TN-Advanced Tibial Nailing System
Christopher Finkemeier, Martin Hessmann, Mark Lee, Andrew Oppy, Karl Stoffel
Intramedullary nailing is becoming increasingly popular for proximal and especially distal tibial fracture fixation. However, expanding the nailing indications toward metaphyseal tibial fractures results in the challenge to fix short bone fragments with adequate stability. The new TN-Advanced (TN-A) Tibial Nailing System was specifically designed to address these issues. The new nail has preassembled polyether ether ketone inlays in the proximal and distal parts of the nail. When locking screws are inserted the inlays provide angular stability between the locking screws and the nail without the need for additional instruments and surgical steps.
Several improvements are introduced with the development of a new Low Profile Locking Screw in a headless design. Furthermore, the TN-Advanced Tibial Nailing System provides instruments for the infrapatellar, intraarticular suprapatellar, and extraarticular parapatellar approaches. The new suprapatellar TN-A instrumentation features a compressible and disposable suprapatellar sleeve that is designed to reduce the pressure on the patellofemoral joint whenever possible.
Defining the clinical problem
In 2016, the medical members of the INEG thoroughly reviewed the clinical performance of the Expert Tibial Nail System (available since 2005) to identify the most important aspects that had to be addressed by a next generation tibial nailing system for improved patient care. Review findings were supported by discussions at our AO TC Trauma Experts' Symposia, verified by published literature, and confirmed by field studies as well as surgeon interviews performed by DePuy Synthes (DPS).
The following outcome-related problems were identified for tibial fracture treatment:
Delayed union, nonunion, and malunion
Intramedullary nailing (IMN) is the most popular and widely used method for treating tibial shaft fractures. From a biomechanical perspective, the nail is a central, load-sharing implant which provides high stability to support early postoperative patient mobilization. This device specific benefit, together with the advantage of the soft-tissue sparing instrumentation, guided surgeons to expand their nailing indications into the metaphyseal zones of the tibia. While plate fixation is decreasing, IMN is becoming increasingly popular for proximal and especially distal tibial fracture fixation.
Expanding the nailing indications toward metaphyseal tibial fractures results in the challenge to fix short bone fragments with adequate stability to promote bone healing and to avoid secondary loss of reduction. This challenge is pronounced in diminished bone quality, the occurrence of which is increasing because of the aging population. A multicenter study with the Expert Tibial Nail from DPS revealed a 12.2% rate of delayed union at 1 year [1]. A nonunion rate of 12% was reported for reamed IMN in a single-center study with 1003 patients [2]. A systematic review and metaanalysis of IMN versus minimally invasive plate osteosynthesis for distal tibial fractures resulted in a 14.8% malunion rate for nailing which was significantly higher than the 8% malunion rate for plating [3]. All these numbers emphasize the importance to increase the fixation stability provided by IMN to avoid complications and to reduce the reoperation rate.
Patient pain and discomfort
In a recent retrospective observational study, [4] 27% of 126 patients treated with a tibial nail reported pain attributed to locking screws at follow-up. Interlocking screw prominence is a frequent reason for soft-tissue irritations which may require screw removal in a secondary intervention. Contributing factors for soft-tissue irritations are bad soft-tissue coverage (particularly around the distal tibia and in elderly patients), imprecise screw length measurement, and the size/design of the interlocking screw head and tip.
There are further procedure-related aspects that had to be addressed in the development of a new state-of-the-art tibial nailing system:
Anatomical nail fit
It is essential that the nail design is optimized to fit most of the anatomical variations of the tibial canal. Adequate nail fit is essential to facilitate implant placement and to avoid deformities or iatrogenic fractures due to nail insertion. So far, surgeons have used the cannulated Expert Tibial Nail which has been provided in two different nail design versions: (1) nail with 10.5° bend starting at 75 mm proximally with a radius of 376 mm to 1128 mm depending on the nail length; (2) nail with 10.5° bend starting at 65 mm proximally with a fixed radius of 100 mm and a 3° tip bend starting at 57 mm distally (called 'Expert Tibial Nail with Proximal Bend'). The latter has been used more frequently, especially for the treatment of proximal tibial fractures. During the development of a next generation tibial nail the following questions had to be addressed: (1) Is there a more optimal nail design? (2) Is one nail design sufficient or is it required to offer two different nail designs with the inherent portfolio complexity?
Usability aspects
Implant systems should be easy and intuitive to use and to support consistent outcomes by reproducible instrumentation. Surgeon feedback is that some instrumentation steps of the Expert Tibial Nail are perceived as complex. Angular stable locking of the Expert Tibial Nail with the Angular Stable Locking System (ASLS, launched in 2010) is an example. This system requires dedicated ASLS screws, bioresorbable ASLS sleeves, and special instruments to achieve angular stable connections between the locking screws and the nail. The procedural complexity of ASLS contributed to the clinical demand for an easier angular stable locking solution.
Instrumentation for different surgical approaches
The infrapatellar approach in a flexed knee position is regarded as the standard approach for IMN of tibial fractures. However, approaches for semi-extended knee positioning are rapidly gaining popularity: intraarticular suprapatellar approach and extraarticular parapatellar approach. They can improve the surgeon's ability to obtain, maintain, and with image intensification evaluate fracture reduction, especially in proximal and distal tibial fractures [5]. Also, the semi-extended knee position requires less patient manipulation and eases image intensification during the surgical procedure.
Clinical solutions
TN-Advanced Tibial Nail
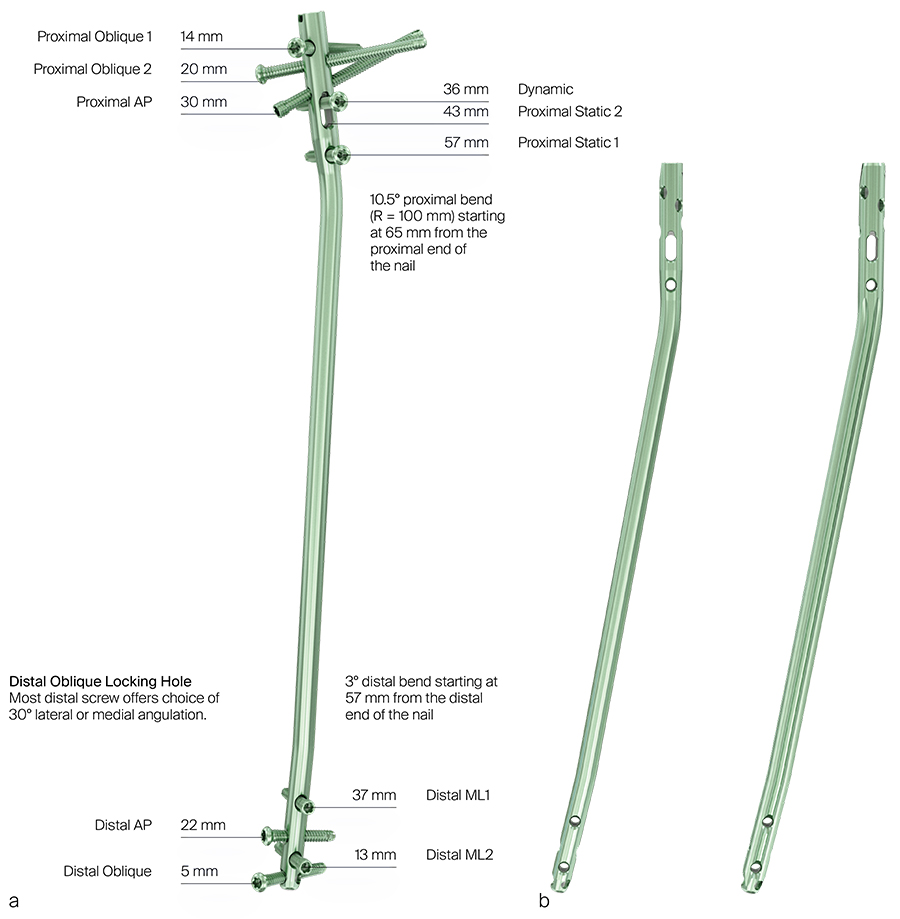
Computed tomographic (CT) based bone models of various patient populations (Caucasian, Asian, male, female, small body size, large body size) were used to investigate the best tibial nail design in terms of anatomical fit by means of computer graphical methods [6, 7]. It was shown that the nail shape of the existing Expert Tibial Nail with Proximal Bend provided an excellent anatomical fit for smooth nail insertion and final nail positioning. The fit was significantly better than the one provided by the other Expert Tibial Nail design version. Based on these study results, it was decided that the new TN-Advanced Tibial Nail (TN-A) should have the same nail shape and locking configurations as the Expert Tibial Nail with Proximal Bend (Fig 1). Furthermore, the anatomical studies revealed that a single nail design is sufficient to address a large variety of patient populations. Offering only one TN-A shape helps to reduce the nail inventory and to simplify the nailing system.
The TN-A is offered in the following nail diameters: 8.2 mm, 9 mm, 10 mm, 11 mm, 12 mm and 13 mm. The proximal nail diameter is 11 mm for all nails with nail shaft diameters from 8.2 mm to 11 mm. For larger nail sizes the proximal nail diameter is the same as the nail shaft diameter. The following nail lengths are available: 255 mm to 465 mm in 15 mm length increments. The TN-A is made of a different material (TAV, Ti-6Al-4V) compared with the Expert Tibial Nail (TAN, Ti-6Al-7Nb). Both titanium alloys have similar mechanical properties.
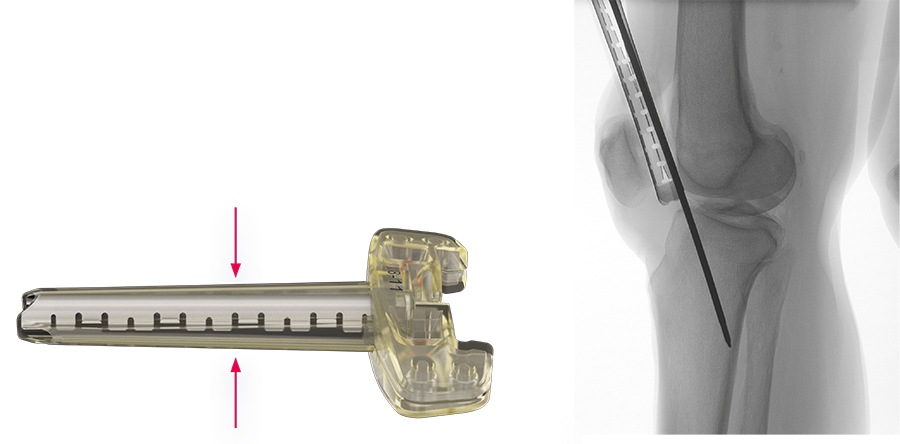
The TN-A has five proximal and four distal multiplanar locking options with an innovative device feature to provide angular stability: there are preassembled polyether ether ketone (PEEK) inlays in the proximal and distal parts of the nail (Fig 2).
Wherever locking screws are inserted in the locking holes of the TN-A (except in the proximal 7 mm nail slot for dynamic and static fixation), the inlays provide angular stability between the locking screws and the nail without the need for additional instruments and surgical steps. The PEEK inlays decrease nail toggle by up to 72% and reduce the risk of screw migration with secondary loss of reduction.
Various preclinical studies were performed to address potential concerns about PEEK debris due to the interaction between the screws and the inlays. Debris particle sizes, shapes, and volumes were analyzed. The amount of debris generated is like the one observed for the MultiLoc Proximal Humeral Nail, which has a preassembled polyethylene inlay. Since its introduction in 2011, no debris issues have been reported for the MultiLoc Proximal Humeral Nail.
The TN-A implants are intended for treatment of fractures in adults and adolescents (12 - 21 years) in which the growth plates have fused. Specifically, the implants are indicated for:
- Open and closed proximal and distal tibial fractures
- Open and closed tibial shaft fractures
- Tibial malunions and nonunions
References
1) Attal R, Hansen M, Kirjavainen M, et al. A multicentre case series of tibia fractures treated with the Expert Tibia Nail (ETN). Arch Orthop Trauma Surg. 2012 Jul;132(7):975-984.
2) Dailey HL, Wu KA, Wu PS, et al. Tibial fracture nonunion and time to healing after reamed intramedullary nailing: risk factors based on a single-center review of 1003 patients. J Orthop Trauma. 2018 Jul;32(7):e263-e269.
3) Liu XK, Xu WN, Xue QY, et al. Intramedullary nailing versus minimally invasive plate osteosynthesis for distal tibial fractures: a systematic review and meta-analysis. Orthop Surg. 2019 Dec; 11(6): 954-965.
4) Beak P, Moudhgalya S, Anderson T, et al. Painful locking screws with tibial nailing, an underestimated complication. Eur J Orthop Surg Traumatol. 2019 Dec;29(8):1795-1799.
5) McAndrew CM, Ricci WM, Miller AN, et al. Distal tibial intramedullary nailing using an extraarticular, lateral parapatellar approach in the semiextended position. J Orthop Trauma. 2018 Aug;32 Suppl 1:S34-S35.
6) Schmutz B, Rathnayaka K, Wullschleger ME, et al. Quantitative fit assessment of tibial nail designs using 3D computer modelling. Injury. 2010 Feb;41(2):216-219.
7) Amarathunga JP, Schuetz MA, Yarlagadda PK, et al. Automated fit quantification of tibial nail designs during the insertion using computer three-dimensional modelling. Proc Inst Mech Eng H. 2014 Dec;228(12):1227-1234.
Locking screws and screwdriver options
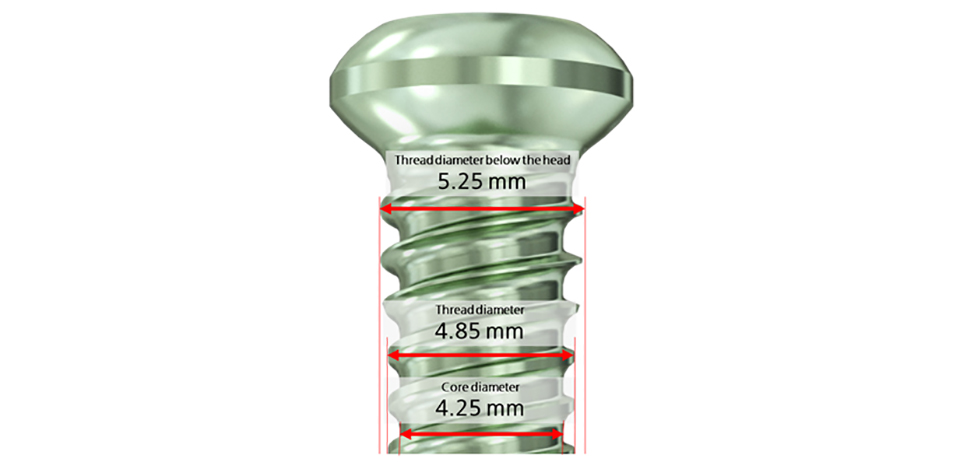
Regarding screw sizes, 5 mm locking screws are used in all locking holes of the TN-A, except for the distal locking holes of the 8.2 mm nail, for which 4 mm locking screws are provided. The use of 5 mm screws in the 9 mm TN-A reduces the screw breakage risk compared with the 9 mm Expert Tibial Nail that relied on 4 mm screws.
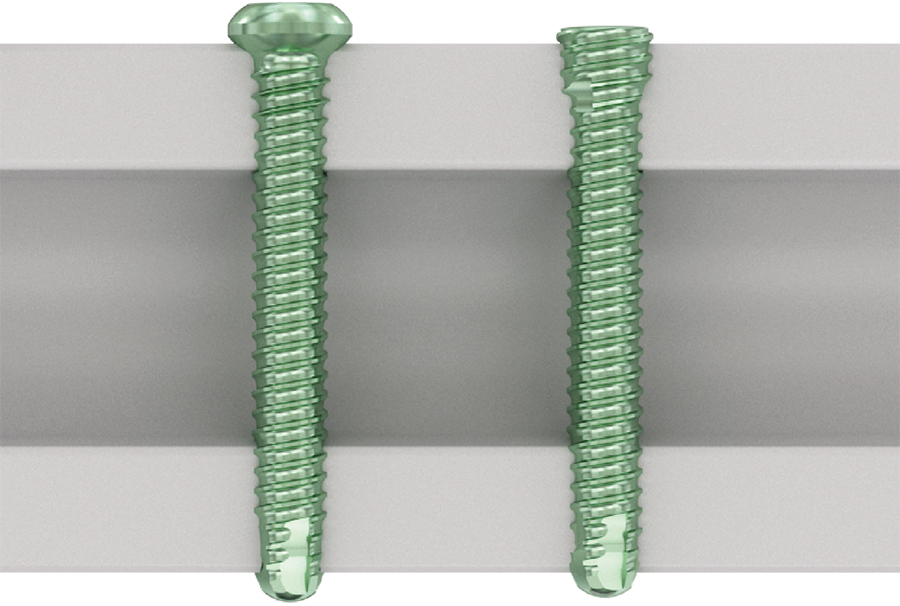
Several improvements are introduced with the development of two new types of locking screws that are compatible across all nails of the Advanced Nailing System (Fig 3).
The new headed Locking Screw (Fig 4) has an increased outer thread diameter portion below the screw head that improves the screw purchase in bone. This aspect is particularly important in poor bone quality and in the presence of thin cortical bone. In addition, modulation of the screw threads provides an improved tactile feedback indicating when the screw is fully seated to avoid inadvertent screw stripping.
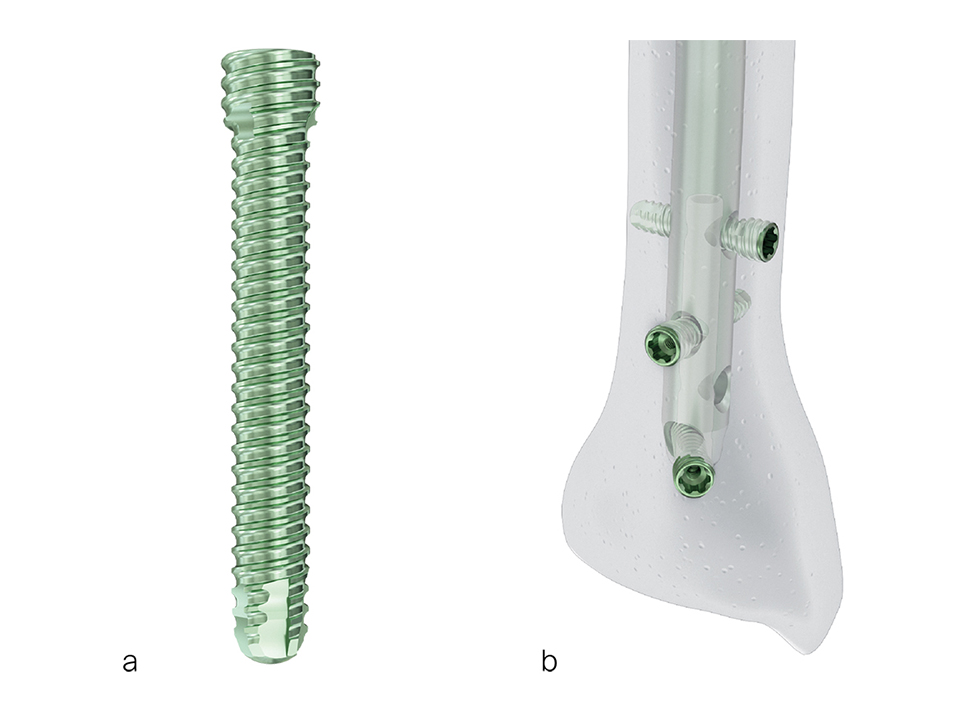
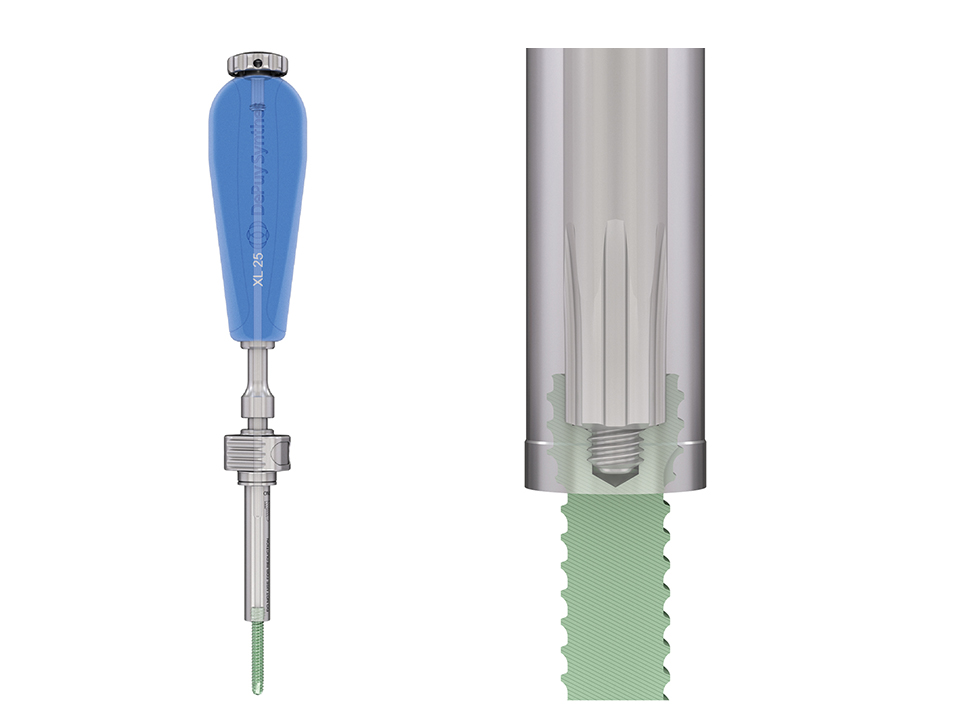
An additional screw type is provided with the Low Profile Locking Screw in a headless design (Fig 5). This novel screw was designed to reduce the risk of soft- tissue damage and irritations due to screw head prominence at areas of low-tissue coverage, eg, the distal tibia. Furthermore, screw purchase is markedly increased by the threaded conical design portion of the Low Profile Locking Screw, which is advantageous in osteoporotic bone.
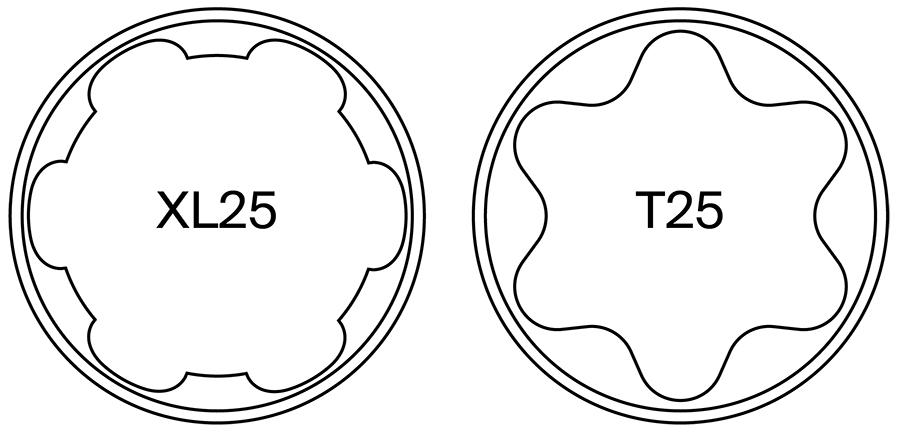
Both locking screw types have a XL25 recess (Fig 6) and self-tapping rounded tips with two extra threads to ease screw insertion and to reduce soft-tissue irritations. All screws have a retaining feature to facilitate instrumentation (Fig 7 and Fig 8).
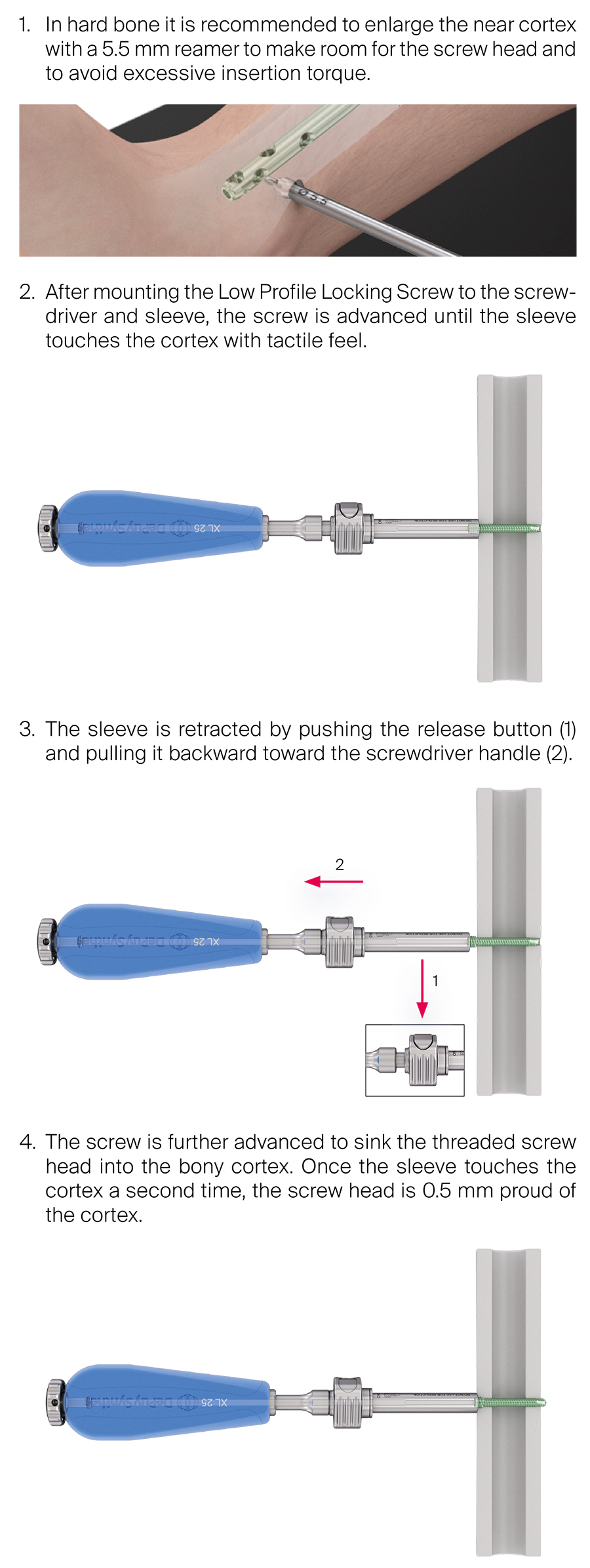
The Low Profile Locking Screw is inserted as described in Fig 9.
In addition to manual screw insertion there is the option to use a power tool for partial screw insertion (Fig 10).
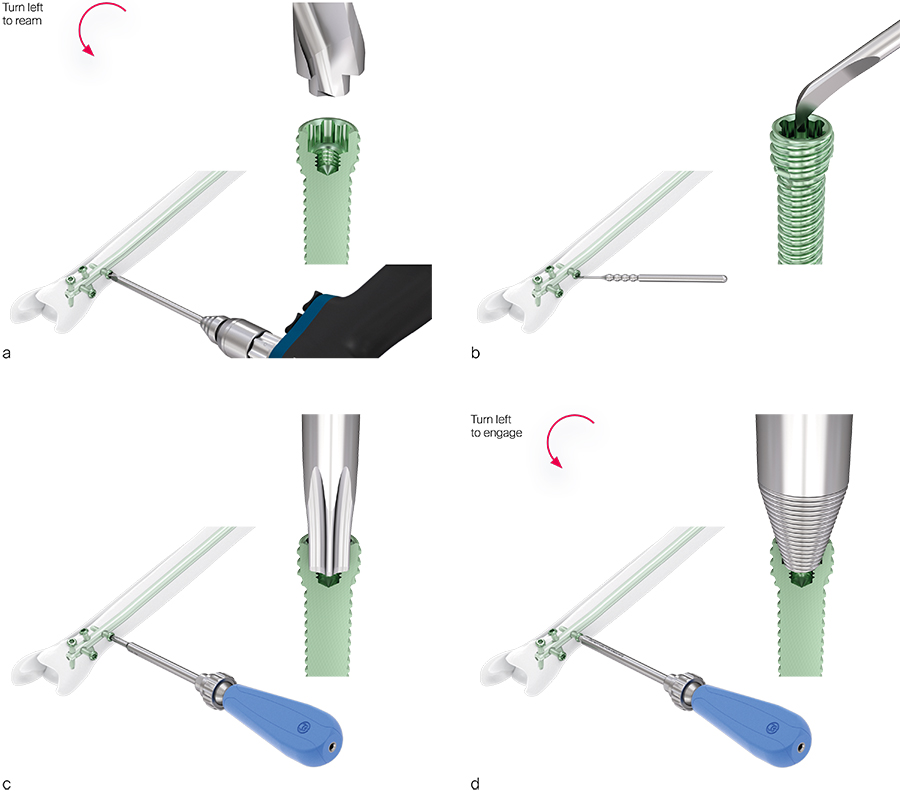
If the screw heads are overgrown or the recess is damaged, additional instruments are available for screw removal (Fig 11 ).
Nailing instruments
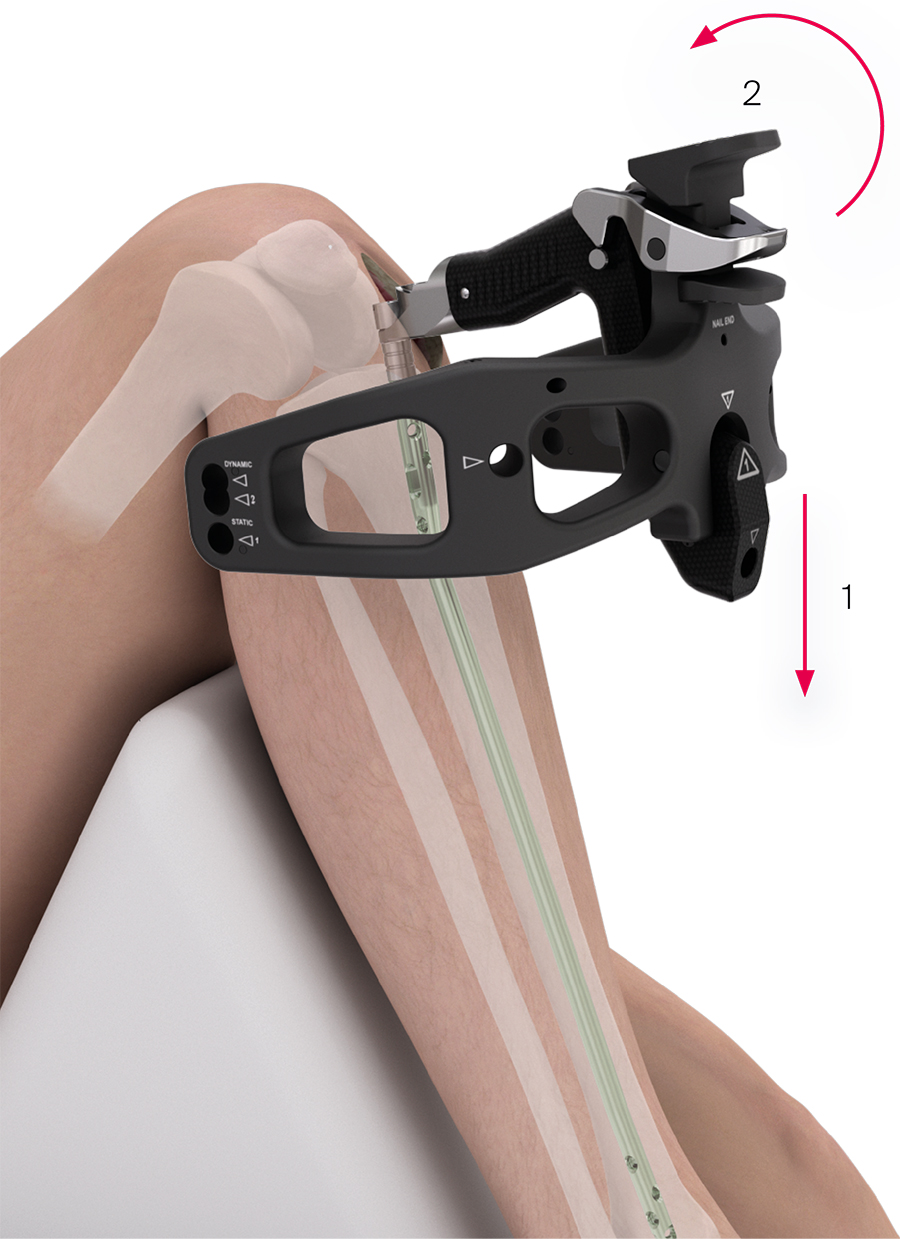
The new nailing instruments were developed to streamline the instrumentation and to eliminate redundancy between nailing system (Fig 1). The TN-A utilizes intuitive instrumentation aimed to improve operating room efficiency. Several innovative solutions address key functionalities of the instrumentation (Fig 2).
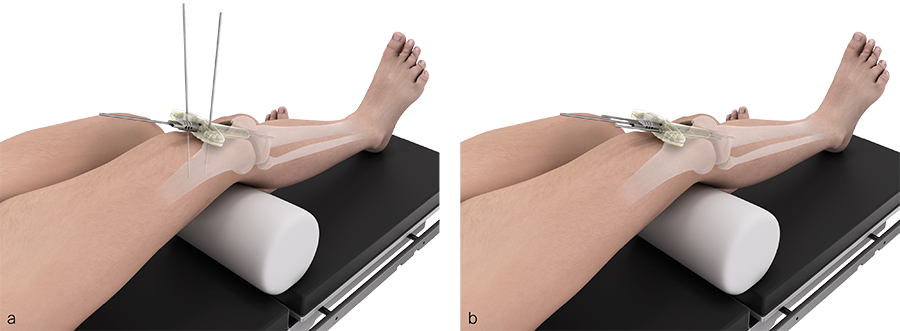
An important aspect for the development of the TN-A instrumentation was to provide instruments for the infrapatellar, intraarticular suprapatellar, and extraarticular parapatellar approaches.
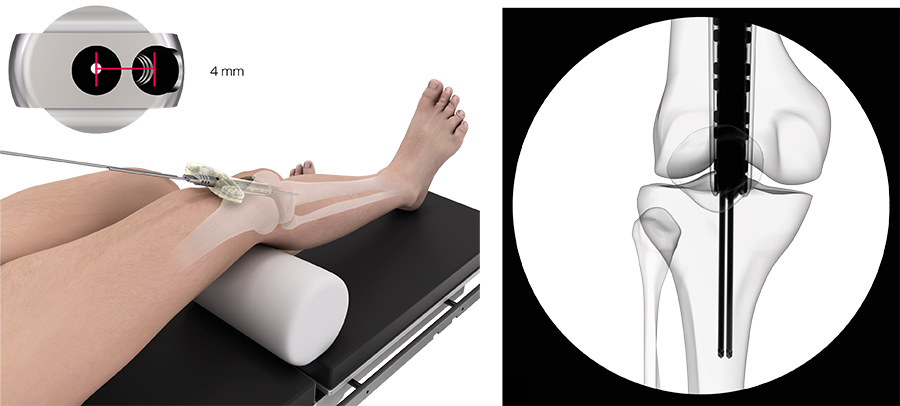
Suprapatellar insertion instruments
Dedicated suprapatellar insertion instruments have been available for the Expert Tibial Nail since 2012. These instruments comprise a soft outer protection sleeve to protect the patellofemoral cartilage and soft tissues as well as an inner metal protection sleeve through which the required cutting and reaming instruments and the nail can be inserted in a safe manner. However, the disadvantage of this instrumentation concept is that the pressure on the patellofemoral joint due to the presence of the sleeves is constantly kept at the same level and for the whole time until the nail is inserted. The new suprapatellar TN-A instrumentation features a compressible and disposable suprapatellar sleeve that is designed to reduce the pressure on the patellofemoral joint whenever possible (Fig 5). The sleeve expands as required by the size of the instruments as these are inserted through it. The compressible sleeve is provided in two sizes: small sleeve for nails with diameters of 8.211 mm and for reamer heads up to 12.5 mm; large sleeve for nails with diameters of 8.213 mm and for reamer heads up to 14.5 mm.
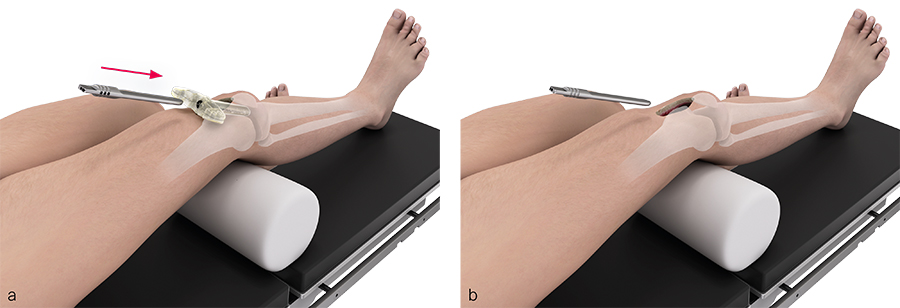
A multihole wire guide can be inserted through the protection sleeve to determine the correct entry point and entry path for the guide wire. This instrument can also be used before the insertion of the protection sleeve, thereby increasing the maneuverability of the wire guide in tight knees (Fig 6). Adjustments to the entry point location can be made by turning the multihole wire guide (Fig 7).
Once the protection sleeve is in its correct position it can be anchored to the femur via the protection sleeve handle using 3.2 mm K-wires. There are alternative protection sleeves available to allow anchoring to the tibial plateau (Fig 8).
The opening drill bit (rigid as well as flexible opening drill bits are available) and the reamers are pushed over the guide wire through the compressible suprapatellar sleeve. Drilling and reaming are supposed not to be started before the cutting instruments are placed down to the bone.
The surgical technique guides for instrumentation the TN-A with the various supported approaches were optimized based on anatomy lab experiences (Fig 9).
The TN-A may be removed by a suprapatellar or by a traditional infrapatellar approach. End cap removal and connection of the removal instrument to the nail is more difficult when using the suprapatellar approach for nail removal.
Innovations in nailing of tibial fractures: Tibia Nail Advanced
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.