DW, Liddle AD, Dodd CA, et al. Unicompartmental knee arthroplasty: is the glass half full or half empty? Bone Joint J. 2015 Oct;97-b(10 Suppl A):3–8.
- Liddle A, Pandit H, Judge A, et al. Optimizing Outcomes Following Unicompartmental Knee Replacement: Insights from a Study of 25,982 Cases (Scientific Exhibit SE11) [abstract]. American Academy of Orthopaedic Surgeons Annual Meeting; 2015.
- Liddle AD, Pandit H, Judge A, et al. Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. Bone Joint J. 2015 Nov;97-b(11):1506–1511.
- Hamilton TW, Rizkalla JM, Kontochristos L, et al. The Interaction of Caseload and Usage in Determining Outcomes of Unicompartmental Knee Arthroplasty: A Meta-Analysis. J Arthroplasty. 2017 Oct;32(10):3228–3237.e3222.
- Robertsson O, Knutson K, Lewold S, et al. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br. 2001 Jan;83(1):45–49.
- Schraknepper J, Dimitriou D, Helmy N, et al. Influence of patient selection, component positioning and surgeon‘s caseload on the outcome of unicompartmental knee arthroplasty. Arch Orthop Trauma Surg. 2020 Jun;140(6):807–813.
- Jones GG, Logishetty K, Clarke S, et al. Do patient-specific instruments (PSI) for UKA allow non-expert surgeons to achieve the same saw cut accuracy as expert surgeons? Arch Orthop Trauma Surg. 2018 Nov;138(11):1601–1608.
- Naziri Q, Mixa PJ, Murray DP, et al. Robotic-Assisted and Computer-Navigated Unicompartmental Knee Arthroplasties: A Systematic Review. Surg Technol Int. 2018 Jun 1;32:271–278.
- van der List JP, Chawla H, Joskowicz L, et al. Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016 Nov;24(11):3482–3495.
- Sousa PL, Sculco PK, Mayman DJ, et al. Robots in the Operating Room During Hip and Knee Arthroplasty. Curr Rev Musculoskelet Med. 2020 Jun;13(3):309–317.
- Begum FA, Kayani B, Morgan SDJ, et al. Robotic technology: current concepts, operative techniques and emerging uses in unicompartmental knee arthroplasty. EFORT Open Rev. 2020 May;5(5):312–318.
- Atesok K, Galos D, Jazrawi LM, et al. Preoperative Planning in Orthopaedic Surgery. Current Practice and Evolving Applications. Bull Hosp Jt Dis (2013). 2015 Dec;73(4):257–268.
- Steinberg EL, Segev E, Drexler M, et al. Preoperative Planning of Orthopedic Procedures using Digitalized Software Systems. Isr Med Assoc J. 2016 Jun;18(6):354–358.
- Cao Z, Niu C, Gong C, et al. Comparison of Fixed-Bearing and Mobile-Bearing Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis. J Arthroplasty. 2019 Dec;34(12):3114–3123.e3113.
- Ashraf T, Newman JH, Desai VV, et al. Polyethylene wear in a non-congruous unicompartmental knee replacement: a retrieval analysis. Knee. 2004 Jun;11(3):177–181.
- Li MG, Yao F, Joss B, et al. Mobile vs. fixed bearing unicondylar knee arthroplasty: A randomized study on short term clinical outcomes and knee kinematics. Knee. 2006 Oct;13(5):365–370.
- Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am. 2002 Dec;84(12):2235–2239.
- Burger JA, Kleeblad LJ, Sierevelt IN, et al. Bearing design influences short- to mid-term survivorship, but not functional outcomes following lateral unicompartmental knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2019 Jul;27(7):2276–2288.
- Emerson RH, Jr., Higgins LL. Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am. 2008 Jan;90(1):118–122.
- Lewold S, Goodman S, Knutson K, et al. Oxford meniscal bearing knee versus the Marmor knee in unicompartmental arthroplasty for arthrosis. A Swedish multicenter survival study. J Arthroplasty. 1995 Dec;10(6):722–731.
- Gleeson RE, Evans R, Ackroyd CE, et al. Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Knee. 2004 Oct;11(5):379–384.
- Emerson R, Hansborough T, Reitman R, et al. Comparison of a Mobile With a Fixed-Bearing Unicompartmental Knee Implant. Knee Society Meeting 2002; 2002.
- Hube R, Keim M. [Minimally invasive implantation in unicondylar arthroplasty]. Orthopade. 2007 Dec;36(12):1093–1099.
- Matziolis G, Tohtz S, Gengenbach B, et al. [Implant with a mobile or a fixed bearing in unicompartmental knee joint replacemen]. Orthopade. 2007 Dec;36(12):1106–1112.
- Radcliffe GS, Brink RB. Arthroscopic treatment of an impinging mobile bearing in a unicompartmental knee arthroplasty. Arthroscopy. 2004 Jul;20 Suppl 2:25–27.
- Hopgood P, Martin CP, Rae PJ. The effect of tibial implant size on post-operative alignment following medial unicompartmental knee replacement. Knee. 2004 Oct;11(5):385–388.
- Vecchini E, Ditta A, Gelmini M, et al. Rupture of the femoral component and severe metallosis of the knee 10 years after unicompartmental knee arthroplasty (UKA): a case report. Acta Biomed. 2019 Jan 10;90(1-s):198–202.
- Chatellard R, Sauleau V, Colmar M, et al. Medial unicompartmental knee arthroplasty: does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res. 2013 Jun;99(4 Suppl):S219–S225.
- Horsager K, Madsen F, Odgaard A, et al. Similar polyethylene wear between cemented and cementless Oxford medial UKA: a 5-year follow-up randomized controlled trial on 79 patients using radiostereometry. Acta Orthop. 2019 Feb;90(1):67–73.
- Rivière C, Iranpour F, Auvinet E, et al. Alignment options for total knee arthroplasty: A systematic review. Orthop Traumatol Surg Res. 2017 Nov;103(7):1047–1056.
- Wada K, Hamada D, Takasago T, et al. Native rotational knee kinematics is restored after lateral UKA but not after medial UKA. Knee Surg Sports Traumatol Arthrosc. 2018 Nov;26(11):3438–3443.
- Rivière C, Harman C, Leong A, et al. Kinematic alignment technique for medial OXFORD UKA: An in-silico study. Orthop Traumatol Surg Res. 2019 Feb;105(1):63–70.
- Pongcharoen B, Chanalithichai N. Clinical outcomes of patients with residual medial osteophytes following mobile bearing unicompartmental knee arthroplasty. PLoS One. 2018 13(10):e0205469.
- Ferrari MB, Mannava S, DePhillipo N, et al. Notchplasty for the Arthroscopic Treatment of Limited Knee Extension. Arthrosc Tech. 2017 Jun;6(3):e517–e524.
- Franz A, Boese CK, Matthies A, et al. Mid-Term Clinical Outcome and Reconstruction of Posterior Tibial Slope after UKA. J Knee Surg. 2019 May;32(5):468–474.
- Suzuki T, Ryu K, Kojima K, et al. The Effect of Posterior Tibial Slope on Joint Gap and Range of Knee Motion in Mobile-Bearing Unicompartmental Knee Arthroplasty. J Arthroplasty. 2019 Dec;34(12):2909–2913.
- Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2004 Mar;86(3):506–511.
- Weber P, Woiczinski M, Steinbrück A, et al. Increase in the Tibial Slope in Unicondylar Knee Replacement: Analysis of the Effect on the Kinematics and Ligaments in a Weight-Bearing Finite Element Model. Biomed Res Int. 2018 2018:8743604.
- Schlegel UJ, Siewe J, Delank KS, et al. Pulsed lavage improves fixation strength of cemented tibial components. Int Orthop. 2011 Aug;35(8):1165-1169.
- Campi S, Mellon SJ, Ridley D, et al. Optimal interference of the tibial component of the cementless Oxford Unicompartmental Knee Replacement. Bone Joint Res. 2018 Mar;7(3):226–231.
- Scheele CB, Müller PE, Schröder C, et al. Accuracy of a non-invasive CT-based measuring technique for cement penetration depth in human tibial UKA. BMC Med Imaging. 2019 Jan 21;19(1):9.