LCP Distal Femur Plate for Veterinary Applications
Christoph Lischer, Fabrice Rossignol, Jeffrey P Watkins
Comminuted fractures of the proximal phalanx (P1) are common injuries in horses. All breeds and all activities are affected. The degree of comminution varies but many are so highly comminuted that fracture reconstruction is not feasible. Currently, the recommended treatment for horses suffering from a highly comminuted P1 fracture is to immobilize the distal limb in a transfixation cast. However, the prognosis for survival is guarded and complications are common, including progressive arthropathy of the metacarpophalangeal / metatarsophalangeal and proximal interphalangeal joints as well as support limb laminitis.
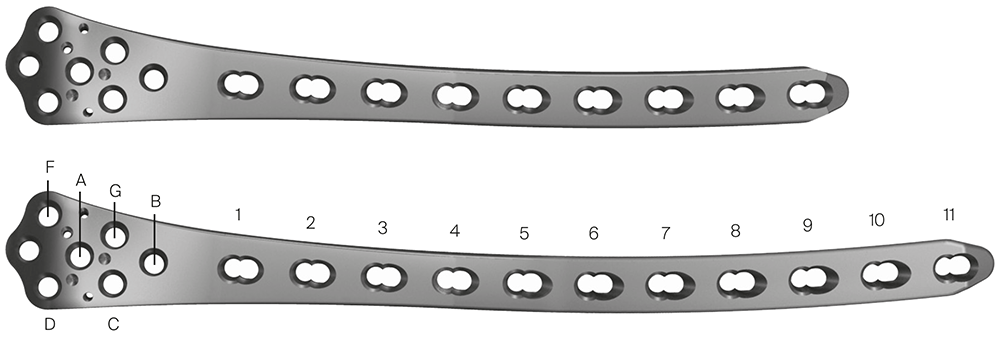
Plate design
The LCP Distal Femur Plate (DFP) is a precontoured, low profile plate that features combi-holes along the shaft accepting 4.5 mm/5.5 mm cortex screws in the dynamic compression unit portion and 5.0 mm locking screws in the threaded portion (Fig 2). The threaded locking holes in the plate head accept 5.0 mm locking screws and 4.5 mm/5.5 mm cortex screws. The LCP DFP, available in a left and a right version, was initially indicated for distal shaft, supracondylar, intraarticular, extraarticular, and periprosthetic fractures in the human femur. Implants and instruments of the LCP DFP are fully compatible with the 4.5/5.0 mm LCP Systems. Recently, the LCP DFP (9- and 11-holes, left and right) has been approved for veterinary applications, specifically for comminuted P1 fractures in horses.
- 9-hole plate (236 mm)
- 11-hole plate (276 mm)
The wide and flattened head of the plate has several locking holes which provides a strong fixation in the proximal aspect of the middle phalanx (P2) and the distal aspect of the P1, distal to the area of major comminution. Furthermore, the curved shape allows abaxial fixation into one of the major fragments in P1 or in the medial or lateral condyle of the distal metacarpus/metatarsus when associated with a concomitant condylar fracture. The low profile of the plate permits placement using less invasive fixation techniques.
The two following cases (both kindly provided by Fabrice Rossignol, Paris, France) demonstrate the surgical procedure which relies on biological osteosynthesis principles with the plate, used as an internal fixator, providing an angle stable construct and durable bridging of the fractured P1. Long-term follow-up regarding biomechanical impact on the distal interphalangeal joint is still required. However, the horses treated thus far have adapted well.
Case 1: Comminuted P1 fracture in a 14-year-old warmblood mare
A 14-year-old Belgian warmblood mare weighing 520 kg was presented with a medical history of severe right forelimb lameness following an unwitnessed paddock injury. Radiographs confirmed a highly comminuted fracture of P1. A distal limb bandage had been applied in an attempt to stabilize the injury before transporting the mare.
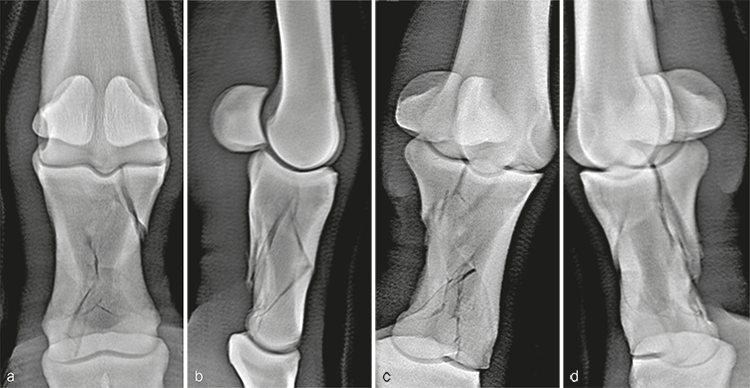
Radiographic evaluation at the time of admission confirmed the highly comminuted fracture configuration and revealed considerable collapse of P1 with malalignment and overriding of the fracture fragments (Fig 3). Due to the highly unstable nature of the injury and the presence of multiple sharp fracture fragments, the immediate concern was the potential for skin penetration and conversion to an open fracture. Consequently, the mare was placed under general anesthesia to facilitate indirect fracture reduction through traction on the distal limb. Once alignment was confirmed radiographically, the distal limb was stabilized by application of a fiberglass cast extending distally from the proximal metacarpus and incorporating the hoof.
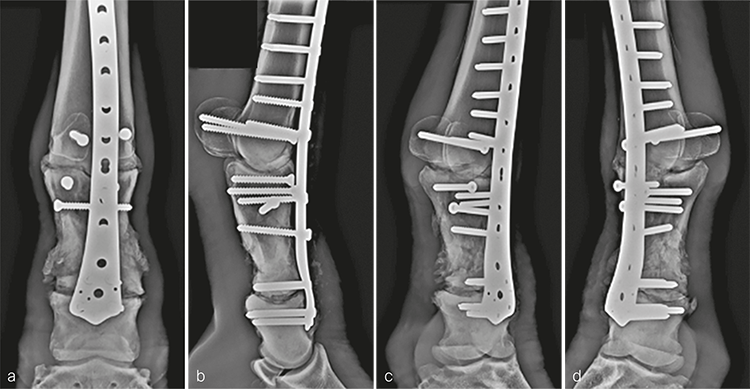
Following recovery from anesthesia, the mare was placed in intensive care for 24 hours to stabilize her physiological status before surgical fixation. Bridging plate fixation of the comminuted P1 fracture in conjunction with arthrodesis of the metacarpophalangeal and proximal interphalangeal joints was accomplished using an LCP DFP (11-holes). Prior to fixation, articular cartilage was debrided from the articulations using a 4.5 mm drill bit and curettes passed through stab incisions. The frontal plane fracture in the proximal aspect of P1 was reduced and stabilized with 5.5 mm cortex screws placed in lag fashion from dorsal to palmar in a slightly distal to proximal orientation.
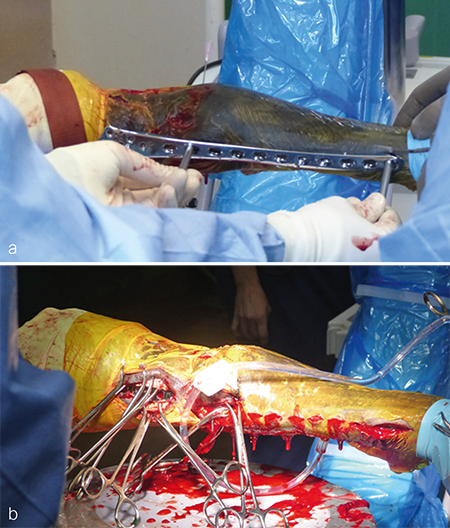
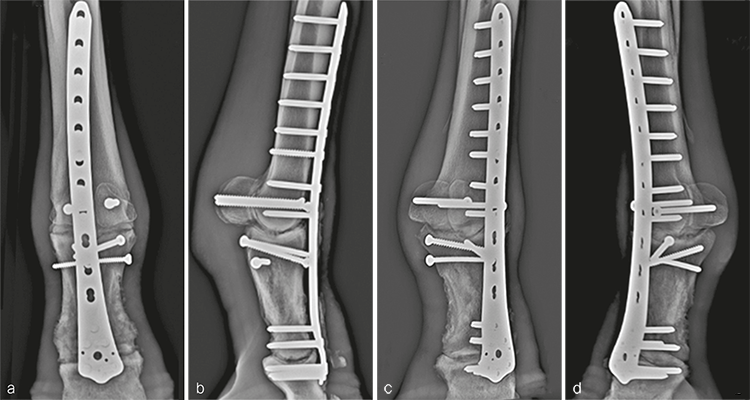
The plate was contoured to the desired 15 of dorsiflexion at the level of the fetlock joint to provide an appropriate joint angle (Fig 4a). Three, approximately 4 cm long dorsal midline incisions were performed through the skin and extensor tendon at the level of the proximal end of the plate, the metacarpophalangeal joint, and at the distal end of the plate overlying the proximal interphalangeal joint. Using a combination of sharp dissection and a large periosteal elevator, a tunnel was created between the bone and overlying soft tissues including the extensor tendon. The plate was inserted into the tunnel and appropriate plate positioning, and cortical alignment were confirmed radiographically. A Push-Pull Reduction Device was placed through hole (A) in the head of the plate at the level of the proximal interphalangeal joint to compress the plate onto the dorsal cortices of the phalanges and maintain alignment of the proximal interphalangeal joint. Five 5.0 mm locking screws were inserted in the expanded head of the plate to purchase the distal aspect of P1 and the proximal aspect of P2. To ensure plate-bone contact proximally, two 5.5 mm cortex screws were placed into the distal aspect of the metacarpus (plate shaft holes 4 and 5). The remaining holes overlying the metacarpus were filled with 5.0 mm locking screws; where possible, 4.5 mm cortex screws were placed through the plate overlying large fragments of the P1. Finally, two 5.5 mm cortex screws were placed in lag fashion abaxial to the plate to engage the medial and lateral proximal sesamoid bones (Fig 5). Screws placed outside of the dorsal midline incisions were placed through additional stab incisions.
The incisions were closed routinely (Fig 4b). The distal limb was placed in a cast, and the patient was assisted in recovery. Surgery time, including casting, was 310 minutes.
The cast was changed 2 weeks postoperatively and removed 1 month following the repair. The distal limb was maintained in a Robert-Jones bandage for 1 additional month. Routine hoof care in conjunction with rocker shoes and silicone padding were initiated at the time of cast removal. The mare made excellent progress postoperatively and was fully weight bearing on the repaired leg immediately. Radiographic evaluation 5 months postoperatively confirmed good fracture healing and progression of the arthrodesis (Fig 6). The mare was returned to paddock activity at this time and was fully functional with only mild mechanical lameness, as expected with arthrodesis of the metacarpophalangeal joint.
Case 2: Comminuted P1 fracture in a 10-year-old warmblood gelding horse
A 10-year-old French warmblood gelding weighing 580 kg was presented a few hours after developing a severe left forelimb lameness following an unwitnessed paddock injury. Initial radiographs demonstrated a severely comminuted, minimally displaced fracture of P1 (Fig 7). The distal limb was immediately placed in a fiberglass cast by the referring veterinarian before transporting the horse, which prevented further displacement of the fragments.
The day following admission, the horse was placed under general anesthesia and bridging plate fracture fixation/arthrodesis was accomplished using an 11-hole LCP DFP as described in case 1. Surgery time was 315 minutes.
Postanesthetic myopathy complicated the patients recovery and necessitated intensive care immediately following surgery. He responded to supportive therapy and improved rapidly. In addition, his comfort level was excellent on his operated leg for the duration of hospitalization. At 3 months postoperatively, clinical evaluation revealed excellent weight bearing on the operated leg (Fig 8a), with mechanical lameness characteristic of horses with a fused metacarpophalangeal joint. The cosmetic appearance of the distal limb was excellent (Fig 8bc). Radiographic examination demonstrated excellent fracture healing with ongoing progress of the arthrodesis in both articulations (Fig 9). He was shoed with rocking shoes and silicone padding on both front feet to facilitate mobility and to provide hoof support.
Biological bridge plating using the human LCP DFP can provide a better alternative to a transfixation cast for surgical management of highly comminuted fractures with fewer complications and better long-term outcomes. The above-mentioned cases are excellent examples of the utility of the LCP DFP for managing catastrophic P1 injuries in adult horses. The fixation allows an early return to weight bearing on the affected limb and thus mitigates complications, such as support limb laminitis, associated with severe, protracted lameness. Furthermore, it limits the duration of external coaptation minimizing the negative effects of long-term cast application. Finally, arthrodesis of the metacarpophalangeal/metatarsophalangeal and proximal interphalangeal joints prevents chronic pain and long-term disability secondary to osteoarthritis.
LCP DFP for veterinary application in comminuted fractures of the P1 in equine
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.