Preview
With the increasing number of patients undergoing total knee arthroplasty (TKA) and the significant economic burden associated with revision surgery, prolonging the longevity of TKA implants has become a key driver of innovation in orthopedic surgery. While cemented TKA is still considered the gold standard, the past decade has witnessed a renewed interest in cementless TKA. As evidenced by recent radiostereometric analysis (RSA) studies, modern cementless designs hold promise in extending the lifespan of TKA implants.
In the third of our three-part series, using RSA results from recent TKA studies, David F Dalury from the University of Maryland St Joseph Medical Center will lead us in taking a closer look at the latest advancements of cementless TKA and the significance of RSA data in predicting long-term implant survival.
David F Dalury
University of Maryland St Joseph Medical Center, Baltimore, Maryland, USA
Member AO Recon Education Forum
Optimizing total knee arthroplasty (TKA): the role of RSA measurements
The resurgence of cementless total knee arthroplasty
With the global aging population, the demand for TKA is steadily increasing [1]. The fixation of a knee prosthesis can be cemented, cementless, or hybrid. Cemented fixation is still widely regarded as the reference standard for TKA, with excellent clinical outcomes and implant longevity of up to 20 years [2–4]. Cemented implants rely on primary bone fixation achieved through cement interdigitation into trabecular bone. However, there are concerns regarding long-term failure of cemented TKA due to loss of cement-bone interlock and debonding at the cement-implant interface, particularly in younger, obese, and active patients [5, 6]. The most common cause of late TKA failure is aseptic loosening due to cumulative mechanical stress, abrasion from cement debris, or trabecular resorption [3].
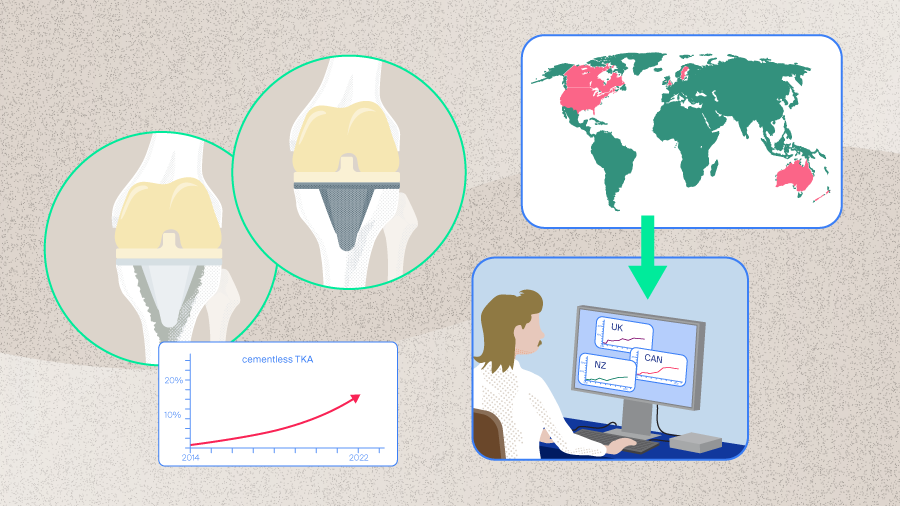
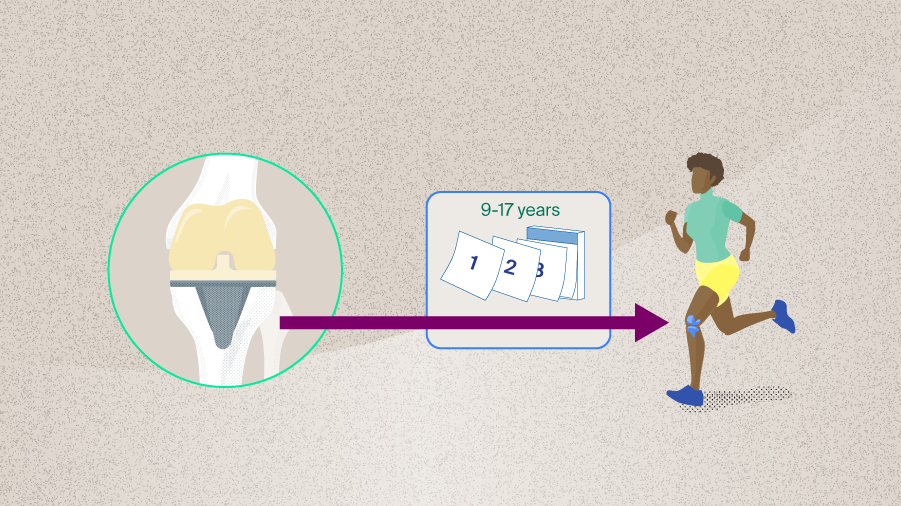
With a growing population of younger, more physically active patients seeking TKA [7], the possibility of long-lasting biological fixation and prolonged implant survival has reignited interest in cementless TKA. Cementless TKA, as opposed to cemented TKA, relies on osseointegration for fixation [8]. This approach aims to provide a more physiological bond between bone and implant, resulting in improved stability and preservation of bone stock for future revisions [4, 5].
First-generation cementless TKA implants faced multiple design-related complications, particularly early aseptic loosening of the tibial component. This loosening was primarily due to factors such as osteolysis, inadequate bone ingrowth into the tibial tray, and micromotion at the bone-implant interface, leading to subsidence—the sinking of the prosthesis into its host bone [9]. However, new designs and, more recently, the integration of 3-dimensional (3D) printing have vastly improved their performance [4]. As introduced in Part 2, modern cementless implants rely on highly porous or roughened surfaces to facilitate bone formation and employ optimized component design to provide a better mechanical interlock, reducing initial micromotion.
Several different modern implants are now available for use in TKA. The latest 3D-printed components are designed to improve the bone-to-metal connection and feature an enhanced porous structure to promote better bone ingrowth, along with peripheral pegs to increase the contact surface area and reduce early micromotion. Some designs exhibit biomechanical properties, such as high compressive strength and elastic modulus, that are very close to those of trabecular bone [10]. These features are thought to facilitate fixation to the host bone, thereby promoting bone ingrowth and increase implant longevity [9–12].
Radiostereometric analysis as a surrogate marker for long-term implant survival
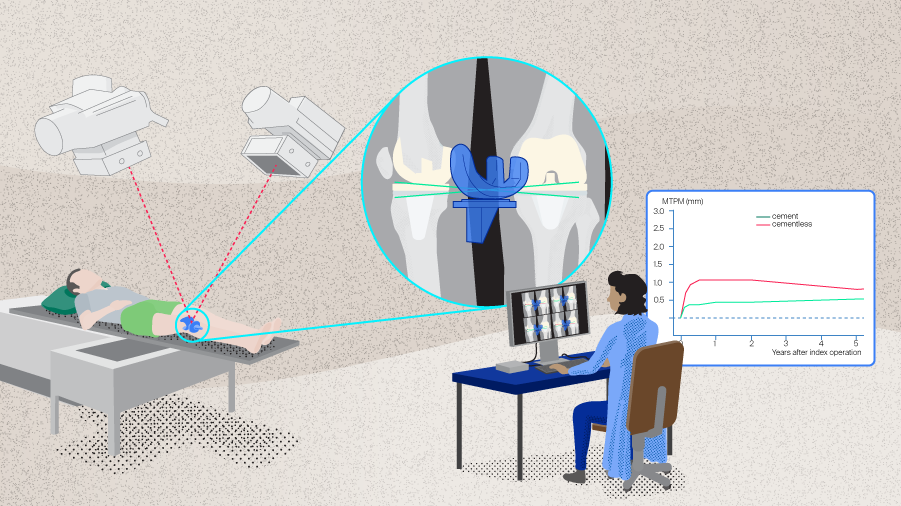
The latest cementless TKA implants have shown promising outcomes in RSA studies. Radiostereometric analysis is a highly accurate imaging technique used to predict implant stability. During the surgical procedure, small radiopaque tantalum markers are implanted in both the bone and the implants. Following surgery, stereoscopic x-rays are taken using a calibration cage with established reference points (Figure 1). These images reveal the positions of the tantalum beads, and when analyzed with an RSA software, they allow surgeons to accurately calculate micromotion between the implant and the bone in three dimensions. By conducting repeated measurements at different time points, RSA allows quantitative analysis of implant migration over time [13]. Given the documented correlation between implant micromotion and the risk of long-term aseptic loosening [14], RSA has emerged as the method of choice for assessing the performance of TKA implants.
Read the full article with your AO login
- Role of RSA measurements
- Radiostereometric analysis – long-term implant survival
- Maximum total point motion migration
- Radiostereometric analysis outcomes
- RSA outcomes of new generation 3D cementless TKA
- Limiting factors for cementless implants
- Conclusion
AO Recon resources
Contributing experts
David F Dalury
University of Maryland St Joseph Medical Center, Baltimore, Maryland, USA
Member AO Recon Education Forum

Bassam Masri
Department of Orthopaedics, University of British Columbia, Vancouver, Canada
Chairperson AO Recon Education Forum and Member AO Recon Steering Board

Gerard A Sheridan
Department of Orthopaedic Surgery, University of Galway, Galway, Ireland
This article was written by Chiara Cianciolo, AO Innovation Translation Center, Clinical Science, Switzerland.
References
- Kurtz SM, Ong KL, Lau E, et al. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014 Apr 16;96(8):624–630.
- Gandhi R, Tsvetkov D, Davey JR, et al. Survival and clinical function of cemented and uncemented prostheses in total knee replacement: a meta-analysis. J Bone Joint Surg Br. 2009 Jul;91(7):889–895.
- Asokan A, Plastow R, Kayani B, et al. Cementless knee arthroplasty: a review of recent performance. Bone Jt Open. 2021 Jan;2(1):48–57.
- Wilczyński M, Bieniek M, Krakowski P, et al. Cemented vs. Cementless Fixation in Primary Knee Replacement: A Narrative Review. Materials. 2024;17(5):1136.
- Schwabe MT, Hannon CP. The Evolution, Current Indications and Outcomes of Cementless Total Knee Arthroplasty. J Clin Med. 2022 Nov 8;11(22).
- Gioe TJ, Novak C, Sinner P, et al. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res. 2007 Nov;464:83–87.
- Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009 Oct;467(10):2606–2612.
- Broberg JS, Koff MF, Howard JL, et al. A multimodal assessment of cementless tibial baseplate fixation using radiography, radiostereometric analysis, and magnetic resonance imaging. J Orthop Res. 2024 Jan;42(1):100–108.
- Sheridan GA, Garbuz DS, Nazaroff H, et al. Short-term results of the uncemented triathlon total knee arthroplasty: a large cohort single-centre comparative study. Eur J Orthop Surg Traumatol. 2023 Aug;33(6):2325–2330.
- Winther NS, Jensen CL, Jensen CM, et al. Comparison of a novel porous titanium construct (Regenerex®) to a well proven porous coated tibial surface in cementless total knee arthroplasty - A prospective randomized RSA study with two-year follow-up. Knee. 2016 Dec;23(6):1002–1011.
- Sporer S, MacLean L, Burger A, et al. Evaluation of a 3D-printed total knee arthroplasty using radiostereometric analysis: assessment of highly porous biological fixation of the tibial baseplate and metal-backed patellar component. Bone Joint J. 2019 Jul;101–b(7_Supple_C):40-47.
- van der Lelij TJN, Marang-van de Mheen PJ, Kaptein BL, et al. Continued Stabilization of a Cementless 3D-Printed Total Knee Arthroplasty: Five-Year Results of a Randomized Controlled Trial Using Radiostereometric Analysis. J Bone Joint Surg Am. 2023 Nov 1;105(21):1686–1694.
- Aspinall GR, Dunbar MJ. CHAPTER 4 - Assessing Clinical Results and Outcome Measures. In: Hozack WJ, Parvizi J, Bender B, ed. Surgical Treatment of Hip Arthritis. Philadelphia: W.B. Saunders; 2009. 30–36.
- Ryd L, Albrektsson BE, Carlsson L, et al. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg Br. 1995 May;77(3):377–383.
- Yilmaz M, Holm CE, Lind T, et al. Bone remodeling and implant migration of uncemented femoral and cemented asymmetrical tibial components in total knee arthroplasty - DXA and RSA evaluation with 2-year follow up. Knee Surg Relat Res. 2021 Aug 17;33(1):25.
- Ryd L. Micromotion in knee arthroplasty. A roentgen stereophotogrammetric analysis of tibial component fixation. Acta Orthop Scand Suppl. 1986;220:1–80.
- Andersen MR, Winther N, Lind T, et al. Tibial Component Undersizing Is Related to High Degrees of Implant Migration Following Cementless Total Knee Arthroplasty: A Study of Radiostereometric Analysis Data for 111 Patients with 2-Year Follow-up. JB JS Open Access. 2023 Jul-Sep;8(3).
- Pijls BG, Plevier JWM, Nelissen R. RSA migration of total knee replacements. Acta Orthop. 2018 Jun;89(3):320–328.
- Hasan S, van Hamersveld KT, Marang-van de Mheen PJ, et al. Migration of a novel 3D-printed cementless versus a cemented total knee arthroplasty: two-year results of a randomized controlled trial using radiostereometric analysis. Bone Joint J. 2020 Aug;102-b(8):1016–1024.
- Goh GS, Wells Z, Ong CB, et al. Does Body Mass Index Influence the Outcomes and Survivorship of Modern Cementless Total Knee Arthroplasty? J Arthroplasty. 2022 Nov;37(11):2171–2177.
- Nilsson KG, Kärrholm J, Carlsson L, Dalén T. Hydroxyapatite coating versus cemented fixation of the tibial component in total knee arthroplasty: Prospective randomized comparison of hydroxyapatite-coated and cemented tibial components with 5-year follow-up using radiostereometry. The Journal of Arthroplasty. 1999 1999/01/01/;14(1):9–20.
- van Hamersveld KT, Marang-van de Mheen PJ, Tsonaka R, et al. Fixation and clinical outcome of uncemented peri-apatite-coated versus cemented total knee arthroplasty : five-year follow-up of a randomised controlled trial using radiostereometric analysis (RSA). Bone Joint J. 2017 Nov;99-b(11):1467–1476.
- Molt M, Ryd L, Toksvig-Larsen S. A randomized RSA study concentrating especially on continuous migration. Acta Orthop. 2016 Jun;87(3):262–267.
- Andersen MR, Winther NS, Lind T, et al. Low Preoperative BMD Is Related to High Migration of Tibia Components in Uncemented TKA-92 Patients in a Combined DEXA and RSA Study With 2-Year Follow-Up. J Arthroplasty. 2017 Jul;32(7):2141–2146.