Indications for the use of metaphyseal fixation in revision total knee replacement
Preview
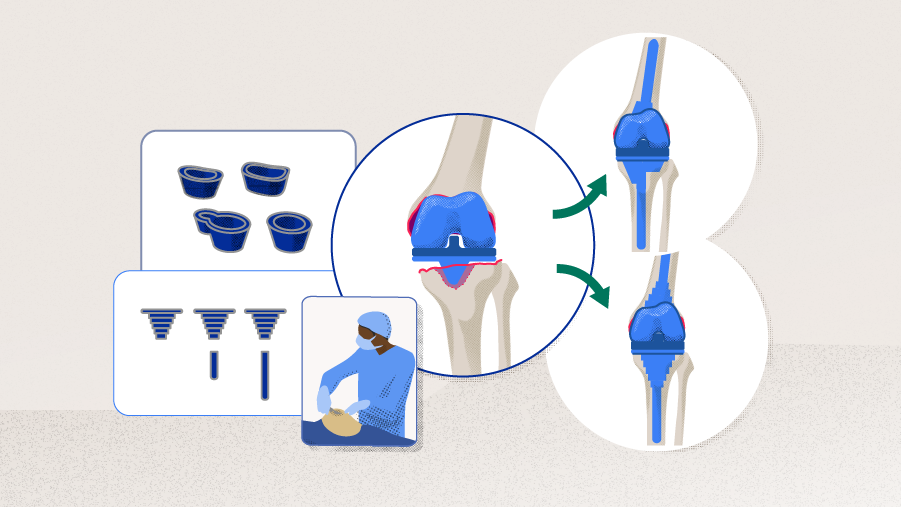
In total knee arthroplasty (TKA) revision surgery, surgeons are often faced with periprosthetic bone loss. Bone loss may even be the ultimate reason for the revision, eg, in patients with aseptic loosening. Additionally, removing a prosthetic component may create further defects. The quantity and quality of bone ultimately drives the decision which type of anchorage to choose for the revision prosthesis. Part 1 of the newsletter will explain the different types of bone defects and the treatment modalities available to address them, with a special focus on metaphyseal anchorage.
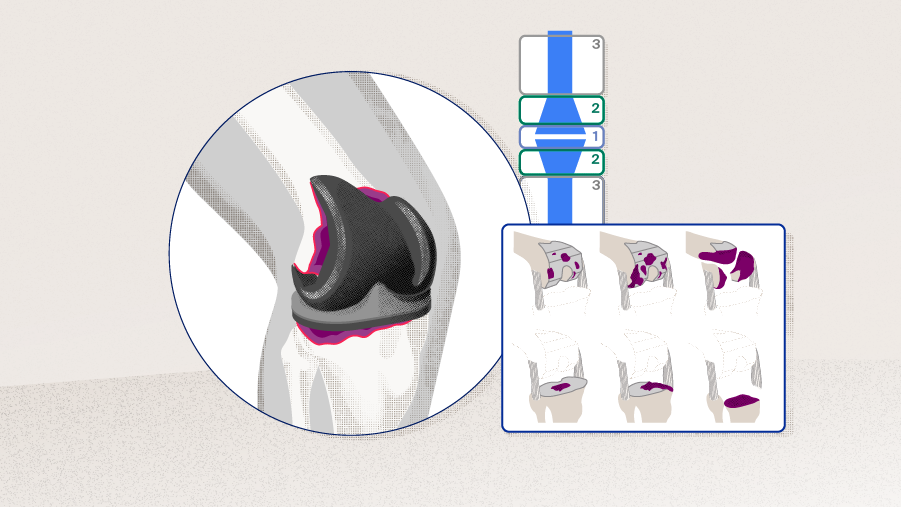
Bone defect classification
Bone defects are an important challenge faced by surgeons when revising a TKA, because they make it difficult to securely anchor an implant. The level of difficulty depends on the severity and location of the defect. Various techniques have been devised to overcome the problem. A wide range of classifications have been developed to classify bone defects based on size, severity, and location of the defects. Some of them may be used for preoperative planning and to guide treatment.
Glen Purnomo
St. Vincentius a Paulo Catholic Hospital
Surabaya, Indonesia
Glen Purnomo, Orthopaedic and Traumatology Specialist at St. Vincentius a Paulo Catholic Hospital, Surabaya, Indonesia, points out: “There is no perfect classification system that would allow to accurately evaluate bone loss for preoperative planning, provide guidelines for management, have proven intra- and interobserver reliability, and predict outcome. Take the Anderson Orthopaedic Research Institute (AORI) classification, which is currently the most widely used: it does not unequivocally prescribe the method to measure defect sizes, so the evaluation remains somewhat subjective. It also misses to include the patella in the evaluation. While some other classifications clearly define the size of the defect, in practice, the radioopaqueness of the implants pose great difficulties to determine the true size of the defect.”
Table 1 provides an overview about the most important classification systems with regard to the type of assessment, ie, preoperative or intraoperative, the features taken into account, ie, dimensions, morphology, and implant stability, as well as the possibility to act as guide for treatment [1].
The different classification systems all use similar assessment criteria. For instance, the minimal type in the Rand classification, the small type in the Slooff and Malefijt classification, the type 1 defect in the AORI classification, the uncontained minor type in the Massachusetts General Hospital classification, the type 1 in the Clatworthey and Gross classification, the cystic type in the Huff and Sculco classification, and the cavitary type in the Bargar and Gross classification—all describe a defect that is small and contained, not requiring complex reconstruction. The massive type in the Rand classification, the discontinuity type in the Bargar and Gross classification, the type 3 defect in the AORI classification, the peripheral type in the Dorr classification, the segmental type in the Huff and Sculco classification, the ice-cream type in the Insall classification—all describe severe defects that reach into the condyles and may even affect the integrity of collateral ligaments [2].
Read the full article with your AO login
- AORI classification
- Different defect types require different treatment modalities
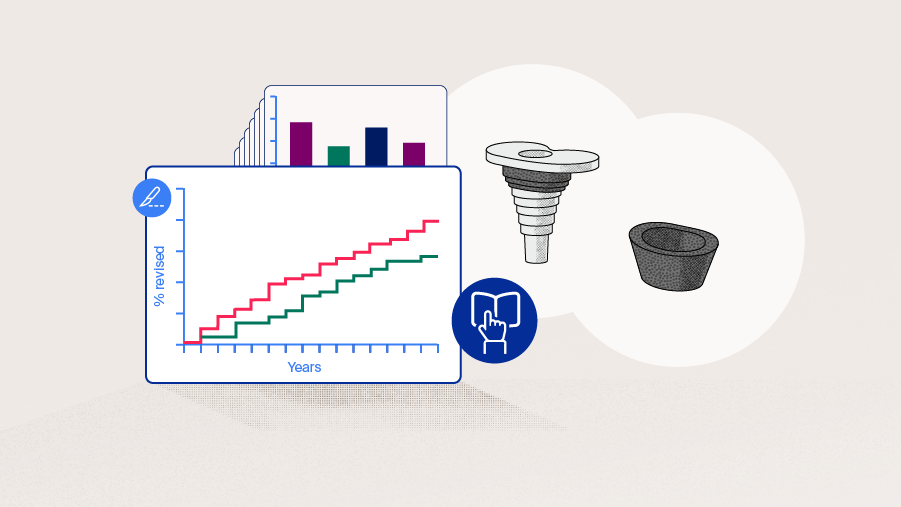
- Treatment modalities for metaphyseal fixation
- Structural bone allograft
- Metal implants: sleeves and cones
Additional AO resources
Access videos, tools, and other assets to learn more about this topic.
- Video: Metaphyseal Fixation in Revision Total Knee Arthroplasty
- Video: Tips and Tricks to Improve Total Knee Arthroplasty Outcomes
- Video: The Difficult Primary Total Knee Arthroplasty
- AO Surgery Reference
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Omar Behery
Atrium Health Musculoskeletal Institute
Charlotte, United States
David F Dalury
University of Maryland St Joseph Hospital
Towson, United States
Glen Purnomo
St. Vincentius a Paulo Catholic Hospital
Surabaya, Indonesia

Bryan D Springer
Atrium Health Musculoskeletal Institute
Charlotte, United States
Seng-Jin Yeo
Singapore General Hospital
Singapore
This article was compiled by Elke Rometsch, Project Manager Medical Writing, AO Foundation, Switzerland.
References
- Mancuso F, Beltrame A, Colombo E, et al. Management of metaphyseal bone loss in revision knee arthroplasty. Acta Biomed. 2017 Jun 7;88(2s):98–111.
- Qiu YY, Yan CH, Chiu KY, et al. Review article: bone defect classifications in revision total knee arthroplasty. J Orthop Surg (Hong Kong). 2011 Aug;19(2):238–243.
- Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–175.
- Sculco PK, Abdel MP. Contemporary bone loss options: Rebuild, reinforce, and augment. Seminars in Arthroplasty. 2015;26(2):108–111.
- Panegrossi G, Ceretti M, Papalia M, et al. Bone loss management in total knee revision surgery. Int Orthop. 2014 Feb;38(2):419–427.
- Lee YS, Chen AF. Managing bone loss in revision total knee arthroplasty. Annals of Joint. 2016;1:17–17.
- Morgan-Jones R, Oussedik SI, Graichen H, et al. Zonal fixation in revision total knee arthroplasty. Bone Joint J. 2015 Feb;97-b(2):147–149.
- Lei PF, Hu RY, Hu YH. Bone Defects in Revision Total Knee Arthroplasty and Management. Orthop Surg. 2019 Feb;11(1):15–24.
- Lombardi AV, Berend KR, Adams JB. Management of bone loss in revision TKA: it's a changing world. Orthopedics. 2010 Sep 7;33(9):662.
- Bauman RD, Lewallen DG, Hanssen AD. Limitations of Structural Allograft in Revision Total Knee Arthroplasty. Clinical Orthopaedics and Related Research®. 2009;467(3):818–824.
- Clatworthy MG, Ballance J, Brick GW, et al. The use of structural allograft for uncontained defects in revision total knee arthroplasty. A minimum five-year review. J Bone Joint Surg Am. 2001 Mar;83(3):404–411.
- Backstein D, Safir O, Gross A. Management of Bone Loss: Structural Grafts in Revision Total Knee Arthroplasty. Clinical Orthopaedics and Related Research®. 2006;446:104–112.
- Haidukewych GJ, Hanssen A, Jones RD. Metaphyseal fixation in revision total knee arthroplasty: indications and techniques. J Am Acad Orthop Surg. 2011 Jun;19(6):311–318.
- Alexander GE, Bernasek TL, Crank RL, et al. Cementless metaphyseal sleeves used for large tibial defects in revision total knee arthroplasty. J Arthroplasty. 2013 Apr;28(4):604–607.
- Salim X, Lopez DJ, Jeys L, et al. Cones and sleeves in knee arthroplasty: a narrative review. Current Orthopaedic Practice. 2019 09/01;30:1.
- Roach RP, Clair AJ, Behery OA, et al. Aseptic Loosening of Porous Metaphyseal Sleeves and Tantalum Cones in Revision Total Knee Arthroplasty: A Systematic Review. J Knee Surg. 2020 Feb 19.
- Graichen H, Scior W, Strauch M. Direct, Cementless, Metaphyseal Fixation in Knee Revision Arthroplasty With Sleeves-Short-Term Results. J Arthroplasty. 2015 Dec;30(12):2256–2259.
- Martin-Hernandez C, Floria-Arnal LJ, Muniesa-Herrero MP, et al. Mid-term results for metaphyseal sleeves in revision knee surgery. Knee Surg Sports Traumatol Arthrosc. 2017 Dec;25(12):3779–3785.
- Ihekweazu UN, Weitzler L, Wright TM, et al. Distribution of Bone Ongrowth in Metaphyseal Sleeves for Revision Total Knee Arthroplasty: A Retrieval Analysis. J Arthroplasty. 2019 Apr;34(4):760–765.
- Graichen H, Scior W. Is stemless implant fixation a valid option in total knee revision arthroplasty - Review of in vitro and in vivo studies. J Orthop. 2021 Jan-Feb;23:113–117.
- Bugler KE, Maheshwari R, Ahmed I, et al. Metaphyseal Sleeves for Revision Total Knee Arthroplasty: Good Short-Term Outcomes. J Arthroplasty. 2015 Nov;30(11):1990–1994.
- Agarwal S, Azam A, Morgan-Jones R. Metal metaphyseal sleeves in revision total knee replacement. Bone Joint J. 2013 Dec;95-b(12):1640–1644.
- Thorsell M, Hedström M, Wick MC, et al. Good clinical and radiographic outcome of cementless metal metaphyseal sleeves in total knee arthroplasty. Acta Orthop. 2018 Feb;89(1):84–88.
- Agarwal S, Neogi DS, Morgan-Jones R. Metaphyseal sleeves in revision total knee arthroplasty: Minimum seven-year follow-up study. Knee. 2018 Dec;25(6):1299–1307.
- Fonseca F, Sousa A, Completo A. Femoral revision knee Arthroplasty with Metaphyseal sleeves: the use of a stem is not mandatory of a structural point of view. J Exp Orthop. 2020 Apr 26;7(1):24.
- Scior W, Chanda D, Graichen H. Are Stems Redundant in Times of Metaphyseal Sleeve Fixation? J Arthroplasty. 2019 Oct;34(10):2444–2448.
- Awadalla M, Al-Dirini RMA, O'Rourke D, et al. Influence of varying stem and metaphyseal sleeve size on the primary stability of cementless revision tibial trays used to reconstruct AORI IIA defects. A simulation study. J Orthop Res. 2018 Jul;36(7):1876–1886.
- Nadorf J, Gantz S, Kohl K, et al. Tibial revision knee arthroplasty: influence of modular stems on implant fixation and bone flexibility in AORI Type T2a defects. Int J Artif Organs. 2016 Nov 29;39(10):534–540.
- Nadorf J, Kinkel S, Gantz S, et al. Tibial revision knee arthroplasty with metaphyseal sleeves: The effect of stems on implant fixation and bone flexibility. PLoS One. 2017;12(5):e0177285.
- Kamath AF, Lewallen DG, Hanssen AD. Porous tantalum metaphyseal cones for severe tibial bone loss in revision knee arthroplasty: a five to nine-year follow-up. J Bone Joint Surg Am. 2015 Feb 4;97(3):216–223.
- Long WJ, Scuderi GR. Porous tantalum cones for large metaphyseal tibial defects in revision total knee arthroplasty: a minimum 2-year follow-up. J Arthroplasty. 2009 Oct;24(7):1086–1092.
- Huten D. Femorotibial bone loss during revision total knee arthroplasty. Orthop Traumatol Surg Res. 2013 Feb;99(1 Suppl):S22–33.