Expert Asian Femoral Nail (A2FN)
The small statured/Asian anatomy was carefully assessed via CT scans and MRI data in terms of morphology and size, to assess the fit of nails to the intramedullary canal of the small stature/Asian patient. It was discovered that current femoral nails do not offer an optimal fit for small stature/Asian anatomy. Generally, the medial lateral bend of current nails is disproportionate, the proximal design of the nails is too long and challenges the surgeon to deliver locking or recon screws into the femoral head without having too much proximal protrusion of the nail itself. The lateral aspects of the nail may cause impingement on the lateral cortex of the small stature/Asian patient.
The A2FN has accommodated all these different aspects. In the proximal region of the nail, the relationship between the locking elements and the proximal nail end has been decreased to negate protrusion in the small stature/Asian patient. Optimum positioning of the recon screws has been accounted for and the length of the proximal end of the nail has been decreased to negate protrusion in the shorter patients. The entry point is at the greater trochanter (5) as this approach is preferred in Asia. The locking options are identical to the AFN except for an additional anteromedial (25) locking hole for more axial stability. The end cap has a longer unthreaded part for easier insertion. A special guide wire with hook engages with the end cap to facilitate a secured way through soft tissue. The nail comes in diameters of 914 mm and in lengths of 280460 mm. The nail is cannulated and available in a left and right version.
Dynamic 4-point bending test of Expert A2FN and AFN according to ASTM showed that the stress curve of the Expert A2FN is about 5% superior to that of the AFN. Dynamic strength of the Expert A2FN is about 30% above that of the AFN.
Case 1: 22-year-old Asian male with multiple injuries after MVA at 160km/hthe car finally stopped in a front yard
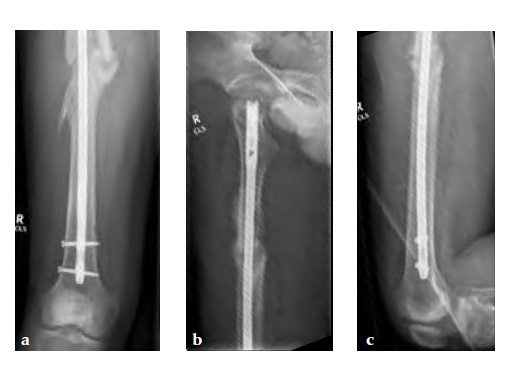
Besides severe upper limb injuries, maxillofacial injuries, a lateral compression pelvic ring injury, and pulmonary contusions, the patient sustained a 32-C3 femur fracture right.
Case provided by Michael Schtz, Brisbane, Australia
After initial stabilization with an external fixator, the femur was nailed in a closed fashion stabilized with an AFN2 in static mode. The accurate length of the injured femur was contemplated from the uninjured leg.
9-month follow-up demonstrates that that the fracture is uniting.
Case 2: A 76-year-old female underwent right total knee replacement 5 years ago and left total knee replacement 4.5 years ago
The patient underwent left L5S1 minimally invasive TLIF with pedicle screws 2 years ago for left lumbar 5th radiculopathy. At the same time she was put on fosamax for osteoporosis.
Case provided by Merng Koon Wong, Singapore, Singapore
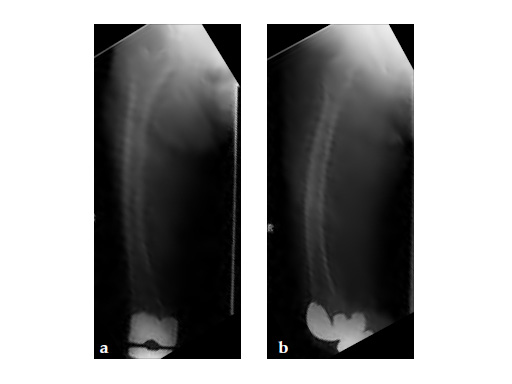
Three weeks prior to her last admission, she complains of recurrent right thigh pain for which epidural analgesics were administered for presumed radiculopathy, however preliminary x-rays and even MRI of the thigh were also taken in view of her primary complaint regarding her right thigh. These investigations did not indicate the possibility of impending bisphosphonate related femur fracture. It is clear from the radiographs that she has an obvious anterolateral bow of her femur and a thickened lateral cortex in the lateral midshaft cortical bone, which may indicate a stress fracture (see Fig 3a-b).
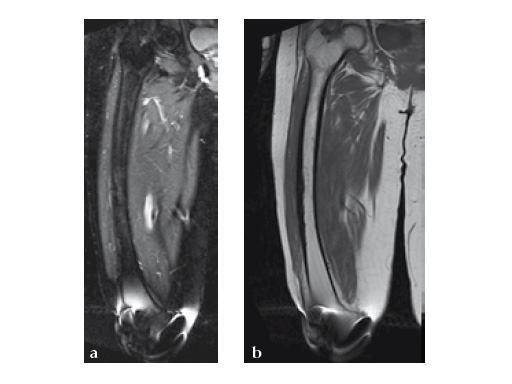
No edema indicated a stress fracture (see Fig 4a-b).
Based on the negative MRI thigh and positive MRI lumbar spine of multiple levels of spinal stenosis, the patient underwent epidural analgesic injection. Patient sustained right femur midshaft periprosthetic fracture the next day after her epidural injection with no trauma.
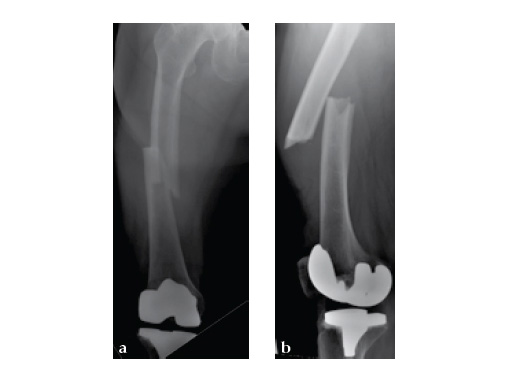
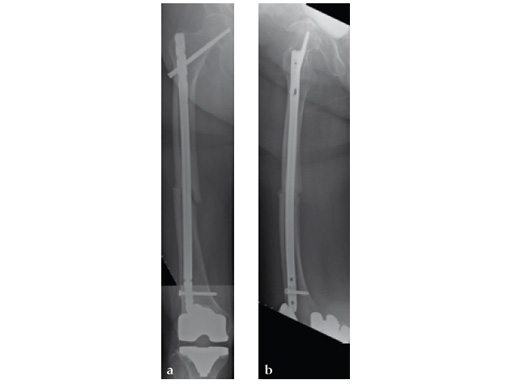
Notice the fracture decrease the emphasis on the anterolateral bow of the femur (See Fig 5a-b).
Insertion of A2FN as patient may be suffering from a stress fracture related to long term (2.5 years) bisphosphonate use. My rationale against a plate is because bisphosphonate related fractures will heal extremely slowly. In our experience even despite bone grafting union may need up to 2 years. In that time, a plate will fail in less than a year even if the patient is only allowed very minimal weight bearing.
Note despite the increased in curvature compared to other nails in the market, there is still noticeable malreduction at the fracture site (see Fig 6a-b).
Patient was allowed and achieved immediate weight bearing and in 6 weeks callus is seen at the fracture site (see Fig 7a-b).
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.