PHILOS Augmented
Michael Blauth, Denise Eygendaal, Alberto Fernandez dell’Oca, René Haag, Harry Hoyen, Martin Jaeger, Reto Jost, Corinne König, Franz Kralinger, Stefaan Nijs, Norbert Südkamp
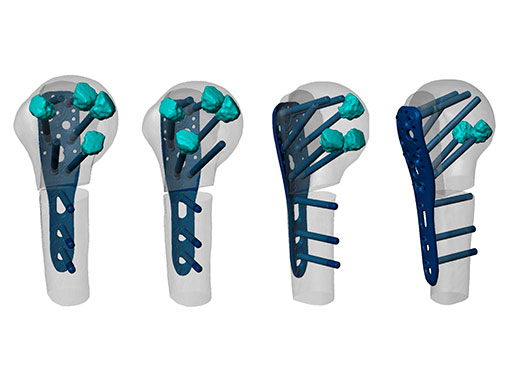
Fixation failure and secondary screw perforation account for a large proportion of the complications of proximal humeral fracture osteosynthesis. It is particularly frequent in elderly patients with osteoporosis [1, 2]. PHILOS (Proximal Humeral Internal Locking System) Augmentation addresses these complications by augmenting the PHILOS plate and screw fixation with Traumacem V+, a high-viscous PMMA cement (Fig 1). A small amount of Traumacem V+ (0.5 ml) is injected through a perforated locking screw, building a cloud around the tip of each screw (Fig 2). Four to six proximal screws are augmented to ensure good anchorage of the osteosynthesis in the humeral head.
Biomechanical principles
The Traumacem V+ clouds increase the surface area around the screw tips and interdigitate with the trabecular structure (Fig 3). This results in a more homogeneous distribution of the stresses at the interface between bone and screw, which enables the transmission of higher loads from the head fragment to the plate. Biomechanical studies confirm that the PHILOS Augmentation offers improved anchorage in low-density bone when compared with standard PHILOS fixation [3, 4] (Fig 4).
Features and benefits
The PHILOS Augmentation system offers a new and unique option to improve the fixation of osteoporotic proximal humeral fractures. It enhances the anchorage in low-density bone, as demonstrated in biomechanical studies. The add-on system allows intraoperative decision making regarding the use of the augmentation option. It enables the surgeon to follow his/her routine reduction and fixation procedure.
PHILOS Augmentation has been in clinical use since January 2013. The very positive user feedback and its biomechanical performance make PHILOS Augmentation a promising treatment option for patients with an osteoporotic proximal humeral fracture.
References
1 Brunner F, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009 Mar; 23(3):163172.
2 Krappinger D, Bizzotto N, Riedmann S, et al. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011 Nov; 42(11):12831288.
3 Unger S, Erhart S, Kralinger F, et al. The effect of in situ augmentation on implant anchorage in proximal humeral head fractures. Injury. 2012 Oct; 43(10):17591763.
4 Kathrein S, Kralinger F, Blauth M, et al. Biomechanical comparison of an angular stable plate with augmented and non-augmented screws in a newly developed shoulder test bench. Clin Biomech. 2013 Mar; 28(3):273277.
NEWS FROM ARI
PHILOS Augmented which screws to augment and how? A numerical analysis of a complex problem
The treatment of fragility fractures remains a major challenge in trauma surgery, particularly at the proximal humerus. Factors such as highly compromised bone mass, complex loading conditions, multifragmental fractures, absent bony support, and limited surgical access to the region make the proximal humeral fixation problem a complex one. Currently, the implant design process is driven by individual opinions and philosophies of medical and technical experts. We hypothesize that this approach will reach its limitations, particularly in the face of complex fracture situations. Rethinking of the design process in terms of employing new tools and procedures for evidence based development will gain importance in the near future.
Computer model to analyze cement augmentation patterns
A first generation computer model has been developed at the AO Research Institute (ARI) in collaboration with AOTK, AOTrauma, and DepuySynthes, to systematically investigate the influence of specific cement augmentation patterns when using the PHILOS plate in combination with bone cement (Fig 1) on the biomechanical competence of the repair construct. The finite elements model employs high resolution quantitative CT image-data of a representative osteoporotic proximal humerus. Each element of the model was assigned with the specific mechanical properties of the corresponding CT gray-values. An unstable 3-part fracture (11-B3) was created by virtually cutting the bone. The fracture was stabilized with a PHILOS plate and screws (6 proximal, 3 distal). Additionally, 0.5 ml bone cement clouds were virtually placed around the tips of the proximal screws. Overall construct stiffness was validated by mechanical testing.
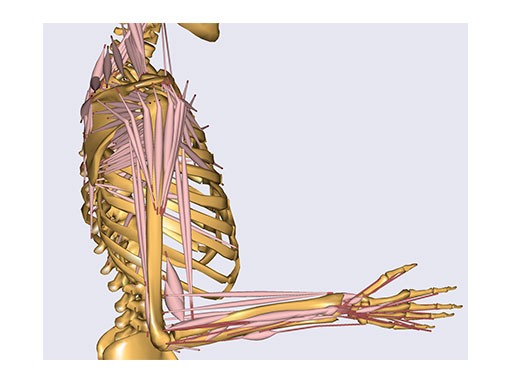
Physiological loading was mimicked by simulated rotator-cuff tendon forces and joint reactions from inverse dynamic calculations (using the AnyBody technology) (Fig 2).
The activity of lifting and placing a cup on the table was simulated, and the corresponding forces were applied to the model. Custom-made software algorithms were used to interlink several software packages from pre to postprocessing to enable efficient simulation of the, in total, 64 combinations of augmented and nonaugmented screws from fully augmented (all 6 proximal screws) to the cementless configuration. Stress/ strain progressions within the bone structure along the screw axes were evaluated. As a general measure for construct performance, strain data around all proximal screws were averaged for each simulation.
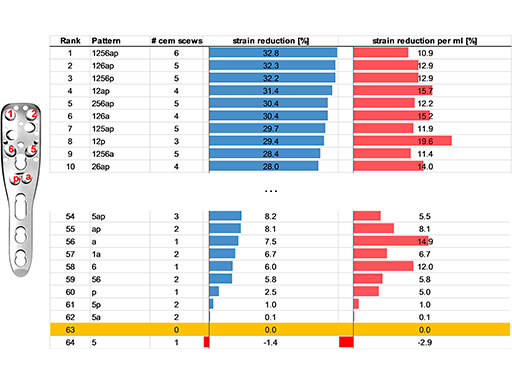
Confirming common sense, a general tendency was observed that bone deformation (strain) decreased with an increased number of augmented Matthias Forte, Ladina Hofmann-Fliri, Claudia Munch, Norbert Sudkamp, Daniel Widmer, Markus Windolf News from ARI Fig 1 PHILOS repair constructs with various cement augmentation patterns. Fig 2 AnyBody model to calculate muscle forces and joint reactions. News from the AO Inst itutes 61 screws. Here, with all six proximal screws augmented, a maximum strain reduction of 33% was achieved compared with the nonaugmented case. However, there were augmentation patterns with fewer augmented screws that yielded a comparable strain reduction. For example, with the most favorable 3-screw pattern (total cement volume 1.5 ml), 29% reduced strain was found (pattern 12p, Fig 3).
On the other hand, the least favorable 3-screw pattern offers a strain reduction of only 8% (pattern 5ap, Fig 3). According to the model, the 4-screw patterns offer strain reductions between 31% and 15% and the 5-screw patterns between 32% and 25%. The fewer screws augmented, the more the actual location of the screws appeared to matter.
It cannot be answered here if these results reflect the performance of an individual case, with specific loading, specific fracture, and individual bone mass distribution, or if they already apply to a population of patients. Enhancement of the model is ongoing by integrating statistical bone models and clinically more relevant fracture patterns. It has to be evaluated in a next step as to what extent these models can support clinical practice by reducing mechanical complications. A future potential is, however, undisputable.
Case 1: Fracture dislocation of the proximal humerus
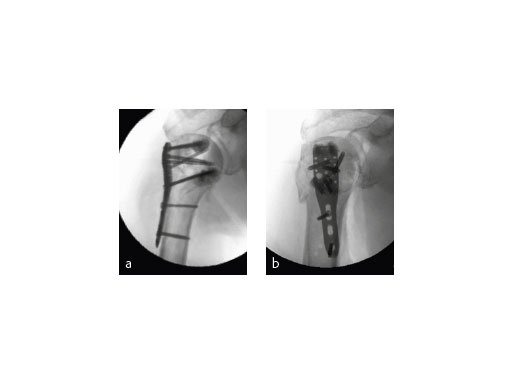
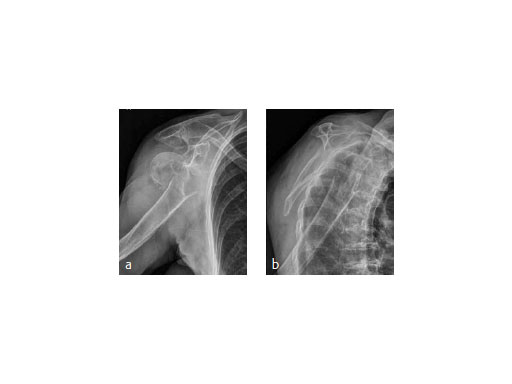
An 82-year-old male patient presented with a fracture dislocation of his right proximal humerus after a fall at home. Examinations revealed a highly unstable valgus-displaced 4-part fracture of the proximal humerus with a disruption of the medial hinge. No neurological injuries were evident (Fig 5).
The patient was placed in supine position, having the shoulder on two shoulder supports. After closed reduction of the shoulder, ORIF was performed via an anterior deltopectoral approach using the PHILOS. Four screws were augmented with Traumacem V+ under fluoroscopic control. Initially the treated shoulder was immobilized in a sling for 2 days followed by a pain-adapted functional treatment (Fig 6).
The X-ray review at 3 months after surgery showed an anatomic reduction of the fracture, nicely formatted augmentation, no secondary loss of reduction, and range of motion of the arm reaching the horizontal plane (Fig 7).
Surgeon's comment
ORIF of proximal humeral fractures using an augmentation technique in addition to the PHILOS seems to be a promising concept. Varus-displaced fractures in osteopenic bone situations of the elderly seem to particularly profit from this technique. Up till now we have had no intraarticular misplacement of the cement and no secondary loss of reduction in these challenging fracture types.
(Case 1 provided by Martin Jaeger, Freiburg, Germany)
Case 2: 91-year-old with osteoporosis
A 91-year-old female patient with osteoporosis had a dislocated 3-part proximalhumeral fracture in her right dominant arm (Fig 8).
The fracture was treated with PHILOS augmentation and healed in anatomical position (Fig 9).
(Case 2 provided by Franz Kralinger, Innsbruck, Austria)
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.