Zero-P Natural Anterior Cervical Plate
Richard Bransford
Zero-P Natural Anterior Cervical Plate
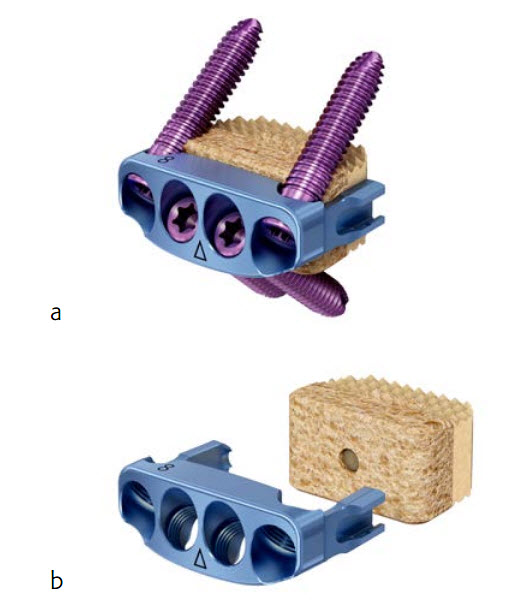
The Zero-P Natural plate is a zero profile anterior cervical plate that provides anterior plate and screw fixation of the cervical spine. The plate is anchored by four locking bone screws, which forms a rigid bone wedge for stability. The plate delivers strength and stability comparable to a traditional cervical plate as demonstrated in mechanical and biomechanical testing [1].
The Zero-P Natural plate was designed for use with the Corticocancellous (CC) Natural allograft spacer processed by the Musculoskeletal Transplant Foundation (MTF) (Fig 1). It features retention arms that are designed to securely attach to the allograft spacer and its height is slightly undersized to the corresponding CC Natural allograft spacer offering potential to avoid stress shielding.
Reference
1. Synthes report: The ZERO-P NATURAL Plate and an MTF CC Natural allograft spacer compared to a one level VECTRA-ONE Cervical Plate with an MTF CC Natural allograft spacer in a cyclic cadaveric range of motion study: ASTM F1717. Test number 0000220895.
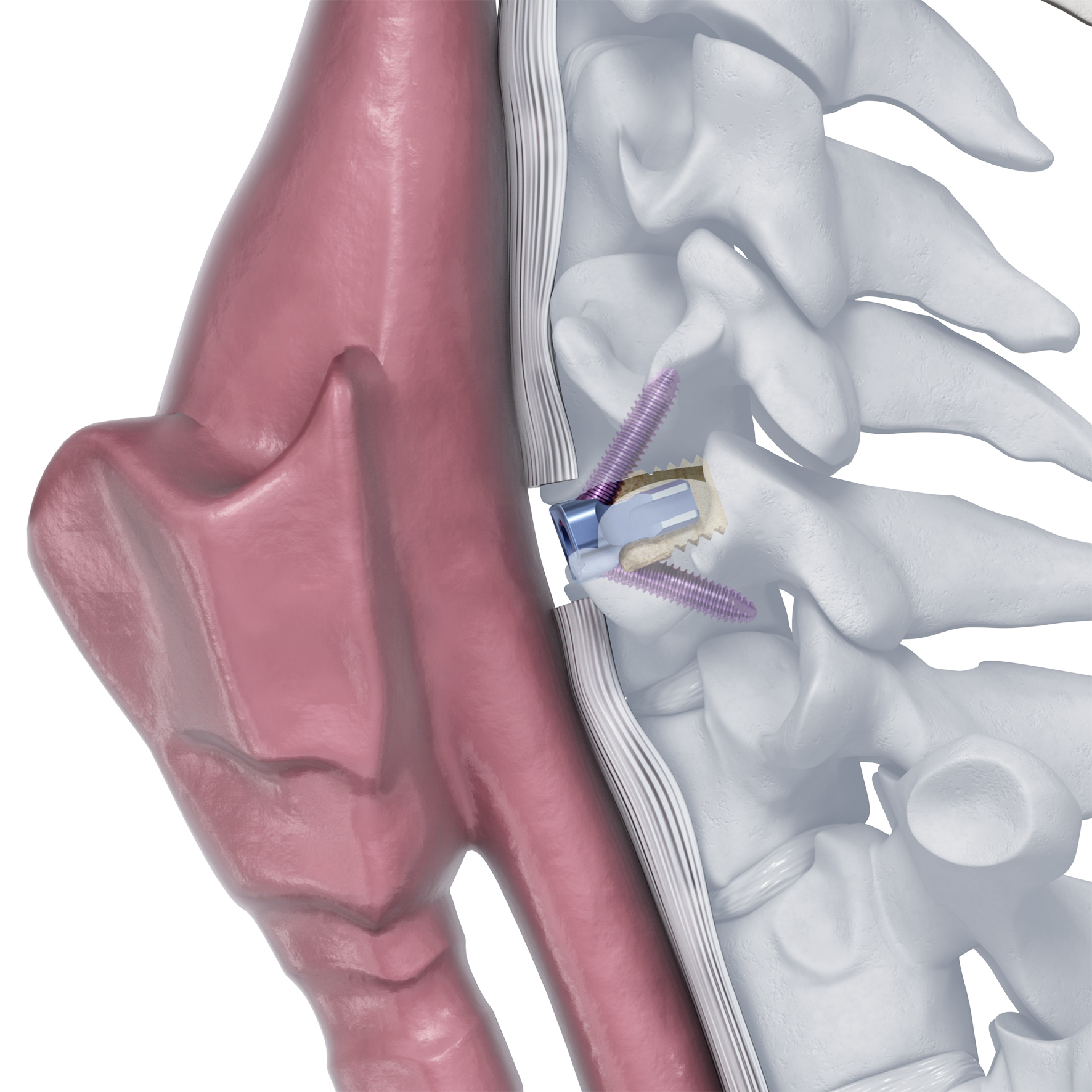
Zero-Profile design to minimize contact with local anatomical structures.
The plate is contained within the excised disc space and does not protrude past the anterior wall of the vertebral body, limiting the risk of damage to vessels and adjacent soft tissue. In addition, preparation of the anterior surface of the vertebral body is not necessary because the plate does not
lie against this surface (Fig 2). It is also designed to prevent contact with adjacent levels. Cervical plates placed near adjacent level discs may contribute to bone formation near or around the adjacent level [2].
Reference
2. Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg (Am). 2005;87:558563.
Ease of use
The Zero-P Natural plate firmly attaches to the allograft spacer. This enables simultaneous insertion for a more streamlined surgical technique. Each plate is supplied sterile-packaged and mounted to an assembly tool that allows the plate to be coupled to the allograft spacer (Fig 3).
Features
Features include:
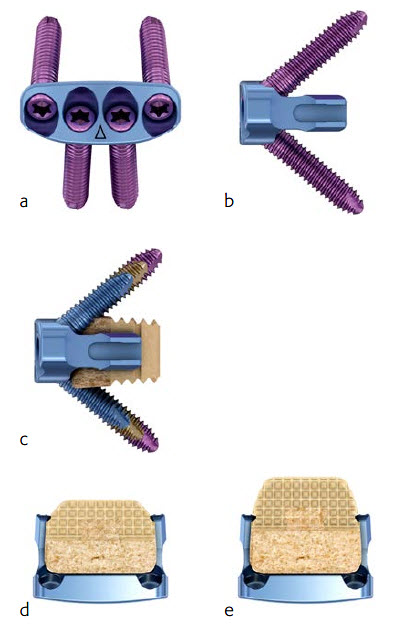
- One-step locking head screws (Fig 4a-c) that form a bone wedge with a 40 5 cranial/caudal angle and 2.5 medial/lateral angle
- Self-tapping screws improve thread purchase
- Self-centering trilobular thread-cutting flutes
- Lengths 12, 14, 16 mm
- The zero-profile titanium alloy plate provides a secure rigid locking screw interface
- The plate accepts different footprints and profiles of the CC Natural allograft spacer (Fig 4d-e)
The CC Natural allograft spacer (Fig 5)
- Eases surgical technique by eliminating the need to shape the allograft spacer or to harvest bone from the patient
- Corticocancellous construction offers fusion potential with structural support
- Pyramidal teeth on superior and inferior surfaces create resistance to expulsive forces
- Demineralized surfaces are intended to expose proteins inherent to bone growth and necessary for fusion of the allograft with the adjacent vertebral bodies [3]
- Size and shape options to suit patient anatomy and surgeons ACDF technique preferences:
Standard and large footprint
Lordotic (7 angle) and parallel sagittal profiles
Heights 612 mm, 1 mm increments
Reference
3. Dunn M. Evaluation of osteoinductivity of surface-demineralized cortical allograft in the athymic mouse intra-muscular model. Musculoskeletal Transplant Foundation. 2003 Nov.
Cases provided by Richard Bransford, Seattle, USA
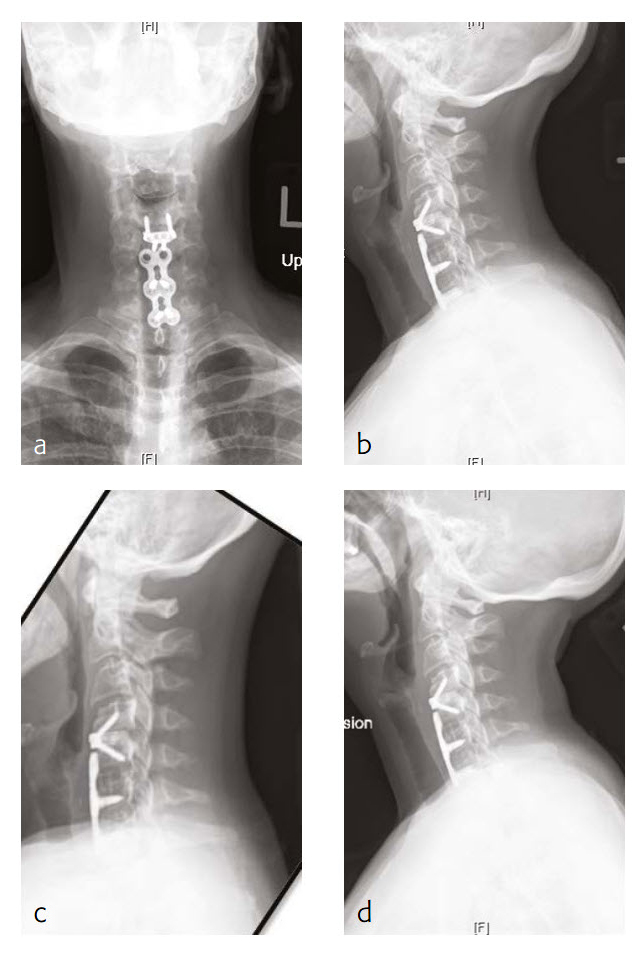
Case 1: Progressive shoulder and arm weakness with neck pain
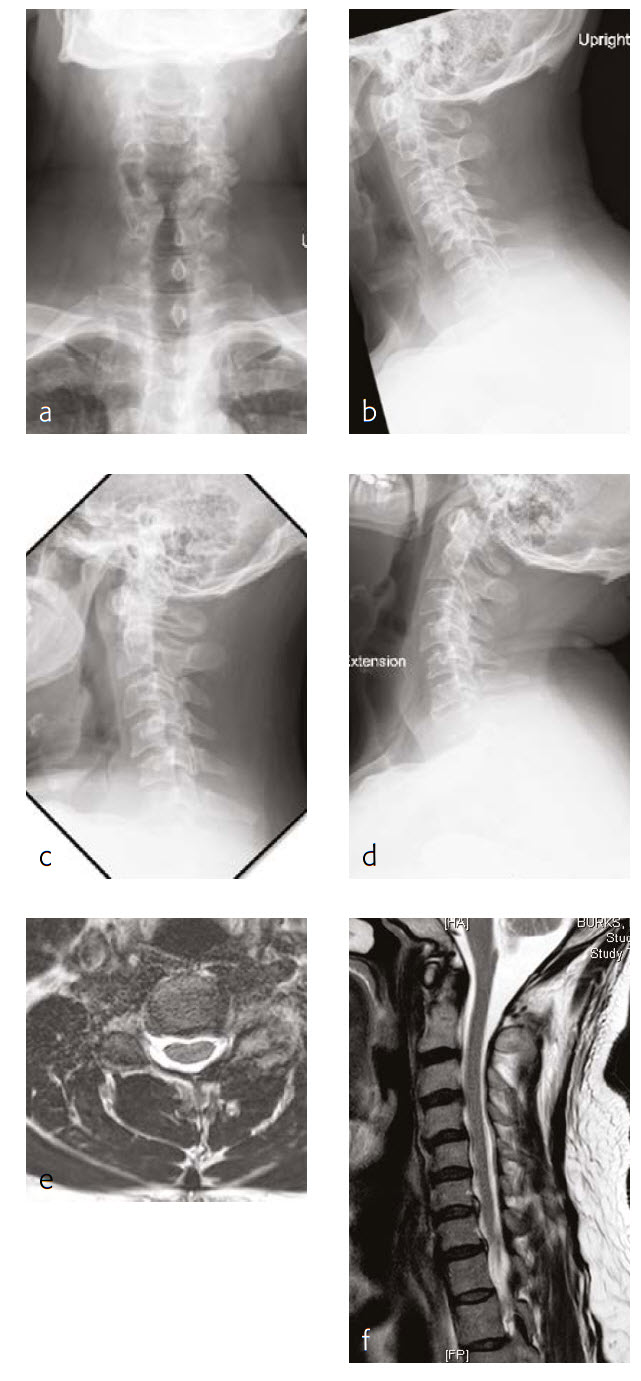
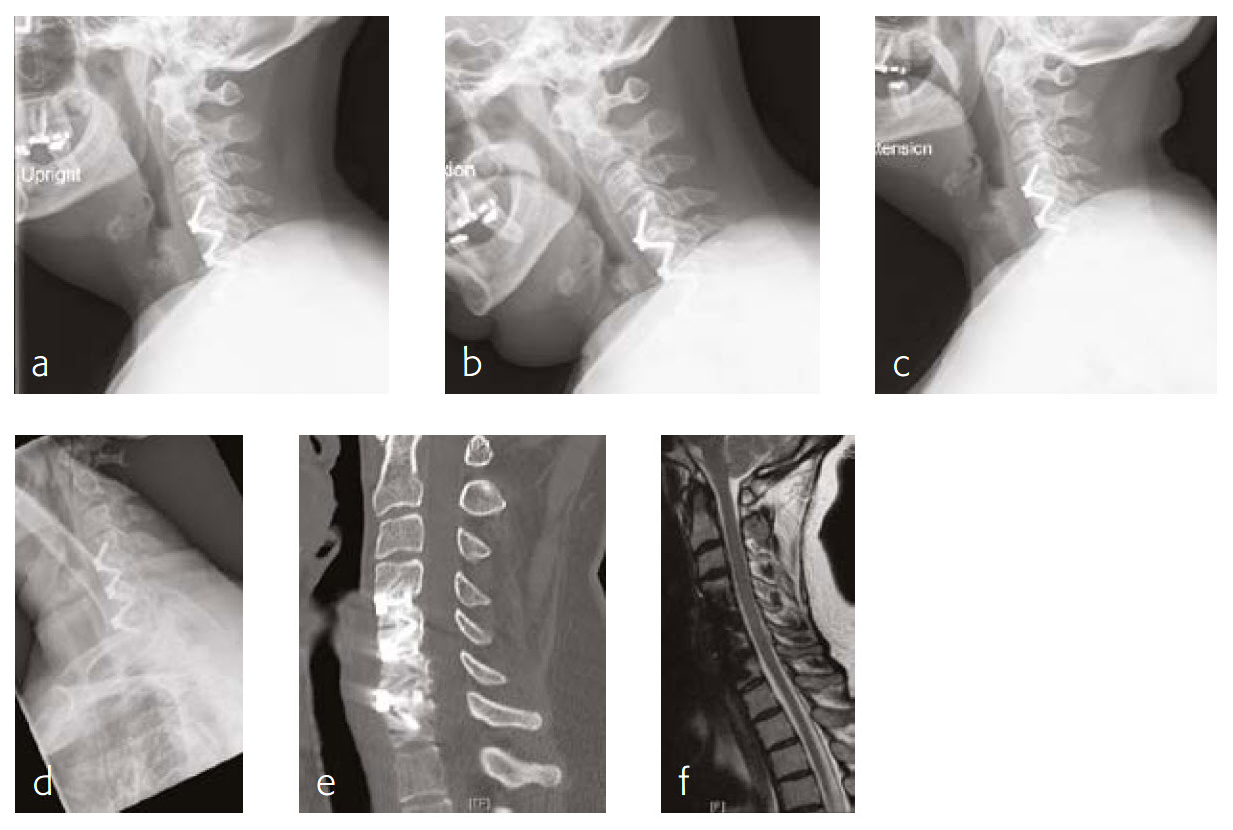
A 56-year-old man, partly left-hand dominant partly right-hand dominant depending on the activity, presented with progressive left shoulder and arm weakness with pain radiating from his neck down to his left shoulder and an EMG documenting a left C5 radiculopathy (Fig 1).
The patient claimed a normal state of health until 5 weeks previous. This then began to backtrack to the neck and to develop weakness in his left arm to the biceps and deltoid. On examination, the patient had 4/5 deltoid and biceps strength on the left and decreased sensation along his lateral shoulder.
The patient showed normal lordosis in his extension x-rays. He has approximately 2 mm of anterolisthesis of C4 on C5 in his extension on his flexion x-ray. This increases to approximately 56 mm and persists in his normal upright film with again some component of spondylolisthesis at that level.
The patient's earlier MRI shows severe left-sided C4-C5 foraminal stenosis and multilevel disc degeneration with very mild central narrowing at C3-C4, C6- C7, and C7-T1. He also has a small right paracentral disc herniation at C6-C7.
The new MRI of the C4-C5 showed mild uncovering of the disc posteriorly due to grade 1 anterolisthesis. There is also mild left facet arthropathy with left uncovertebral joint osteophytes resulting in moderate left neural foraminal narrowing. The right neural foramen is adequately patent.
Follow-up (4 months)
At the patient follow-up at 4 months postoperative, he described complete resolution of left upper extremity pain (Fig 2). He was also happy with his left upper extremity strength and was extremely pleased with his progress. He continued to have no left upper extremity pain. He also believed that he had made significant progress in terms of his left upper extremity range-of-motion and strength.
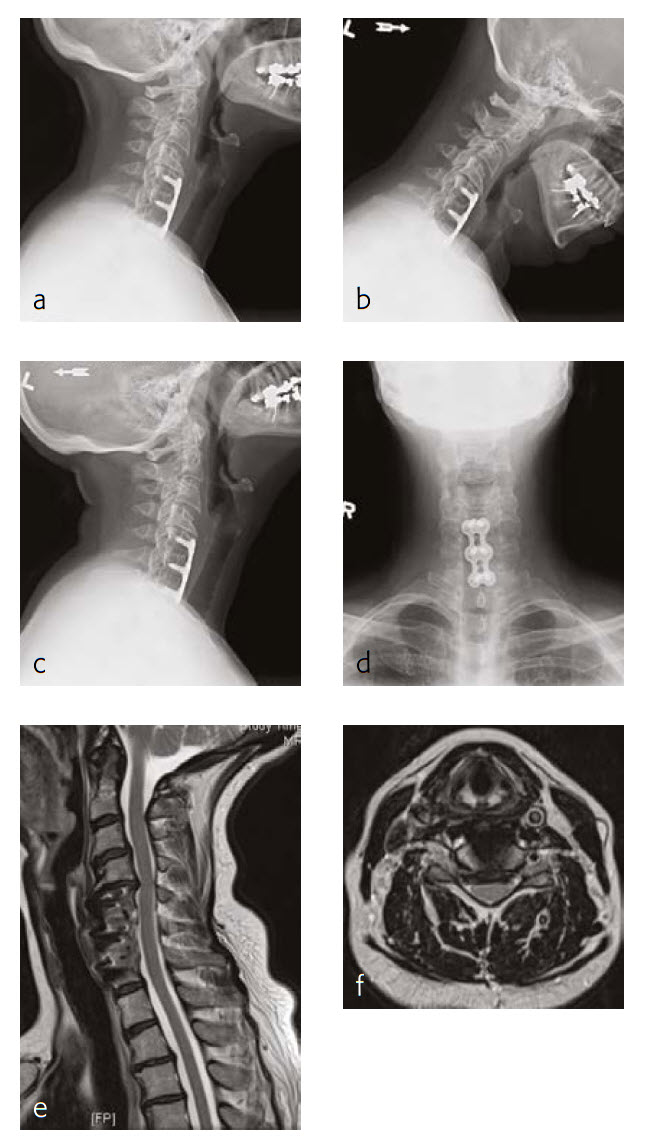
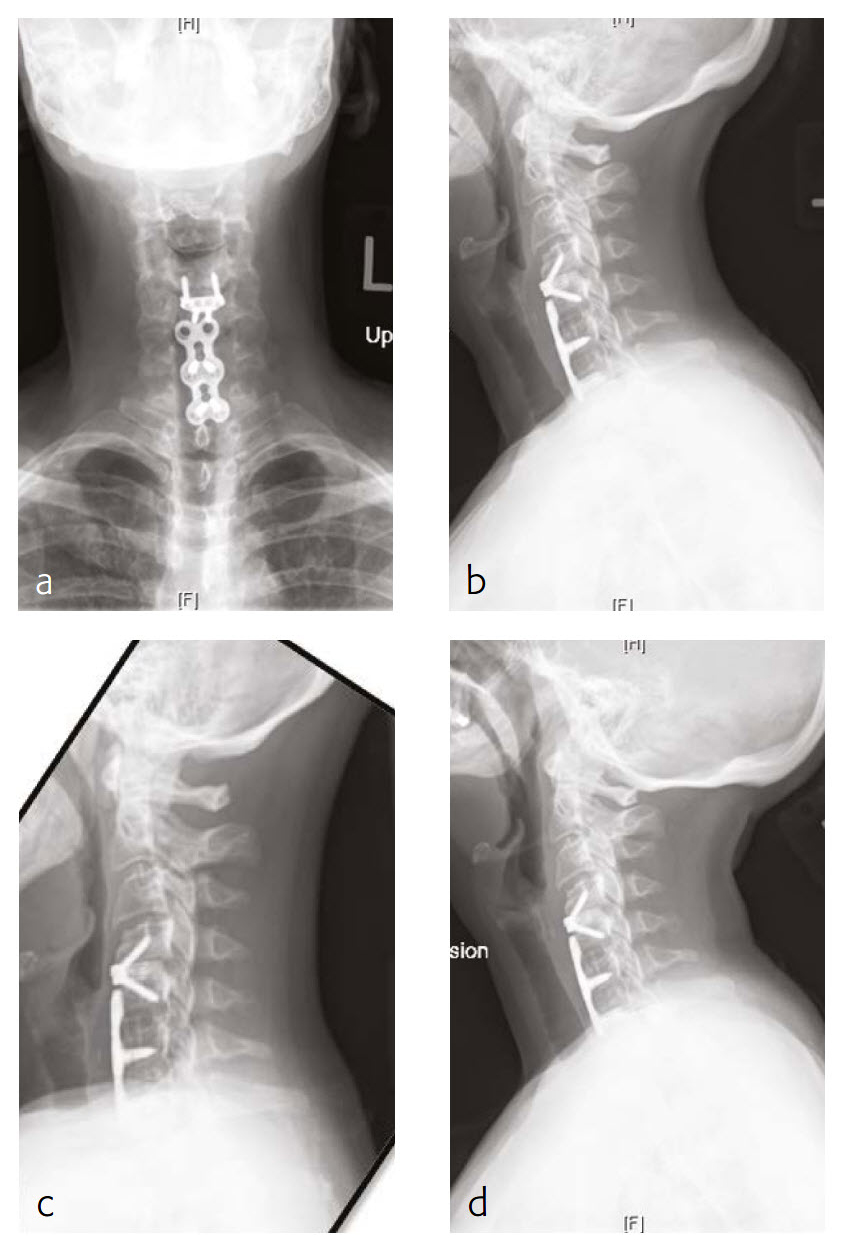
Case 2: Neck pain with cervicogenic headaches
The patient works at a grocery store as a produce stocker and has a history of C5 through C7 ACDF done in 2005 (Fig 3). Her symptoms were relieved at that time, but she had quite severe neck pain and bilateral radicular symptoms. She had chronic C6 radiculopathy since recovery from that procedure, however, was able to return to work. Unfortunately, over the last 34 months, she has had a recurrence of symptoms, with constant neck pain and occasional cervicogenic headaches.
She will occasionally get bilateral pain, a pins and needles-type sensation through a number of distributions, including C5 through her shoulders, less occasionally through a C7 or C6 distribution. Movement of her neck was becoming increasingly painful, particularly with flexion and lateral flexion to the right and left.
She has tried a number of conservative modalities including narcotic pain medications, rest, heat, ice, physical therapy-type exercises, activity avoidance, and oral steroids. She states that she has had a steroid injection. These were not helpful for her. Eventually, she got an MRI and was found to have adjacent level disease.
On manual muscle testing, the patient had 5/5 strength bilaterally with shoulder abduction, elbow extension and flexion, wrist extension and flexion, finger abduction and grip strength.
The patient has appropriate range of motion through her cervical spine with flexion and extension, and lateral flexion and rotation. She gets grimacing pain with extreme ends of flexion as well as bilateral rotation and lateral flexion. She has no tenderness to palpation of the spinous process or paraspinous musculature of her cervical spine. She has decreased sensation in bilateral C5 distributions.
Follow-up (6 months)
The patient is now about 6 months status post a C4-C5 discectomy and interbody fusion with removal of preexisting C5 screws (Fig 4). She was recovering well and has not been taking any narcotic pain medication. She takes acetaminophen.
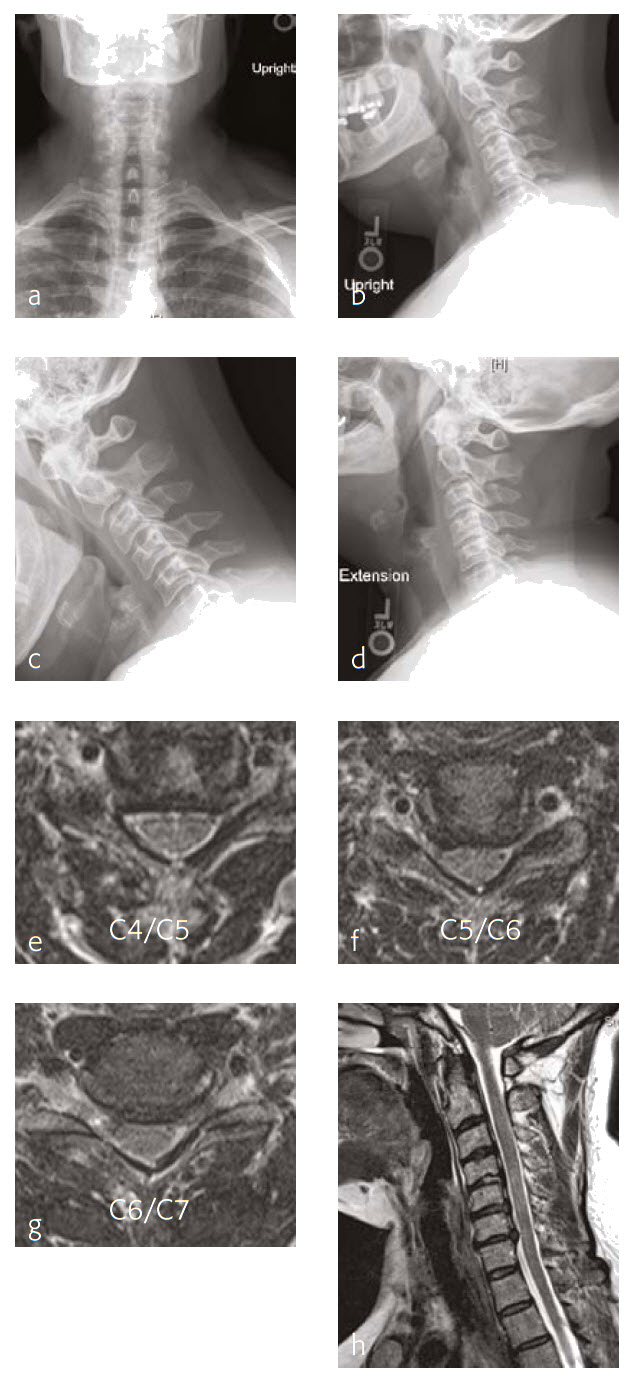
Case 3: A 46-year-old woman with neck pain and upper extremity paresthesia
A 46-year-old woman presented with one-year history of neck pain, upper extremity paresthesia, weakness, and subjective numbness (Fig 5). Her right upper extremity was worse than her left, with loss of function and debilitating pain. She described cramping in her upper extremities without etiology and without alleviating factors.
She had not been responsive to anti-inflammatory medications nor other nonoperative treatment including physical therapy. She had trouble with many of her activities of daily living due to breaks that must be taken due to her pain, as well as the inability to do certain things like open jars due to weakness.
Musculoskeletally, she had no obvious deformity in any of her extremities. Her bilateral upper extremities had strength testing of 5/5 in shoulder abduction, elbow flexion/extension, wrist extension/flexion, and finger abduction/flexion. Bilateral lower extremities showed 5/5 strength with hip flexion bilaterally, as well as bilateral 5/5 strength knee extension, dorsiflexion, plantar flexion of the ankle, and firing EHL.
She had sensation that is intact in all dermatomes. She had no pathological reflexes and no clonus. There was normal tandem gait.
Review of the patients outside imaging showed congenital stenosis of the cervical spine, as well as multilevel disk disease and concomitant acquired stenosis in the foramen of C4-C5, C5-C6, and C6-C7 where it was at its most significant level.
Follow-up (4 months)
At the 4-month follow-up, the patients symptoms were largely resolved and she has been able to return to work (Fig 6). She was very satisfied with her outcome. made significant progress in terms of his left upper extremity range-of-motion and strength.
Zero-P Natural Plate
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.