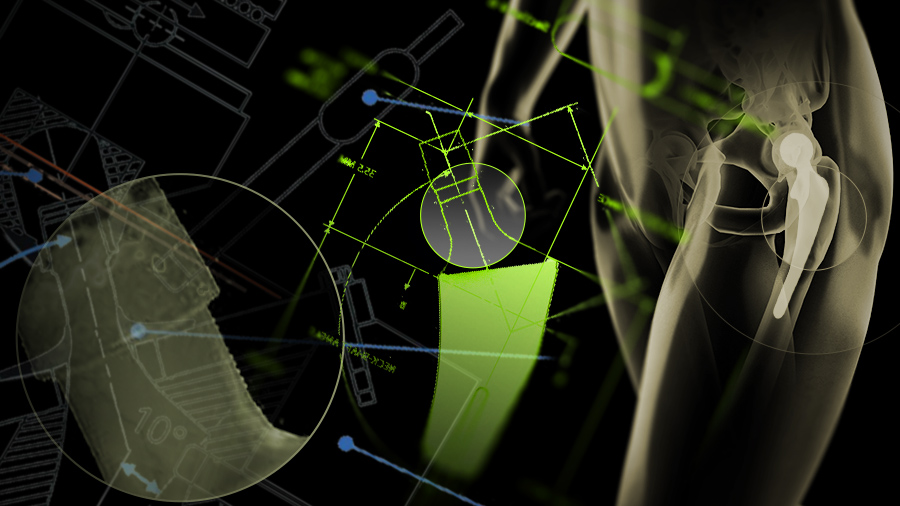
How to diagnose taper corrosion
Preview
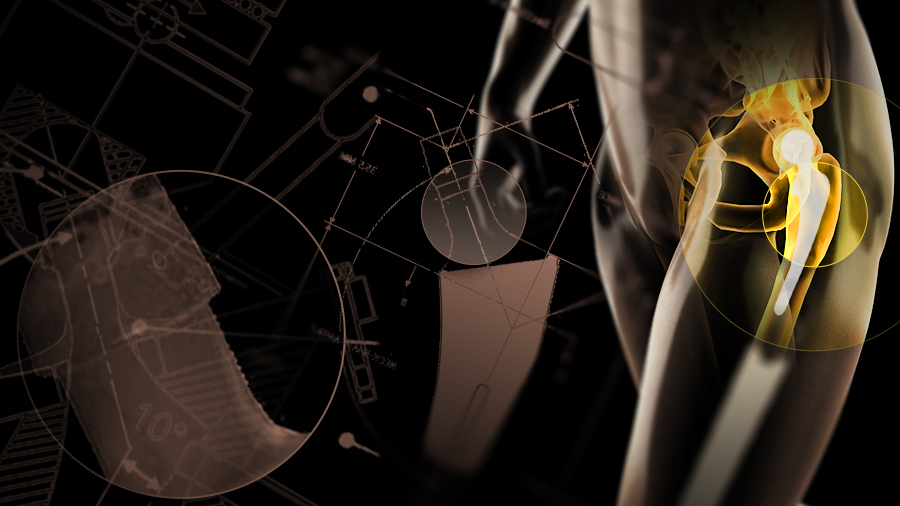
Taper junction corrosion in total hip replacements is a growing concern; it is also a multi-faceted problem. With both asymptomatic and symptomatic patient groups, what indications should a surgeon look for when corrosion is suspected? While there is not a single test to isolate corrosion problems, a spectrum of diagnostic tools have been suggested to make a diagnosis.
Corrosion of the head-neck or taper junction in modular total hip implants has increasingly been reported [1, 2]. While several co-mingling factors have been identified as contributors to the problem (see Part I of this article series), patients may or may not display symptoms, which can make it challenging to identify corrosion through symptoms. In some cases, corrosion has not been identified or confirmed until during revision, and these patients may experience higher rates of complications [3]. Symptoms patients may display cover a broad range and include, but are not limited to: pain, instability, elevated serum metal levels, adverse local tissue reactions (ALTR), swelling, in rare cases neurological changes, and more.
It can take upwards of eight months to establish corrosion as a diagnosis and perform retrieval [4] and Kwon cautions against overreliance on any single diagnostic tool [5]. Here we look at a selection of clinical indicators that may help identify or eliminate corrosion and/or associated metal toxicity as a cause for concern.
Read the full article with your AO login
- When to suspect corrosion
- Pain as a possible initial symptom
- Is it an infection?
- Serum metal levels may be elevated
- Evidence of adverse local tissue reaction?
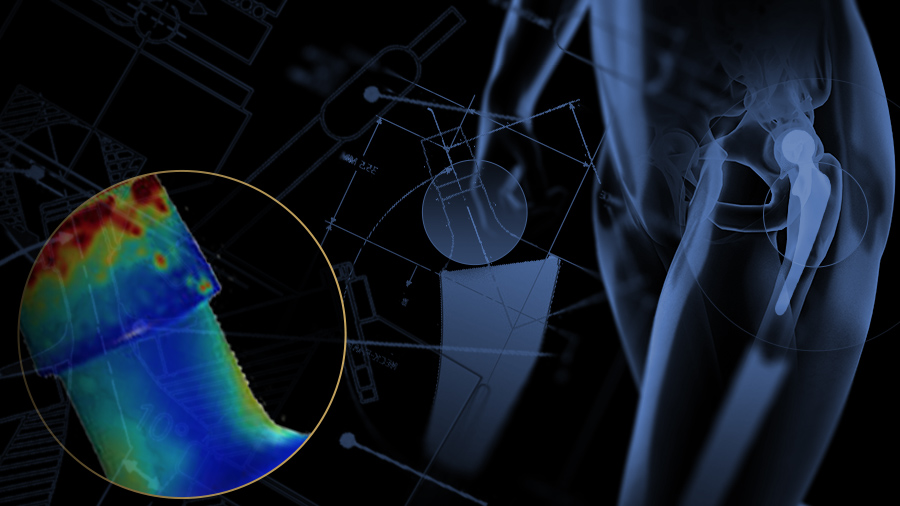
- Use of imaging technology
- Rare cases
- Conclusion
- References
Additional AO resources
Access videos, tools, and other assets to learn more about this topic.
- Upcoming events: AO Recon Course finder
Contributing experts
This series of articles was created with the support of the following specialists (in alphabetical order):

Moussa Hamadouche
Cochin University Hospital
Paris, France

Michael Morlock
Hamburg University of Technology
Hamburg, Germany
Carsten Perka
Charité—University Medicine Berlin
Berlin, Germany
This issue was created by Word+Vision Media Productions, Switzerland
References
- McGrory BJ, McKenney BR. Revision for taper corrosion at the head-neck junction: pearls and pitfalls. Curr Rev Musculoskelet Med. 2016 Mar;9(1):97-102.
- Morlock M, Bünte D, Gührs J, et al. Corrosion of the head-stem taper junction—Are we on the verge of an epidemic? HSS J. 2016 Oct;12(3).
- Lash NJ, Whitehouse MR, Greidanus NV, et al. Delayed dislocation following metal-on-polyethylene arthroplasty of the hip due to 'silent' trunnion corrosion. Bone Joint J. 2016 Feb;98-B(2):187-193.
- Cooper HJ, Della Valle CJ, Berger RA, et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012 Sep 19;94(18):1655-1661.
- Kwon YM. Evaluation of the painful dual taper modular neck stem total hip arthroplasty: Do they all require revision? J Arthroplasty. 2016 Jul;31(7):1385-1389.
- Jennings J, Dennis D, Yang C. Corrosion of the head-neck junction after total hip arthroplasty. J Am Acad Orthop Surg. 2016 Jun;24(6):349-356.
- Whitehouse MR, Endo M, Zachara S, et al. Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: the risk of misdiagnosis. Bone Joint J. 2015 Aug;97-B(8):1024-1030.
- Weiser MC, Chen DD. Revision for taper corrosion at the neck-body junction following total hip arthroplasty: pearls and pitfalls. Curr Rev Musculoskelet Med. 2016 Mar; 9(1): 75–83.
- Lanting BA, MacDonald SJ. The painful total hip replacement: diagnosis and deliverance. Bone Joint J. 2013 Nov;95-B(11 Suppl A):70-73.
- Hussenbocus S, Kosuge D, Solomon LB, et al. Head-neck taper corrosion in hip arthroplasty. Biomed Res Int. 2015:758123. Available at: https://www.hindawi.com/journals/bmri/2015/758123/. Accessed October 21, 2016.
- Nam D, Nunley RM, Sauber TJ, et al. Incidence and Location of Pain in Young, Active Patients Following Hip Arthroplasty. J Arthroplasty. 2015 Nov;30(11):1971-1975.
- Matsen Ko L, Coleman JJ, Stas V, et al. Iliopsoas irritation as presentation of head-neck corrosion after total hip arthroplasty: a case series. Orthop Clin North Am. 2015 Oct;46(4):461-468.
- Fehring KA, Fehring TK. Modes of failure in metal-on-metal total hip arthroplasty. Orthop Clin North Am. 2015 Apr;46(2):185-192.
- Cooper JH, Urban RM, Wixson RL. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013 May 15; 95(10): 865–872.
- Prieto HA, Berbari EF, Sierra RJ. Acute delayed infection: increased risk in failed metal on metal total hip arthroplasty. J Arthroplasty. 2014 Sep;29(9):1808-1812.
- Cooper JH, Urban RM, Wixson RL. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013 May 15; 95(10): 865–872.
- Levine BR, Hsu AR, Skipor AK, et al. Ten-year outcome of serum metal ion levels after primary total hip arthroplasty: a concise follow-up of a previous report*. J Bone Joint Surg Am. 2013 Mar 20;95(6):512-8.
- Wyles CC, McArthur BA, Wagner ER, et al. Ceramic femoral heads for all patients? An argument for cost containment in hip surgery. Am J Orthop (Belle Mead NJ). 2016 Sep/Oct;45(6):E362-E366.
- Kwon YM, Fehring TK, Lombardi AV, et al. Risk stratification algorithm for management of patients with dual modular taper total hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons and the Hip Society. J Arthroplasty. 2014 Nov; 29(11):2060-2064.
- Fehring TK, Carter JL, Fehring KA, et al. Cobalt to chromium ratio is not a key marker for adverse local tissue reaction (ALTR) in metal on metal hips. J Arthroplasty. 2015 Sep; 30(9 Suppl):107-109.
- Pritchett J. Metallosis of the Resurfaced Hip. Available at: http://www.pritchettorthopedics.com/articles/pritchett_metallosis_of_the_hip.pdf Accessed October 21, 2016.
- Bisseling P, de Wit BW, Hol AM, et al. Similar incidence of periprosthetic fluid collections after ceramic-on-polyethylene total hip arthroplasties and metal-on-metal resurfacing arthroplasties: results of a screening metal artefact reduction sequence-MRI study. Bone Joint J. 2015 Sep;97-B(9):1175-1182.
- Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979 Jun;(141):17-27.
- Toms AP, Marshall TJ, Cahir J, et al. MRI of early symptomatic metal-on-metal total hip arthroplasty: a retrospective review of radiological findings in 20 hips. Clinical Radiology. 2008 63(1):49–58.
- Tower S. Arthroprosthetic cobaltism: identification of the at-risk patient. Alaska Med. 2010 Sep;52:28-32.
- Martin JR, Spencer-Gardner L, Camp CL, et al. Cardiac cobaltism: a rare complication after bilateral metal-on-metal total hip arthroplasty. [Case report] Arthroplasty Today. 2015 Dec;1(4):99-102. Available at: http://www.sciencedirect.com/science/article/pii/S2352344115000710 Accessed October 21, 2016.