Positioning of the acetabular component: Key elements
Preview
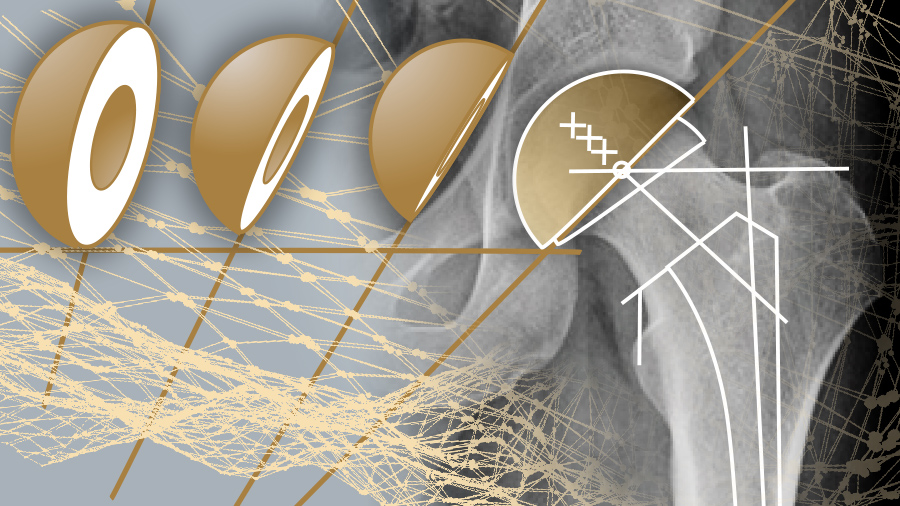
Total hip arthroplasty (THA) aims to return joint function and improve joint stability for patients. If surgeons do not account for the unique biomechanics of each patient, outcomes can be negatively impacted—leg length discrepancy, gait dysfunction, impingement, wear, and loosening are all issues that may arise. Accurate positioning of the acetabular cup is one element of a THA that can alleviate many of these concerns. There are five aspects of cup positioning that influence the success of THA: medialization, depth, height, angular positioning, and pelvic tilt. How do these considerations allow surgeons to accommodate patient-specific characteristics?
It will be of no surprise to AO Recon members to read, that medicine is moving away from a generalized, one-size-fits-all approach towards treatment strategies that take into account an individuals’ unique physiology and/or genetic composition, among other considerations [1, 2]. While customized care based on the unique needs of each patient has been forefront for quite some time, as our understanding of genetics and acknowledgement of physiological differences grows, so too do our treatment options.
Indeed, precision or personalized medicine, the tailoring of health care based on genetics, lifestyle, and environment, is gaining traction around the world—in 2015, US President Obama announced the launch of the National Health Institute’s Precision Medicine Initiative. The Initiative has the stated mission of enabling “a new era of medicine through research, technology, and policies that empower patients, researchers, and providers to work together toward development of individualized care.” [3]
Personalized orthopedics
In OECD countries, THA is expected to grow at a rate of 1.2% per year, with approximately 2.8 million annual hip replacements in 2050 [4]; another study on THA trends in the US predicts that by 2060, there will be 1.23 million primary THA’s a year in that country alone [5].
Orthopedic surgeons are seeing the introduction of technology such as 3D printing of device components and instrumentation that facilitate treatment customized to specific patients [6, 7]. While new technology and understanding certainly play a role in improved outcomes, successful THA is increasingly being seen as more reliant on achieving biomechanics optimized for each individual patient and less on achieving generic intraoperative targets.
Goals of THA
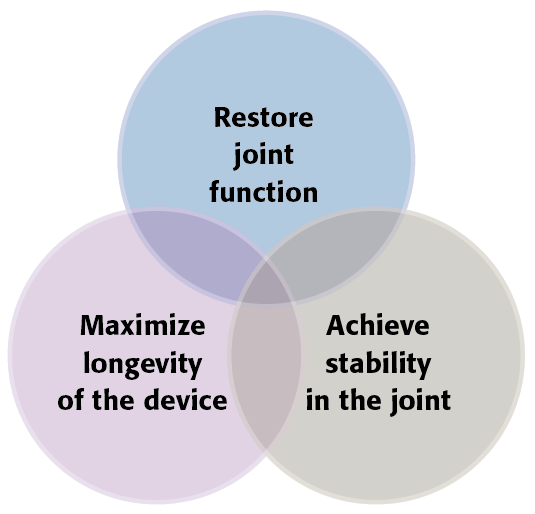
For a THA to be considered successful from a surgeon’s perspective, three interdependent elements must be satisfied. Firstly, functionality of the hip joint must be delivered so mobility can be returned to a patient. Secondly, stability within the joint is integral to meeting the goal of mobility and this must be achieved surgically. Thirdly, maximizing the lifespan of the implant is associated with realization of the previous two elements (see Figure 1). Revision THA for any reason brings increased risks to patients such as infection and re-do revisions [8]. Malpositioning of the acetabular cup has been called “the most common cause of THA dislocation” [9].
Read the full article with your AO login
- What we want to avoid: dislocation, pain, revision
- Defining acetabular cup positioning
- Joint reaction force
- Medialization
- Conventional versus anatomic approach
- Depth
- Height
- Angular positioning: anteversion and inclination
- Variability in defining “safe zone” angles
- Different ways to measure and describe the “safe zone”
- Pelvic tilt
- Conclusion
- References
Additional AO resources
Access videos, tools, and other assets to learn more about this topic.
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Mohamad Allami
Burjeel Hospital
Abu Dhabi, United Arab Emirates

Chad Johnson
University of British Columbia
Vancouver, Canada

Bas A Masri
University of British Columbia
Vancouver, Canada
This issue was created by Word+Vision Media Productions, Switzerland
References
- Hodson R. Precision Medicine. Nature Outlook. 2016 Sep;537(7619): Editorial. Available at: https://www.nature.com/articles/537S49a.pdf. Accessed January 22, 2019.
- Wikipedia. Precision Medicine. Wikipedia. Available at: https://en.wikipedia.org/wiki/Precision_medicine. Accessed January 22, 2019.
- The White House. The Precision Medicine Initiative. The White House - President Barak Obama. 2015 Jan. Available at: https://obamawhitehouse.archives.gov/precision-medicine. Accessed January 22, 2019.
- Pabinger C, Lothaller H, Portner N, et al. Projections of hip arthroplasty in OECD countries up to 2050. HIP International. 2018 May;28(5):498-506.
- Sloan N, Sheth, NP. Projected Volume of Primary and Revision Total Joint Arthroplasty in the United States, 2030-2060. Paper presented at: 2018 Annual Meeting Center - Research News. American Academy of Orthopedic Surgeons AAOS. Available at: http://aaos-annualmeeting-presskit.org/2018/research-news/sloan_tjr/. NA. Accessed January 22, 2019.
- Sorokina Y. Personalized Hip and Knee Replacements: U.S. Manufacturers Battle for Innovation Spotlight. 2018 Sep 13. Available at: https://www.odtmag.com/contents/view_online-exclusives/2018-09-13/personalized-hip-and-knee-replacements-us-manufacturers-battle-for-innovation-spotlight/48615. Accessed January 22, 2019.
- Golish SR, Kurtz SM, and Boyan BD. Can 3D Printing Revolutionize Orthopaedic Devices? AAOS NOW. 2018 Jan. Available at: https://www.aaos.org/AAOSNow/2018/Jan/Cover/cover01/?ssopc=1. Accessed January 22, 2019.
- Badarudeen S, Shu A, Ong K, et al. Complications After Revision Total Hip Arthroplasty in the Medicare Population. J Arthroplasty. 2017 Jun;32(6):1954-1958.
- Journé A, Sadaka J, Bélicourt C, et al. New method for measuring acetabular component positioning with EOS imaging: feasibility study on dry bone. Int Orthop. 2012 Nov;36(11):2205–2209.
- Ng VY, Kean JR, Glassman AH. Limb-length discrepancy after hip arthroplasty. J Bone Joint Surg Am. 2013 Aug;95(15):1426-1436.
- Lecoanet P, Vargas M, Pallaro J, et al. Leg length discrepancy after total hip arthroplasty: Can leg length be satisfactorily controlled via anterior approach without a traction table? Evaluation in 56 patients with EOS 3D. Orthop Traumatol Surg Res. 2018 Dec;104(8):1143-1148.
- Pathak P, Gupta R, Meena H, et al. Limb length discrepancy after total hip arthroplasty: a systematic review. Int J Res Orthop. 2018 Sep;4(5):690-697.
- Colgan G, Walsh M, Bennett D, et al. Gait analysis and hip extensor function early post total hip replacement. J Orthop. 2016 Sep;13(3):171-176.
- Bennett D, Ryan P, O'Brien,S,et al. Gait kinetics of total hip replacement patients-A large scale, long-term follow-up study. Gait Posture. 2017 Mar;53:173-178.
- Foucher K. Gait abnormalities before and after total hip arthroplasty differ in men and women. J Biomed. 2016 Oct;49(14):3582-3586.
- Ardestani MM, Amenábar Edwards PP, Wimmer MA. Prediction of Polyethylene Wear Rates from Gait Biomechanics and Implant Positioning in Total Hip Replacement.Clin Orthop Relat Res. 2017 Aug;475(8):2027-2042.
- Madsen MS, Ritter MA, Morris HH, et al. The effect of total hip arthroplasty surgical approach on gait. J Orthop Res. 2004 Jan;22(1):44-50.
- Regenexx. The Age of Patients Getting Knee and Hip Replacements Continues to Decrease. 2018 Mar 27. Available at: https://www.regenexx.com/blog/knee-and-hip-replacements-in-younger-patients/. AccessedJanuary 27, 2019.
- Bayliss L, Culliford D, Pau A, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017 Apr;389(10077):1424–1430.
- Schreurs W, Hannink G. Total joint arthroplasty in younger patients: heading for trouble? Lancet. 2017 Feb;389(10077):1374-1375.
- Lee P, Lakstein D, Lozano B, et al. Mid-to long-term results of revision total hip replacement in patients aged 50 years or younger. Bone Joint J. 2014 Aug;96-B(8);1047-1051.
- Lin YT, Wu JS, Chen JH. The study of wear behaviors on abducted hip joint prostheses by an alternate finite element approach. Comput Methods Programs Biomed. 2016 Jul;131:143-155.
- Werner BC, Brown TE. Instability after total hip arthroplasty. World J Orthop. 2012 Aug;3(8):122-130.
- Dargel J, Oppermann J, Brüggemann G, et al. Dislocation Following Total Hip Replacement. Dtsch Arztebl Int. 2014 Dec;111(51-52):884–890.
- Ezquerra L, Quilez M, Pérez M, et al. Range of Movement for Impingement and Dislocation Avoidance in Total Hip Replacement Predicted by Finite Element Model. J Med Biol Eng. 2017 Jan;37(1):26-34.
- Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002 Apr;17(3):282-288.
- Brooks P. Dislocation following total hip replacement: causes and cures. Bone Joint J. 2013 Nov;95-B(11 Suppl A);67-69.
- Scheerlinck T. Cup positioning in total hip arthroplasty. Acta Orthop Belg. 2014 Sep;80(3):336-47.
- Rivière C, Lazic S, Villet L, et al. Kinematic alignment technique for total hip and knee arthroplasty: The personalized implant positioning surgery. EFORT Open Rev. 2018;3(3):98-105.
- Echeverri S, Leyvraz P, Zambelli P, et al. Reliable acetabular cup orientation with a new gravity-assisted guidance system. J Arthroplasty. 2006 Apr;21(3):413-419.
- Harrison CL, Thomson AI, Cutts S, et al. Research Synthesis of Recommended Acetabular Cup Orientations for Total Hip Arthroplasty. J Arthroplasty. 2014 Feb;29(2):377-382.
- Bosker B, Verheyen C, Horstmann W, et al. Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch Orthop Trauma Surg. 2007 Jul;127(5):375-379.
- Parcells B. Cup Placements: THA Technique. Available at: https://hipandkneebook.com/tha-chapters/2017/3/1/basic-hip-biomechanics. Accessed January 29, 2019.
- Beverland DE, ONeill CKJ, Rutherford M, et al. Placement of the acetabular component. The Bone & Joint Journal. 2016 Jan:98-B(1 Suppl A):37-43.
- Snijders TE, Schlösser TPC, van Gaalen SM, et al. Trigonometric Algorithm Defining the True Three-Dimensional Acetabular Cup Orientation Correlation Between Measured and Calculated Cup Orientation Angles. JBJS Open Access. 2018 Sept:3(3);p e0063
- Karadsheh M. Hip Biomechanics. Orthobullets. Available at: https://www.orthobullets.com/recon/9064/hip-biomechanics. Accessed February 27, 2019.
- Harris MD, MacWilliams BA, Bo Foreman K, et al. Higher medially-directed joint reaction forces are a characteristic of dysplastic hips: A comparative study using subject-specific musculoskeletal models. J Biomech. 2017 Mar;54:80-87.
- Bhaskar D, Rajpura A, Board T. Current Concepts in Acetabular Positioning in Total Hip Arthroplasty. Indian J Orthop. 2017 Jul;51(4):386-396.
- Bonnin MP, Archbold PH, Basiglini L, et al. Do we medialise the hip centre of rotation in total hip arthroplasty? Influence of acetabular offset and surgical technique. Hip Int. 2012 Jul-Aug;22(4):371-378.
- Fraysse F, Arnold J, Thewlis D. A method for concise reporting of joint reaction forces orientation during gait. J Biomech. 2016 Oct;49(14):3538-3542.
- Terrier A, Florencio FL, Rüdiger HA. Benefit of Cup Medialization in Total Hip Arthroplasty is Associated With Femoral Anatomy. Clin Orthop Relat Res. 2014 Oct;472(10):3159–3165.
- Cassidy KA, Noticewala MS, Macaulay W, et al. Effect of femoral offset on pain and function after total hip arthroplasty. J Arthroplasty. 2012 Dec;27(10):1863-1869.
- Houcke JV, Khanduja V, Pattyn C, et al. The History of Biomechanics in Total Hip Arthroplasty. Indian J Orthop. 2017 Jul-Aug;51(4):359-367.
- Naal FD, Kain MSH, Hersche O, et al. Clinical Orthopaedics and Related Research. 2009 Feb;467(4):923-928.
- Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop Relat Res. 1970 Sep-Oct; 72():7-21.
- Charnley J. Low Friction Arthroplasty of the Hip – Theory and Practice. Berlin, Heidelberg: Springer-Verlag; 1979.
- Asayama I, Chamnongkich S, Simpson KJ, et al. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005 Jun;20(4):414-420.
- Bonnin MP, Archbold PH, Basiglini L, et al. Should the acetabular cup be medialised in total hip arthroplasty. Hip Int. 2011 Jul-Aug;21(4):428-435.
- Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007 Aug;89(8):1832-1842.
- Sexton SA, Yeung E, Jackson MP, et al. The role of patient factors and implant position in squeaking of ceramic-on-ceramic total hip replacements. J Bone Joint Surg Br. 2011 Apr;93(4):439-442.
- Hart AJ, Buddhdev P, Winship P, et al. Cup inclination angle of greater than 50 degrees increases whole blood concentrations of cobalt and chromium ions after metal-on-metal hip resurfacing. Hip Int. 2008;18:212–219.
- Shoji T, Yamasaki T, Izumi S, et al. The effect of cup medialization and lateralization on hip range of motion in total hip arthroplasty. Clin Biomech. 2018 Aug;57:121-128.
- Breusch SJ, Malchau H, Older J. Acetabulum. In: The Well-Cemented Total Hip Arthroplasty. Springer, Berlin, Heidelberg; 2005.
- Bicanic G, Barbaric K, Bohacek I, et al. Current concept in dysplastic hip arthroplasty: Techniques for acetabular and femoral reconstruction. World J Orthop. 2014 Sep;5(4):412-424.
- Flecher X, Ollivier M, Argenson JN. Lower limb length and offset in total hip arthroplasty. Orthop Traumatol Surg Res. 2016 Feb;102(1 Suppl):S9-20.
- Pathak PK, Gupta RP, Meena HS, et al. Limb length discrepancy after total hip arthroplasty: a systematic review. Int J Res Orthop. 2018 Sep;4(5)690-697.
- McWilliams AB, Grainger AJ, O'Connor PJ, et al. A review of symptomatic leg length inequality following total hip arthroplasty. Hip Int. 2013 Jan-Feb;23(1):6-14.
- Knutson GA. Anatomic and functional leg-length inequality: A review and recommendation for clinical decision-making. Part I, anatomic leg-length inequality: prevalence, magnitude, effects and clinical significance. Chiropr Osteopat. 2005; 13: 11. Published online 2005 Jul 20.
- Parvizi J, Sharkey PF, Bissett GA, et al. Surgical treatment of limb-length discrepancy following total hip arthroplasty. J Bone Joint Surg Am. 2003 Dec;85-A(12):2310–2317.
- Archbold P, Mohammed M, O’Brien S, et al. Limb length Restoration Following Total Hip Arthroplasty – Using the Transverse Acetabular Ligament and Caliper to Control the Height of the Acetabular and Femoral Components Respectively. Orthopaedic Proceedings. 2006; 88-B:SUPP_II: 281-281.
- Lee C, Jang J, Kim HW, et al. Three-dimensional analysis of acetabular orientation using a semi-automated algorithm. Computer Assisted Surgery. Published online 2019 Jan;DOI: 10.1080/24699322.2018.1545872.
- Maruyama M, Feinberg JR, Capello WN, et al. Morphologic Features of the Acetabulum and Femur: Anteversion Angle and Implant Positioning. Clin Orthop Relat Res. 2001 Dec;393:52-65. Presented at: 29th Open Meeting of the Hip Society and the American Association of Hip and Knee Surgeons: The Frank Stinchfield Award.
- Stem ES, O'Connor MI, Kransdorf MJ, et al. Computed tomography analysis of acetabular anteversion and abduction. Skeletal Radiol. 2006 Jun;35(6):385-389.
- Vanrusselt J, Vansevenant M, Vanderschueren G, et al. Postoperative radiograph of the hip arthroplasty: what the radiologist should know. Insights Imaging. 2015;6(6):591-600
- Lewinnek G, Lewis J, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978 Mar;60(2):217-220.
- McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990 Dec;261:159-170.
- Abdel M, von Roth P, Jennings M, et al. What Safe Zone? The Vast Majority of Dislocated THAs Are Within the Lewinnek Safe Zone for Acetabular Component Position. Clin Orthop Relat Res. 2016 Feb;474(2):386-391.
- Seagrave KG, Troelsen A, Malchau H, et al. Acetabular cup position and risk of dislocation in primary total hip arthroplasty: A systematic review of the literature. Acta Orthop. 2017 Feb; 88(1):217-220.
- Donnelly WJ, Crawford RW, Rimmington TD, et al. Acetabular Cup Placement, Are We Accurate? Orthopedic Proceedings. 2004 Apr:86-B(SUPP_IV);474.
- Murphy WS, Yun HH, Hayden B, et al. The Safe Zone Range for Cup Anteversion Is Narrower Than for Inclination in THA. Clin Orthop Relat Res. 2018 Feb;476(2):325-335.
- Yoon YS, Hodgson AJ, Tonetti J, et al. Resolving inconsistencies in defining the target orientation for the acetabular cup angles in total hip arthroplasty. Clin Biomech. 2008 Mar;23(3):253-259.
- Parcells B. Biomechanics. Available at: https://hipandkneebook.com/tha-chapters/2017/3/1/basic-hip-n?rq=pelvic%20tilt. Accessed February 9, 2019.
- Schwarz TJ, Weber M, Dornia C, et al. Correction of Pelvic Tilt and Pelvic Rotation in Cup Measurement after THA - An Experimental Study. Rofo. 2017 Sep;189(9):864-873.
- Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008 Feb;90(2):357-365.
- Digioia AM, Jaramaz B, Blackwell M, et al. The Otto Aufranc Award. Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop Relat Res. 1998 Oct:355;8-22.
- Marques CJ, Martin T, Kochman A, et al. Pelvic Tilt Angle Differences Between Symptom-Free Young Subjects and Elderly Patients Scheduled for THA: The Rationale for Tilt-Adjusted Acetabular Cup Implantation. Open Orthop J. 2018 Aug:12(1):364-372.
- Lembeck B, Mueller O, Reize P, et al. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005 Aug;76(4):517-523.
- Zhu J, Wan Z, Dorr LD. Quantification of pelvic tilt in total hip arthroplasty. Clin Orthop Relat Res. 2010 Feb;468(2):571–575.