Preventing periprosthetic joint infections: how to lower infection rates
Preview
As the number of joint replacements being performed around the world grows every year, so do the number of periprosthetic joint infections (PJI). The troublesome rise in antibiotic resistance as well as the antibiotic tolerance of biofilms, presents risk to patients and limited and shrinking treatment options for clinicians. What measures can you and your surgical team take prior to, during, and after joint replacement that will help lower the risk of PJI?
The frequency of joint replacement is forecast to continue its upward trend in all countries. A study in 2019 by Ackerman et al predicted that Australia could expect total knee (TKR) and hip (THR) replacements to increase by 276% and 208%, respectively, by 2030 [1]. Whether or not joint replacement growth estimates take into account a country’s changing demographics, body mass index (BMI), and gender factors [2], it is agreed that joint arthroplasty will only become more common [3–5]. As the number of implantations and cumulative number of joints in place increases, so too will the number of reported complications, including related infections [6, 7].
Did you miss AO Recon’s webinar on periprosthetic joint infection (PJI)?
In June 2019, AO Recon gathered an online community of close to 200 surgeons for an interactive information session and Q&A led by Olivier Borens, Head of Septic Surgery and Head of Traumatology at the Centre Hospitalier Universitaire Vaudois (Lausanne, Switzerland) and chat moderator Andrej Trampuz, Infectious Diseases Consultant in Septic Surgery at Charité–Universitätsmedizin (Berlin, Germany) on the topic of infection after joint arthroplasty.
Economic burden of infection
Despite the evolution and adoption of more stringent infection control protocols, infection is a very serious problem throughout the world’s hospitals. It carries both a psychological and economic burden for both patients and their families, the health care team, as well as the health care system. With a wider consideration of costs to society, health care-associated infection costs in the US have been estimated to exceed $200 billion annually [8].
Periprosthetic joint infection (PJI) is a complication that is both “serious and complex” [9]. As orthopedic surgeons, you will have had patients that were impacted by PJI, with some cases responding to treatment more readily than others [10]. Treating PJI can increase procedure costs by up to 24 times compared with cases without PJI [12]. The longer treatment takes and the more surgical intervention that is required (such as two-stage revisions), the higher the costs [6, 12, 13].
Antimicrobial resistance
However, the persistence of infection encountered in some patients, despite antibiotic treatment, highlights a global problem that has been brewing since antibiotics came into use. Antimicrobial resistance is developing to the antibiotics and fungicides that even 50 years ago were effective and rapid treatments. Methicillin-resistant Staphylococcus aureus (MRSA) is estimated to cause at least 20,000 annual in-hospital deaths in the US alone [11].
Tackling antimicrobial resistance
There are numerous organizations with the aim of funding, conducting, and/or dispersing research into antimicrobial resistance as well as providing education on its prevention and treatment. Here are a few:
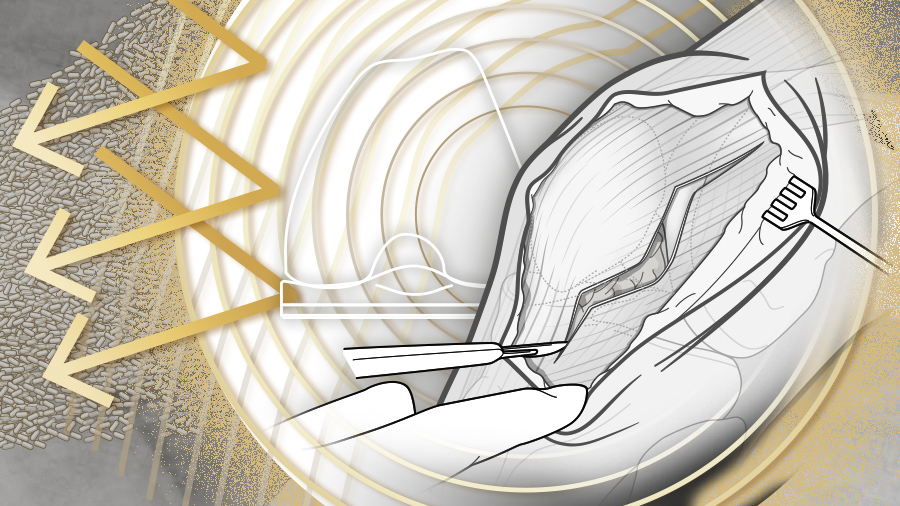
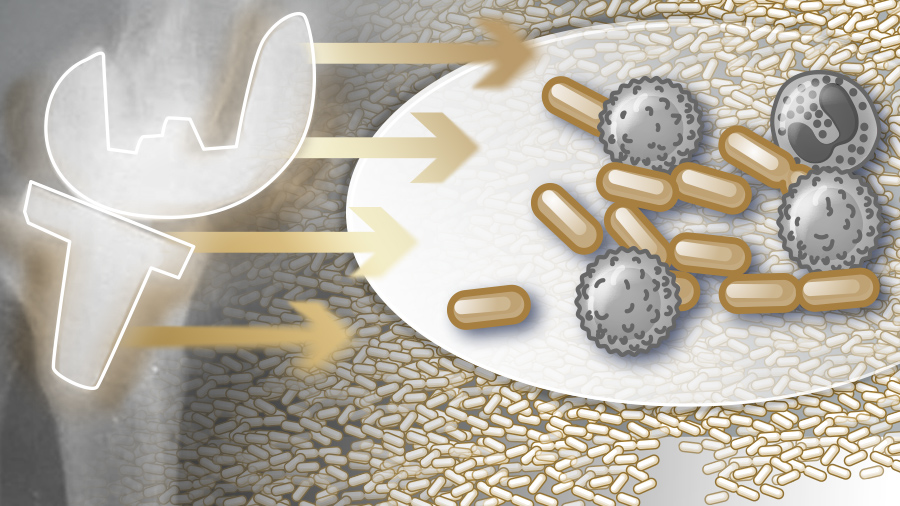
Biofilms: a complex, persistent neighborhood
However, PJI’s are difficult to treat because pathogen microorganisms colonize the prosthesis, growing in biofilms [12]. Biofilms are “structurally complex” which gives them the emergent property of an evolved protection against the body’s immune response as well as against antibiotics, and even physical debridement [13]. A biofilm is more persistent than its parts as it is structured in a layered matrix—a community that alters its metabolic function and even communicates with itself via quorum sensing [14, 15].
How does bacteria form a biofilm?
A short animation from the Centre for Microbial Innovation, at the University of Auckland, New Zealand, illustrates the process. Created by Andrew Dopheide.
How bacteria form a biofilm from Andrew Dopheide on Vimeo.
Ciofu et al point out that biofilm-associated antimicrobial tolerance is “fundamentally different from antimicrobial resistance” and attribute this to the following multi-factorial causes [16]:
- Antimicrobial tolerance increases with biofilm age (maturation)
- Biofilm matrices restrict antimicrobial penetration
- Bacterial metabolic activity varies within the layers of biofilm
- Specific gene expression unique to biofilms can provide enhanced tolerance
- Persister cells divide slowly or not at all, inhibiting antibiotic pathways
- The in vivo environment may have low oxygen tension, limiting the effectiveness of antibiotics dependent on the presence of oxygen for uptake, such as fluoroquinolones, beta‐lactams, and aminoglycosides
It has been observed that biofilm-associated infections are diversifying and the impact of this may be underestimated [17]. The persistent characteristics of biofilm and the role it plays in PJI highlights the importance of correct use of biofilm active antibiotics in implant-associated infections.
Read the full article with your AO login
- PJI rates differ for joints
- Prevention of PJI needs a cross-disciplinary approach
- PREOPERATIVE infection prevention strategies
- Identification and management of risk factor comorbidities
- Nasal screening
- Skin preparation
- Immunosuppressive therapy
- Glycemic control
- New device coatings to battle microorganisms
- INTRAOPERATIVE infection prevention strategies
- Prophylactic antibiotics
- Reducing operating room traffic
- Dressed for success
- A (clean) tool for the job?
- POSTOPERATIVE infection prevention strategies
- Prophylactic antibiotics for certain procedures
- Blood transfusion
- Wound care
- Timeline for prevention
- Conclusion
- References
Additional AO resources on this topic
Access videos, tools, and other assets to learn more about this topic.
- Video: Updates in Infection Management after TKA
- Video: Infection After Joint Arthroplasty
- Further reading: Fracture-related infection: new consensus on diagnosis and treatment
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):
Olivier Borens
University Hospital Lausanne
Lausanne, Switzerland

Nora Renz
Inselspital—University Hospital Bern
Bern, Switzerland

Andrej Trampuz
Charité—University Medicine Berlin
Berlin, Germany
This issue was created by Word+Vision Media Productions, Switzerland.
References
- Ackerman IN, Bohensky MA, Zomer E, et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord. 2019 Feb 23;20(1):90.
- Culliford D, Maskell J, Judge A, et al. Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthritis Cartilage. 2015 Apr;23(4):594–600.
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–785.
- Inacio MCS, Paxton EW, Graves SE, et al. Projected increase in total knee arthroplasty in the United States—an alternative projection model. Osteoarthritis Cartilage. 2017 Nov;25(11):1797–1803.
- Carvalho RT, Lopes TL, Takano MI, et al. Evolution and projection of knee arthroplasties from 2003 to 2030 in the state of Sao Paulo. Rev Assoc Med Bras (1992). 2019 Aug 5;65(7):1001–1006.
- Kurtz SM, Lau E, Watson H, et al. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012 Sep;27(8 Suppl):61–65 e1.
- Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014 Apr;27(2):302–345.
- Scott RD, 2nd, Culler SD, Rask KJ. Understanding the Economic Impact of Health Care-Associated Infections: A Cost Perspective Analysis. J Infus Nurs. 2019 Mar/Apr;42(2):61–69.
- World Health Organization. Antimicrobial resistance: global report on surveillance 2014. 2014, April.
- Teterycz D, Ferry T, Lew D, et al. Outcome of orthopedic implant infections due to different staphylococci. Int J Infect Dis. 2010 Oct;14(10):e913-8.
- Boucher HW, Corey GR. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008 Jun 1;46 Suppl 5:S344–349.
- Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004 Oct 14;351(16):1645–1654.
- Jacqueline C, Caillon J. Impact of bacterial biofilm on the treatment of prosthetic joint infections. J Antimicrob Chemother. 2014 Sep;69 Suppl 1:i37–i40.
- Taha M, Abdelbary H, Ross FP, et al. New Innovations in the Treatment of PJI and Biofilms-Clinical and Preclinical Topics. Curr Rev Musculoskelet Med. 2018 Sep;11(3):380-388.
- Chen L, Wen YM. The role of bacterial biofilm in persistent infections and control strategies. Int J Oral Sci. 2011 Apr;3(2):66–73.
- Ciofu O, Rojo-Molinero E, Macia MD, et al. Antibiotic treatment of biofilm infections. APMIS. 2017 Apr;125(4):304–319.
- Del Pozo JL. Biofilm-related disease. Expert Rev Anti Infect Ther. 2018 Jan;16(1):51–65.
- Illingworth KD, Mihalko WM, Parvizi J, et al. How to minimize infection and thereby maximize patient outcomes in total joint arthroplasty: a multicenter approach: AAOS exhibit selection. J Bone Joint Surg Am. 2013 Apr 17;95(8):e50.
- Aggarwal VK, Weintraub S, Klock J, et al. 2019 Frank Stinchfield Award: A comparison of prosthetic joint infection rates between direct anterior and non-anterior approach total hip arthroplasty. Bone Joint J. 2019 Jun;101-B(6_Supple_B):2–8.
- Achermann Y, Vogt M, Spormann C, et al. Characteristics and outcome of 27 elbow periprosthetic joint infections: results from a 14-year cohort study of 358 elbow prostheses. Clin Microbiol Infect. 2011 Mar;17(3):432–438.
- Egglestone A, Ingoe H, Rees J, et al. Scoping review: Diagnosis and management of periprosthetic joint infection in shoulder arthroplasty. Shoulder Elbow. 2019 Jun;11(3):167-181.
- Li C, Renz N, Trampuz A. Management of Periprosthetic Joint Infection. Hip Pelvis. 2018 Sep;30(3):138–146.
- Kurtz SM, Ong KL, Lau E, et al. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res. 2010 Jan;468(1):52–56.
- Roberts HJ, Tsay EL, Grace TR, et al. Increased conditional risk of recurring complications with contralateral total hip arthroplasty surgery. Bone Joint J. 2019 Jun;101-B(6_Supple_B):77–83.
- Lenguerrand E, Whitehouse MR, Beswick AD, et al. Risk factors associated with revision for prosthetic joint infection following knee replacement: an observational cohort study from England and Wales. Lancet Infect Dis. 2019 Jun;19(6):589–600.
- Bodansky D, Oskrochi Y, Judah G, et al. Change the habit to change the practice: Do audits really ever change anything? Injury. 2017 Sep;48(9):1999–2002.
- Nobile M, Bronzin S, Navone P, et al. Reinforcing good practice: Implementation of guidelines at hospital G. Pini. Injury. 2014 Dec;45 Suppl 6:S2–S8.
- Sartelli M, Kluger Y, Ansaloni L, et al. Knowledge, awareness, and attitude towards infection prevention and management among surgeons: identifying the surgeon champion. World J Emerg Surg. 2018;13:37.
- Conaty O, Gaughan L, Downey C, et al. An interdisciplinary approach to improve surgical antimicrobial prophylaxis. Int J Health Care Qual Assur. 2018 Mar 12;31(2):162–172.
- Mahmoudi L, Ghouchani M, Mahi-Birjand M, et al. Optimizing compliance with surgical antimicrobial prophylaxis guidelines in patients undergoing gastrointestinal surgery at a referral teaching hospital in southern Iran: clinical and economic impact. Infect Drug Resist. 2019;12:2437–2444.
- Morris AJ, Roberts SA, Grae N, et al. The New Zealand Surgical Site Infection Improvement (SSII) Programme: a national quality improvement programme reducing orthopaedic surgical site infections. N Z Med J. 2018 Jul 27;131(1479):45–56.
- Rakow A, Perka C, Trampuz A, et al. Origin and characteristics of haematogenous periprosthetic joint infection. Clin Microbiol Infect. 2019 Jul;25(7):845–850.
- Accardi R, Castaldi S, Marzullo A, et al. Prevention of healthcare associated infections: a descriptive study. Ann Ig. 2017 Mar-Apr;29(2):101–115.
- Forrester JA, Koritsanszky L, Parsons BD, et al. Development of a Surgical Infection Surveillance Program at a Tertiary Hospital in Ethiopia: Lessons Learned from Two Surveillance Strategies. Surg Infect (Larchmt). 2018 Jan;19(1):25–32.
- Chandrananth J, Rabinovich A, Karahalios A, et al. Impact of adherence to local antibiotic prophylaxis guidelines on infection outcome after total hip or knee arthroplasty. J Hosp Infect. 2016 Aug;93(4):423–427.
- Handaya AY, Werdana VAP. Adherence to preoperative hand hygiene and sterile gowning technique among consultant surgeons, surgical residents, and nurses: a pilot study at an academic medical center in Indonesia. Patient Saf Surg. 2019;13:11.
- Badia JM, Casey AL, Rubio-Perez I, et al. A survey to identify the breach between evidence and practice in the prevention of surgical infection: Time to take action. Int J Surg. 2018 Jun;54(Pt A):290–297.
- Allegranzi B, Bischoff P, de Jonge S, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016 Dec;16(12):e276-e287.
- Allegranzi B, Zayed B, Bischoff P, et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016 Dec;16(12):e288–e303.
- Barchitta M, Matranga D, Quattrocchi A, et al. Prevalence of surgical site infections before and after the implementation of a multimodal infection control programme. J Antimicrob Chemother. 2012 Mar;67(3):749–755.
- McHugh SM, Corrigan MA, Dimitrov BD, et al. Preventing infection in general surgery: improvements through education of surgeons by surgeons. J Hosp Infect. 2011 Aug;78(4):312–316.
- Ratto N, Arrigoni C, Rosso F, et al. Total knee arthroplasty and infection: how surgeons can reduce the risks. EFORT Open Rev. 2016 Sep;1(9):339-344.
- Lowik CAM, Zijlstra WP, Knobben BAS, et al. Obese patients have higher rates of polymicrobial and Gram-negative early periprosthetic joint infections of the hip than non-obese patients. PLoS One. 2019;14(4):e0215035.
- Ratto N, Arrigoni C, Rosso F, et al. Total knee arthroplasty and infection: how surgeons can reduce the risks. EFORT Open Rev. 2016 Sep;1(9):339–344.
- Cancienne JM, Werner BC, Browne JA. Is There a Threshold Value of Hemoglobin A1c That Predicts Risk of Infection Following Primary Total Hip Arthroplasty? J Arthroplasty. 2017 Sep;32(9S):S236–S240.
- Breznicky J, Hlavac M, Novak M, et al. Risk factors for periprosthetic joint infection of the hip and knee. Med Glas (Zenica). 2020 Feb 1;17(1).
- Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J. 2013 Nov;95-B(11):1450–1452.
- Parvizi J, Shohat N, Gehrke T. Prevention of periprosthetic joint infection: new guidelines. Bone Joint J. 2017 Apr;99-B(4 Supple B):3–10.
- Gorwitz RJ, Kruszon-Moran D, McAllister SK, et al. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001-2004. J Infect Dis. 2008 May 1;197(9):1226–1234.
- Courville XF, Tomek IM, Kirkland KB, et al. Cost-effectiveness of preoperative nasal mupirocin treatment in preventing surgical site infection in patients undergoing total hip and knee arthroplasty: a cost-effectiveness analysis. Infect Control Hosp Epidemiol. 2012 Feb;33(2):152–159.
- Pelfort X, Romero A, Brugues M, et al. Reduction of periprosthetic Staphylococcus aureus infection by preoperative screening and decolonization of nasal carriers undergoing total knee arthroplasty. Acta Orthop Traumatol Turc. 2019 Sep 16.
- Swan JT, Ashton CM, Bui LN, et al. Effect of Chlorhexidine Bathing Every Other Day on Prevention of Hospital-Acquired Infections in the Surgical ICU: A Single-Center, Randomized Controlled Trial. Crit Care Med. 2016 Oct;44(10):1822–1832.
- Emara K, Hirose CB, Rogero R. What Preoperative Optimization Should Be Implemented to Reduce the Risk of Surgical Site Infection/Periprosthetic Joint Infection (SSI/PJI) in Patients Undergoing Total Ankle Arthroplasty (TAA)? Foot Ankle Int. 2019 Jul;40(1_suppl):6S–8S.
- Kapadia BH, Zhou PL, Jauregui JJ, et al. Does Preadmission Cutaneous Chlorhexidine Preparation Reduce Surgical Site Infections After Total Knee Arthroplasty? Clin Orthop Relat Res. 2016 Jul;474(7):1592–1598.
- Shohat N, Muhsen K, Gilat R, et al. Inadequate Glycemic Control Is Associated With Increased Surgical Site Infection in Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. J Arthroplasty. 2018 Jul;33(7):2312–2321 e3.
- Darouiche RO. Treatment of infections associated with surgical implants. N Engl J Med. 2004 Apr 1;350(14):1422–1429.
- Wang M, Tang T. Surface treatment strategies to combat implant-related infection from the beginning. J Orthop Translat. 2019 Apr;17:42-54.
- Elbourne A, Crawford RJ, Ivanova EP. Nano-structured antimicrobial surfaces: From nature to synthetic analogues. J Colloid Interface Sci. 2017 Dec 15;508:603–616.
- Wyles CC, Hevesi M, Osmon DR, et al. 2019 John Charnley Award: Increased risk of prosthetic joint infection following primary total knee and hip arthroplasty with the use of alternative antibiotics to cefazolin: the value of allergy testing for antibiotic prophylaxis. Bone Joint J. 2019 Jun;101-B(6_Supple_B):9–15.
- Branch-Elliman W, O'Brien W, Strymish J, et al. Association of Duration and Type of Surgical Prophylaxis With Antimicrobial-Associated Adverse Events. JAMA Surg. 2019 Jul 1;154(7):590–598.
- Quintanilla M. [Impact of adherence to local antibiotic prophylaxis guidelines on infection outcome after total hip or knee arthroplasty.]. Rev Chilena Infectol. 2016 Dec;33(6):706.
- Panahi P, Stroh M, Casper DS, et al. Operating room traffic is a major concern during total joint arthroplasty. Clin Orthop Relat Res. 2012 Oct;470(10):2690–2694.
- Song Z, Borgwardt L, Hoiby N, et al. Prosthesis infections after orthopedic joint replacement: the possible role of bacterial biofilms. Orthop Rev (Pavia). 2013 Jun 7;5(2):65–71.
- Qoreishi M, Abbasian M, Safdari F. Sterile Parts of Operating Gown during Lower Limb Joint Replacement Surgery. Arch Bone Jt Surg. 2019 Jul;7(4):354–359.
- Byrd WA, Kavolus JJ, Penrose CT, et al. Donning Gloves Before Surgical Gown Eliminates Sleeve Contamination. J Arthroplasty. 2019 Jun;34(6):1184–1188.
- Lopes LKO, Costa DM, Tipple AFV, et al. Complex design of surgical instruments as barrier for cleaning effectiveness, favouring biofilm formation. J Hosp Infect. 2019 Sep;103(1):e53–e60.
- Deshpande A, Smith GW, Smith AJ. Biofouling of surgical power tools during routine use. J Hosp Infect. 2015 Jul;90(3):179–185.
- HAI and Antibiotic Use Prevalence Survey.: Centers for Disease Control and Prevention.; 2014 [cited 2019. September 17.]. Available from: https://www.cdc.gov/hai/eip/antibiotic-use.html
- Grosso MJ, Neuwirth AL, Boddapati V, et al. Decreasing Length of Hospital Stay and Postoperative Complications After Primary Total Hip Arthroplasty: A Decade Analysis From 2006 to 2016. J Arthroplasty. 2019 Mar;34(3):422–425.
- Chen A, Haddad F, Lachiewicz P, et al. Prevention of late PJI. J Arthroplasty. 2014 Feb;29(2 Suppl):119–128.
- DeFroda SF, Lamin E, Gil JA, et al. Antibiotic Prophylaxis for Patients with a History of Total Joint Replacement. J Am Board Fam Med. 2016 Jul-Aug;29(4):500–507.
- Kim JL, Park JH, Han SB, et al. Allogeneic Blood Transfusion Is a Significant Risk Factor for Surgical-Site Infection Following Total Hip and Knee Arthroplasty: A Meta-Analysis. J Arthroplasty. 2017 Jan;32(1):320–325.
- Pulido L, Ghanem E, Joshi A, et al. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008 Jul;466(7):1710–1715.
- Matar WY, Jafari SM, Restrepo C, et al. Preventing infection in total joint arthroplasty. J Bone Joint Surg Am. 2010 Dec;92 Suppl 2:36–46.
- Gibon E, Courpied JP, Hamadouche M. Total joint replacement and blood loss: what is the best equation? Int Orthop. 2013 Apr;37(4):735–739.
- Cai J, Karam JA, Parvizi J, et al. Aquacel surgical dressing reduces the rate of acute PJI following total joint arthroplasty: a case-control study. J Arthroplasty. 2014 Jun;29(6):1098–1100.
- Kuo FC, Chen B, Lee MS, et al. AQUACEL(R) Ag Surgical Dressing Reduces Surgical Site Infection and Improves Patient Satisfaction in Minimally Invasive Total Knee Arthroplasty: A Prospective, Randomized, Controlled Study. Biomed Res Int. 2017;2017:1262108.