Mid-term outcomes of modern cementless total knee arthroplasty and patient selection in 2024
Preview
Cementless total knee arthroplasty (TKA) has undergone a rapid evolution over the last few years. Technology has advanced leading to new designs with highly porous surfaces promoting osseointegration at the bone-implant interface. These new generations of cementless TKA designs are now starting to show good short- to mid-term outcomes [1].
In this part of the series, Bassam Masri from the Department of Orthopaedics at the University of British Columbia leads us through the technological advancements in cementless TKA designs and their performance in clinical studies, looking at mid-term survivorship and clinical outcomes of newer cementless TKA designs.

Bassam Masri
Department of Orthopaedics, University of British Columbia, Vancouver, Canada
Chairperson AO Recon Education Forum and Member AO Recon Steering Board
Updates in cementless total knee arthroplasties
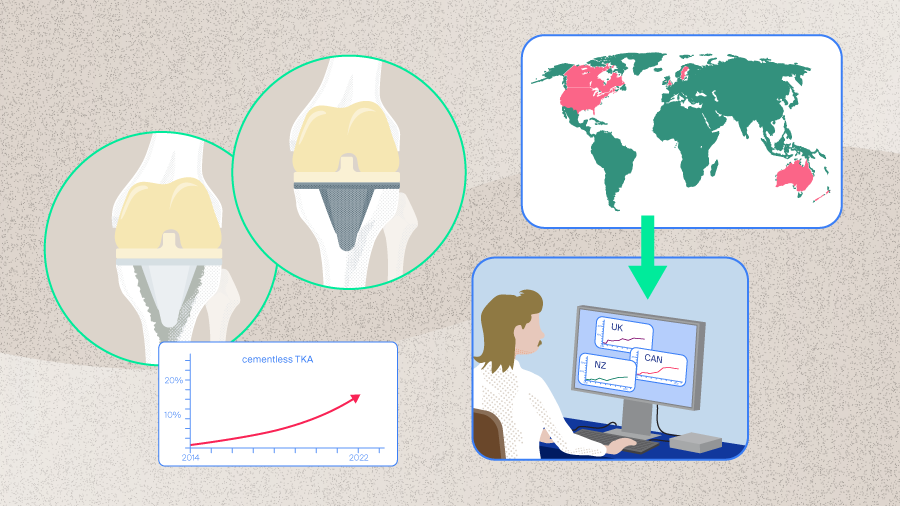
There has been an upsurge in the use of cementless fixation in TKA in recent years evidenced both by the most recent registry data [2–6] and the changing sentiments of an ever-increasing community of surgeons performing TKAs. Indeed, as shown in Part 1 of this series of articles, around one-fifth of TKAs performed in the United States are now cementless, which is a substantial increase compared to 10 years prior [2]. As Masri explains, “at least at our center, the utilization of cementless TKA has increased significantly since 2018, and this has mirrored what other centers and surgeons have done. This is due to the improving results of cementless TKA and will hopefully withstand the test of time.”
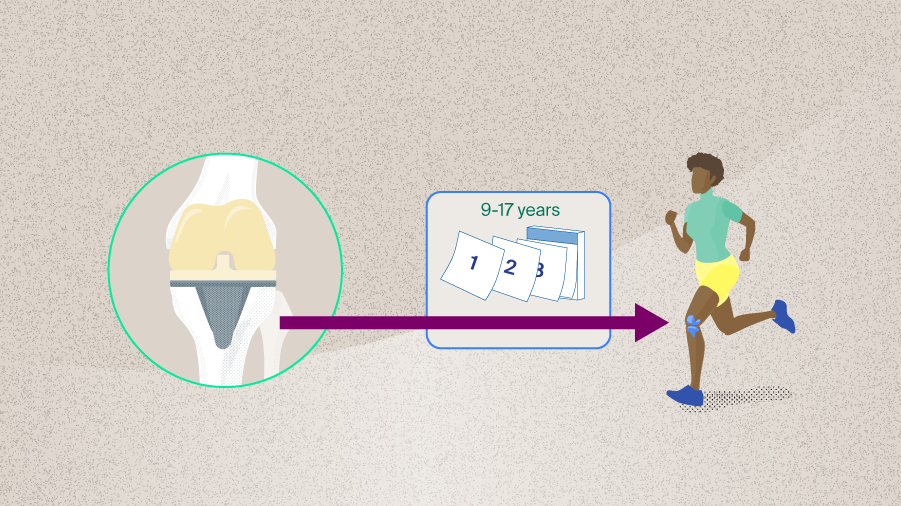
With this increasing trend towards using cementless TKAs comes another, more concerning trend, that of the changing demographic now seeking TKA. Patients are more active, younger, and there are also more obese patients requiring TKA [7]. Bearing these factors in mind, it is now necessary to carefully consider the survival of implants as well as the type of fixation used. Cemented fixation, which is traditionally considered to be the gold standard in TKA, allows for immediate stability of the prosthesis and is still the most frequently used method of fixation. In contrast, cementless fixation was previously associated with poorer outcomes and survivorship when compared with cemented implants. The historically poorer performance of cementless TKAs may potentially be attributed to the type of implant designs used at the time [8]. Thankfully, cementless fixation technology and cementless implant design have advanced. Modern implants now include the addition of highly porous surfaces promoting osseointegration, and this has been coupled with parallel advancements in implant fixation strategies [9]. It was previously proposed that a cementless TKA has the potential to preserve bone stock, avoid cement debris, and provide a lasting biological fixation of the implant to the bone through osseointegration [9]. Regarding the latter, it is therefore more unlikely that implant loosening occurs except as a result of lysis or sepsis [9]. This feeds into the desire to provide an implant with a lasting physiological bone fixation, particularly in the younger and more active as well as the obese population.
Advanced implant technology promotes osseointegration
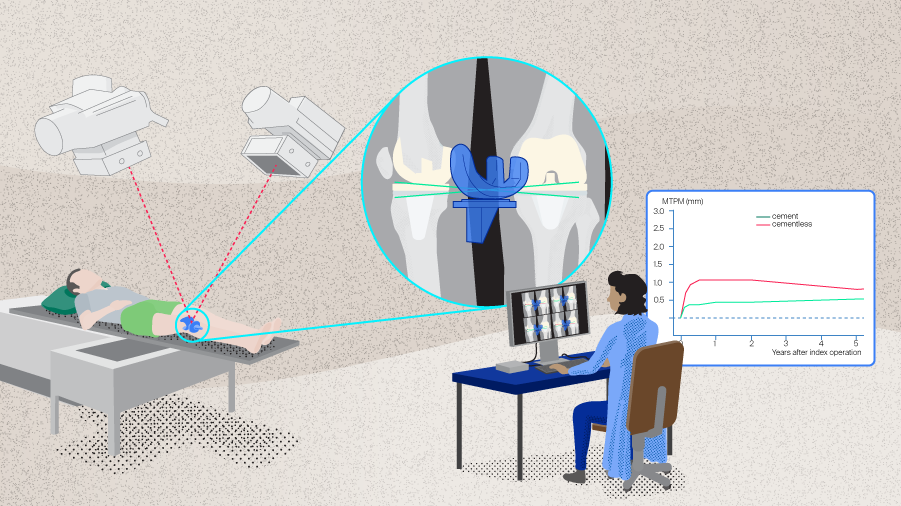
Newer cementless TKA implants have been developed with highly porous surfaces aiming to promote osseointegration to achieve fixation. Here, the osteoblast and mesenchymal cells migrate towards the implant and osseointegration occurs at the implant’s roughened surface achieving durable fixation [10]. The porous surfaces ideally have a minimum pore size of 100 µm taking cell size, migration, and transport into consideration, although pore sizes > 300 µm have been recommended given the new bone and capillary formation that occurs [10]. Additional to the roughened, porous surfaces facilitating osseointegration, these newer surfaces also positively impact primary stability because in the immediate postoperative period, the shear load-bearing capacity at the bone-implant interface is increased [10]. The mechanical “interlock” provided by the porous surface also acts to limit micromotion, an important feature given that the presence of micromotion compromises a change of osseointegration [9].
Read the full article with your AO login
- Updates in cementless TKA fixation
- Advanced implant technology promotes osseointegration
- Overcoming tibial baseplate loosening
- Promising short-term results
- Excellent mid-term survivorship
- Mid-term clinical outcomes achieved
- Patient selection
AO Recon resources
Contributing experts
David F Dalury
University of Maryland St Joseph Medical Center, Baltimore, Maryland, USA
Member AO Recon Education Forum

Bassam Masri
Department of Orthopaedics, University of British Columbia, Vancouver, Canada
Chairperson AO Recon Education Forum and Member AO Recon Steering Board

Gerard A Sheridan
Department of Orthopaedic Surgery, University of Galway, Galway, Ireland
This article was written by Lyndsey Kostadinov, AO Innovation Translation Center, Clinical Science, Switzerland.
References
- Sheridan GA, Garbuz DS, Nazaroff H, et al. Short-term results of the uncemented triathlon total knee arthroplasty: a large cohort single-centre comparative study. Eur J Orthop Surg Traumatol. 2023;33(6):2325–2330.
- American Joint Replacement Registry (AJRR): 2023 Annual Report. Rosemont, IL: American Academy of Orthopaedic Surgeons (AAOS); 2023.
- National Joint Registry | 20th Annual Report. London: National Joint Registry; 2023.
- The New Zealand Joint Registry Twenty-four Year Report (January 1999 - December 2022). New Zealand Orthopaedic Association; 2023.
- Smith PN, Gill DR, McAuliffe MJ, et al. Hip, Knee and Shoulder Arthroplasty: 2023 Annual Report, Australian
Orthopaedic Association National Joint Replacement Registry. 2023. - W-Dahl A, Kärrholm J, Rogmark C, et al. Swedish Arthroplasty Register (2022): Annual report 2022. Swedish Arthroplasty Register; 2022.
- Gold PA, Garbarino L, Sodhi N, et al. The Case for Cementless Total Knee Arthroplasty. Surg Technol Int. 2020;36:388–396.
- Nam D, Kopinski JE, Meyer Z, et al. Perioperative and Early Postoperative Comparison of a Modern Cemented and Cementless Total Knee Arthroplasty of the Same Design. J Arthroplasty. 2017;32(7):2151–2155.
- Dalury DF. Cementless total knee arthroplasty: current concepts review. Bone Joint J. 2016;98-b(7):867–873.
- Polizzotti G, Lamberti A, Mancino F, et al. New Horizons of Cementless Total Knee Arthroplasty. J Clin Med. 2023;13(1).
- Waddell DD, Sedacki K, Yang Y, et al. Early radiographic and functional outcomes of a cancellous titanium-coated tibial component for total knee arthroplasty. MUSCULOSKELETAL SURGERY. 2016;100(1):71–74.
- Bhimji S, Meneghini RM. Micromotion of cementless tibial baseplates: keels with adjuvant pegs offer more stability than pegs alone. J Arthroplasty. 2014;29(7):1503–1506.
- Yazdi H, Choo KJ, Restrepo C, et al. Short-term results of triathlon cementless versus cemented primary total knee arthroplasty. Knee. 2020;27(4):1248–1255.
- Restrepo S, Smith EB, Hozack WJ. Excellent mid-term follow-up for a new 3D-printed cementless total knee arthroplasty. Bone Joint J. 2021;103-b(6 Supple A):32–37.
- Nam D, Bhowmik-Stoker M, Mahoney OM, et al. Mid-Term Performance of the First Mass-Produced Three-Dimensional Printed Cementless Tibia in the United States as Reported in the American Joint Replacement Registry. J Arthroplasty. 2023;38(1):85–89.
- Hegarty P, Walls A, O'Brien S, et al. A Prospective Randomized Study Comparing Postoperative Pain, Biological Fixation, and Clinical Outcomes Between Two Uncemented Rotating Platform Tibial Tray Designs. J Arthroplasty. 2020;35(2):429–437.
- Chen K, Xu J, Dai H, et al. Uncemented Tibial Fixation Has Comparable Prognostic Outcomes and Safety Versus Cemented Fixation in Cruciate-Retaining Total Knee Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. J Clin Med. 2023;12(5).
- Sheridan GA, Cassidy RS, McKee C, et al. Survivorship of 500 Cementless Total Knee Arthroplasties in Patients Under 55 Years of Age. J Arthroplasty. 2023;38(5):820–823.
- Salem HS, Tarazi JM, Ehiorobo JO, et al. Cementless Fixation for Total Knee Arthroplasty in Various Patient Populations: A Literature Review. J Knee Surg. 2020;33(9):848–855.
- Kim YH, Park JW, Lim HM, et al. Cementless and cemented total knee arthroplasty in patients younger than fifty five years. Which is better? Int Orthop. 2014;38(2):297–303.
- Goh GS, Wells Z, Ong CB, et al. Does Body Mass Index Influence the Outcomes and Survivorship of Modern Cementless Total Knee Arthroplasty? J Arthroplasty. 2022;37(11):2171–2177.