Angular Stable Locking of Intramedullary Nails (ASLS) A new system
The system is compatible with all existing intramedullary nails thereby removing the need for additional implant investment. The system is designed to accommodate intra-operative decision making with regard to deciphering the clinical need for increased stability in specific cases.
Intramedullary nailing of the tibia, femur, and humerus is a long-standing traditional approach to surgical fracture treatment. An important advance in intramedullary nailing was the so-called locking technique.
In intramedullary nailing the fracture fragments of the long bones are threaded onto a tubular or solid intramedullary nail and secured. Additional stabilization of the large fragments is generally achieved by transverse insertion of locking screws. This technique neutralizes rotational and tilting movements. Due to this development almost all fractures in the mid-4/5ths of the long bones could and can be treated by insertion of a locked intramedullary nail.
Previous locking techniques meant that there was always a certain amount of free toggling between the screw and the nail.
Experimental studies [1, 2] have shown that blocked locking would, in principle, be advantageous. In fact, in the area of plating systems, this has already been achieved in the form of so-called angular stable plates.
Why?
The question of why this development was needed is quickly answered: The existing technical solution was not entirely adequate. Residual looseness was disadvantageous to fracture healing and stability and imperfect in terms of patient symptoms, especially in osteoporotic bones weakened by age. The correct technical approach is angular stable locking.
The Solution
The dowels are made of 70:30 poly(L-lactide-co-D,L-Lactide). No critical reaction has been reported so far. Resorbtion of the sleeve may lead to an intrinsic dynamization. Resorbtion starts not before 12 weeks but it depends on the individual. The bioresorbable material makes the system forgiving should any debris have been generated by extra manipulations in the primary operation or the removal. The first removals of the nails caused no problems.
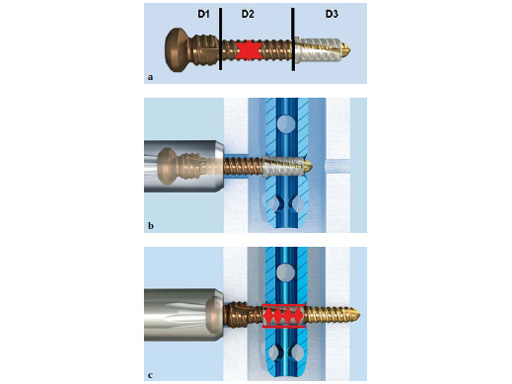
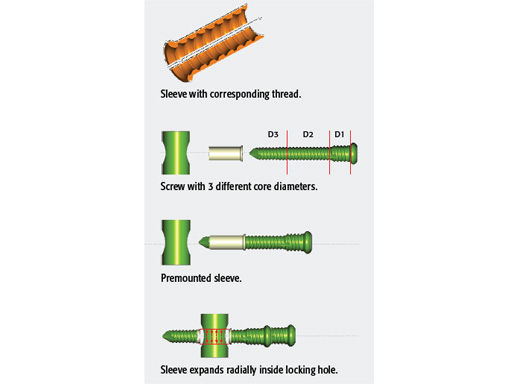
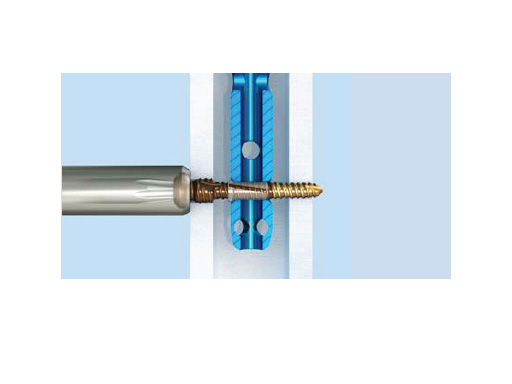
An appropriate hole is made in both bone walls for insertion of the transverse locking screw. The former looseness is eliminated by a dowel system. To insert these dowels, the hole on the side of the surgeon has to be enlarged slightly. The screw has been designed so that it expands the dowel in the nail hole, leading to angular stable locking. The larger thread just beneath the screw head fits tightly into the threaded nail hole (see Fig 2).
ASLS is tolerant with non-exact drilling. Intraoperative change of screws is easy.
We predict:
- Less pain during the healing phase
- Earlier functional loading
- Less initial and delayed displacements of the bone fragments from their ideal positions (maintaining the achieved reduction, preventing secondary malalignment)
With respect to all previous criteria the new locking system will make it possible to rehabilitate patients faster, to restore function sooner, and to lessen and shorten the duration of pain even in nonunions. ASLS is especially advantageous for very proximal fractures which have a higher risk of secondary dislocation, and distal fractures, also in osteoporotic bone. Overall, ASLS is also expected to expand nailing indications.
Final recommendation
Before doing the first case, look very precisely at the operation technique. The system with drills, screws, and sleeves is very easy to understand. The learning curve is very short, if you accept the special additional 2 or 3 steps. In this case the time for the ASLS locking is not significantly longer. A teaching set is available on request.
Bibliography
- Kaspar K, Schell H, Seebeck P, et al (2005) Angle stable locking reduces interfragmentary movements and promotes healing after unreamed nailing. Study of a displaced osteotomy model in sheep tibiae. J Bone Joint Surg Am; 87(9):20282037.
- Epari DR, Kassi JP, Schell H, et al (2007) Timely fracture-healing requires optimization of axial fixation stability. J Bone Joint Surg Am; 89(7):15751585.
First clinical experience with ASLS in patients with tibial, femoral, and humeral fractures
Denise Schmid, AOCID
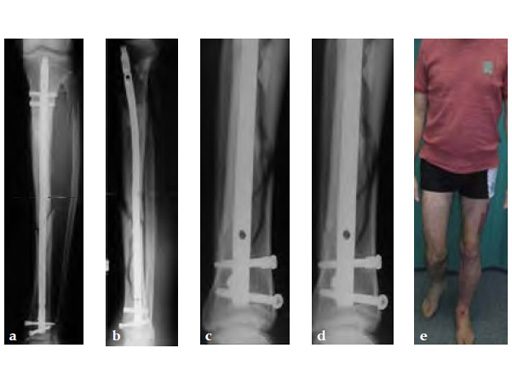
The performance, handling, and technique of ASLS were investigated in a prospective multicenter case series including 31 patients with tibial, femoral, and humeral fractures. Surgeon satisfaction with the handling of ASLS and fracture stability was assessed on a numeric scale ranging from 1 (not satisfied at all) to 5 (extremely satisfied). Radiological assessments were performed at 6 weeks, 12 weeks, and 6 months postoperatively. Time to weight bearing and the occurrence of complications were monitored throughout the 6-month postoperative period.
Of the 31 patients included (cases provided from Berlin, Hannover, Innsbruck, Mainz, and Tbingen), 28 had a tibial fracture (46% open), 2 a femoral, and 1 a humeral fracture. 29 patients were available at each of the 6-week, 12-week, and 6-month follow-up assessments; 2 patients with a tibial fracture dropped out. The follow-up rates were 94% for all examinations. The mean patient age was 45.1 years with the majority of the study population being male (84%).
In 21 cases (68%), the surgeons were very to extremely satisfied with the handling of ASLS. In 30 cases (97%), the surgeons rated the achieved fracture stability as very to extremely satisfactory. Half of the patients with tibial fractures were able to bear full body weight 11 weeks after surgery. Partial and full weight bearing was accompanied by minimum pain.
A follow-up of 94% could be reached. The handling of ASLS is considered simple and satisfactory. Furthermore, surgeons were satisfied with the achieved fracture stability. Only two mild complications were assessed as being related to ASLS. We hypothesize that patients treated with ASLS bear full weight earlier compared to patients with conventional locking. The results and new questions arising from this prestudy led to the planning of a randomized controlled trial, in order to prove the advantages of ASLS with respect to pain progression, weight bearing, gait pattern, and fracture healing compared to conventional locking.
Tips and Tricks Using the ASLS for IM Nails
Angular stable locking of intramedullary (IM) nails has been a goal for many years. The aim is to achieve proximal locking of tibial nails with an end cap blocking the most proximal oblique screw or the spiral blade used with the distal femoral nail (DFN) and proximal humeral nail (PHN).
The increased overall stability of an angular stable locked construct in comparison to a conventional one has been demonstrated in biomechanical studies [13]. Animal studies have shown that bone healing is better and faster [4, 5]. Desired flexible elastic fixation can be achieved by the implant itself similar to angular stable plating compared to uncontrolled toggling. Ultimately, the construct would be an intramedullary internal fixator additional to the external fixator and the extramedullary internal fixator.
Technique
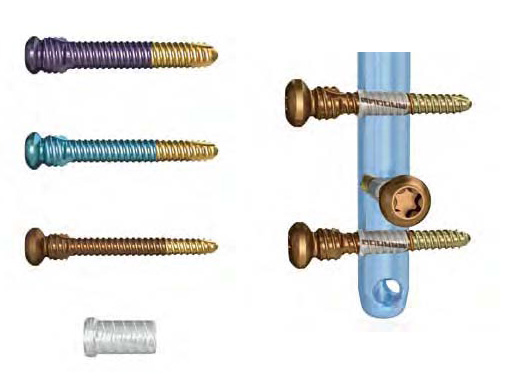
The angular stable locking system (ASLS) consists of a sleeve (function of a dowel) which is added to the locking screws. The sleeves are sterilepacked separate to the locking screws. The surgeon can decide during the operation if the nail should be locked angular stable or conventional. The sleeve is made of a bioresorbable material (70:30 poly L-lactide-co-D,LLactide). The screw is designed to expand the sleeve in the nail hole during insertion, leading to angular stable locking (Fig 1).
From an engineering perspective, the goal to obtain an angular stable locked nailing construct has been achieved. Since 2009, the ASLS has been available in 4, 5, and 6 mm for the different nail diameters and has been successfully used with cannulated nails for the tibia, femur, humerus, and hindfoot. In the hands of experienced surgeons it has led to expanded indications for IM nailing. Provided here are some recommendations on how to use the system based on the experiences during the first two years.
Tips and tricks
As the decision on angular stable or conventional locking can be made intraoperatively, the screws and sleeves should always be available on the tray/shelf and properly sorted (similar to the suture material).
The 6 mm ASLS is only required for the very strong femoral nail (> 13 mm). Depending on the local patient population, it may be sufficient to obtain only the 4 and 5 mm systems to minimize inventory.
In proximal applications only ASLS may be used, or in the following combinations with conventional locking: dual-core locking screws, proximal locking screws blocked by an end cap, or all of them.
ASLS should not be used in the dynamic locking slot as it does not provide enough hold/resistance.
In distal applications, mixing conventional locking screws with ASLS does not make sense.
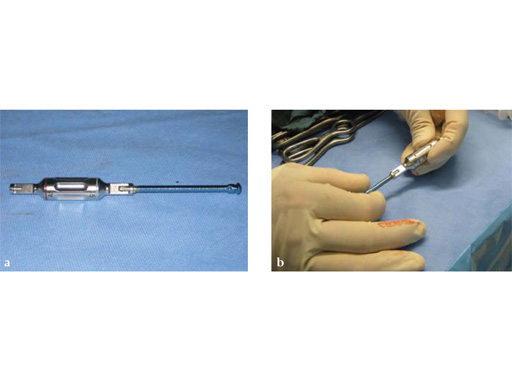
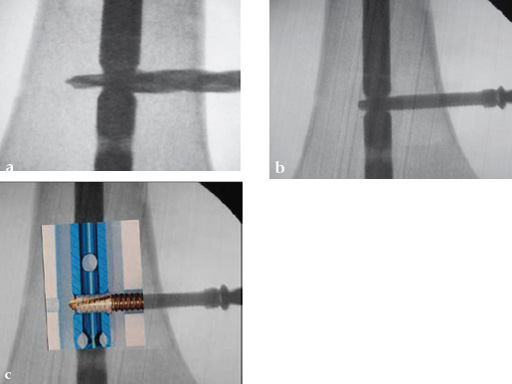
Drilling is identical but the near cortex needs additional reaming so it is wide enough to insert the sleeve. The enlarged hole at the near cortex will be filled by the thicker part which has a larger diameter than the rest of the screw (Fig 2). Use of the hand reamer has proven to be more tactile compared to drilling with machines (Fig 3). Power-driven drilling is only needed for very strong cortices, eg, the femur.
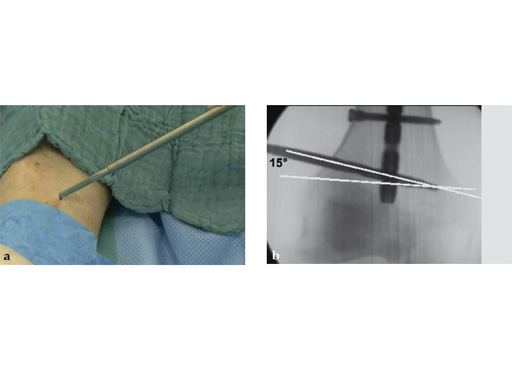
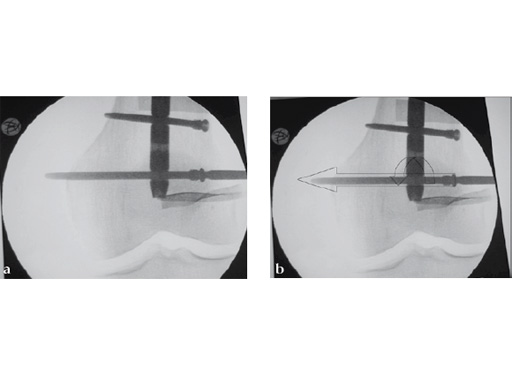
Drilling does not have to be very precise as the ASLS tolerates deviance. An exact amount cannot be given but up to 15 seems to be unproblematic (Fig 4).
To ensure sufficient sized reaming, insert the tip of the reamer until it may touch the hole of the nail. When using the hand reamer, the reamer cannot be damaged.
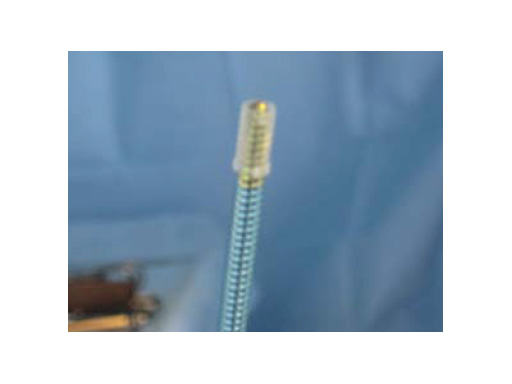
The sleeve is threaded on the screw by hand just before implantation (Fig 5). The lip of the sleeve needs to face the screw head. The sleeve is positioned correctly when the gold part of the screw is visible on either side of the sleeve (Fig 6). If the sleeve is placed too far on the screw, the connecting bars may be damaged or break. In this case a new sleeve has to be used. A sleeve with broken bars will not work. A sleeve positioner is available which prevents overthreading (Fig 7).
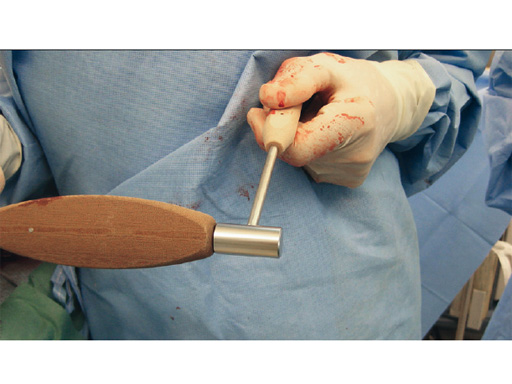
The screw-sleeve construct is pushed into the nail's locking hole by hand. For the final placement, a light hammer (100 gr) may be used (Fig 8). You can actually feel and even hear the correct positioning. Use of a heavier hammer may lead to too deep placement or even pushing the sleeve too far through the locking hole. Control by image intensifier of the reamer and/or screw placement is only needed in the very early part of the learning curve (Fig 9).
The final screw positioning can be felt as the broader screw thread widens the sleeve, filling up the enlarged near cortex.
In thin cortex, regardless of whether proximal or distal, the screw needs to be inserted very carefully, otherwise the tensile forces may pull the screw head beneath the cortex. Image intensifier control may be helpful in cases of thin cortex (Fig 10) or the use of the protection sleeve system to stop the insertion at the correct point (Fig 11). But the sleeve system does not need to be used in every case as it needs a bigger skin incision.
An inserted screw which is either too long or too short can be exchanged without problems. In most cases, the sleeve will remain in the nail and does not need to be exchanged.
The ASLS should only be used with cannulated nails. In solid nails, the compressed sleeve develops heat through the increased pressure. In cannulated nails this does not occur as the material expands into the cannulated inner part of the nail. ASLS is not indicated for use with solid nails but if a solid nail is selected by the surgeon, insertion has to be done very slowly and with short breaks for cooling.
Removal of a nail locked with ASLS is not any different than without. If the sleeve is not yet fully resorbed it will remain in the nail and is removed together with the nail.
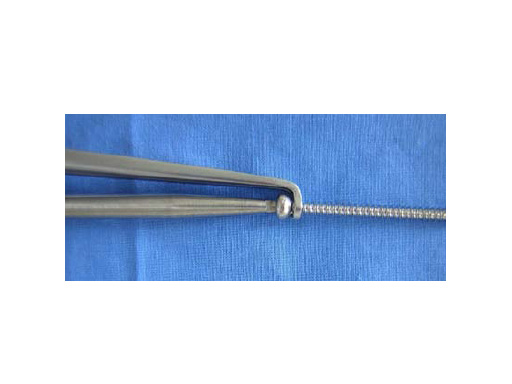
Remember that removal of the locking screws does not remove the sleeve. In case of a resorbed sleeve, the screw may not have enough hold in the sleeve thread to be screwed out. In this case it can be beneficial to use an extraction forceps which closes behind the screw head and allows screwing and pulling at the same time (Fig 12). This extraction forceps is very helpful in similar kinds of screw removals without ASLS.
Overall, the intriguing features of the ASLS are its universal use in all cannulated nails, the almost unchanged standard locking procedure, and its easy and tolerant application. These tips and tricks have demonstrated that only a few additional maneuvers need to be considered.
References
1 Miller DL, Goswami T (2007) A review of locking compression plate biomechanics and their advantages as internal fixators in fracture healing. Clin Biomech; 22(10):10491062.
2 Perren SM (2002) Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surgery; 84(8):10931110.
3 Egol KA, Kubiak EN, Fulkerson E, et al (2004) Biomechanics of locked plates and screws. J Orthop Trauma; 18(8):488493.
4 Kaspar K, Schell H, Seebeck P, et al (2005) Angle stable locking reduces interfragmentary movements and promotes healing after unreamed nailing. Study of a displaced osteotomy model in sheep tibiae. J Bone Joint Surg Am; 87(9):20282037.
5 Epari DR, Kassi JP, Schell H, et al (2007) Timely fracture-healing requires optimization of axial fixation stability. J Bone Joint Surg Am; 89(7):15751585.
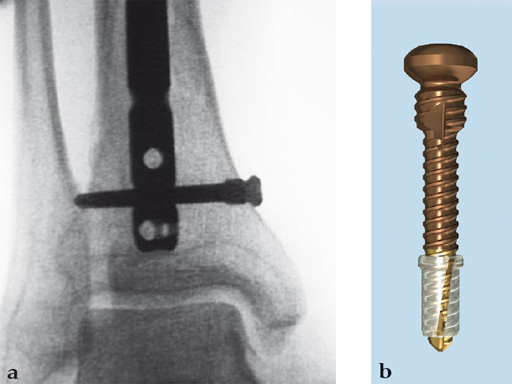
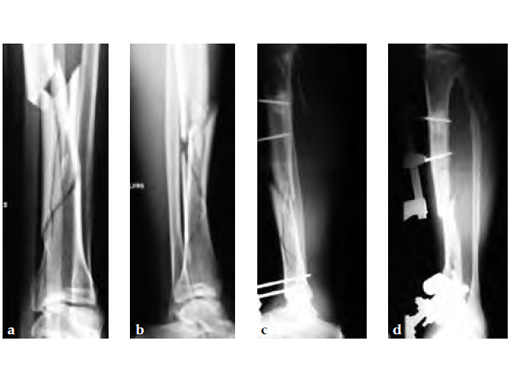
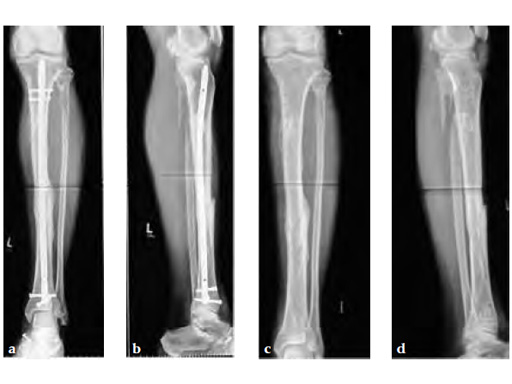
A 58-year-old male sustained a closed multifragmentary 42-C1 fracture in the distal tibia with compartment syndrome.
Case provided by Dankward Hntzsch, Tbingen, Germany
Primary treatment consisted of an external fixator and release of compartments.
Mobilization of the limb started with an applied external fixator.
Secondary treatment: insertion of an unreamed intramedullary nail with three ASLS screws inserted distally providing angular stability.
Partial weight bearing started on postoperative day 2 (with 2030kg). The weight was gradually increased over the following weeks. At 6 weeks, the patient was able to fully bear weight even though a high fibula fracture was present and no callus had yet formed. This suggests that angular stable interlocking of the nail markedly enhances stability. The patient was able to bear weight faster than planned and full weight bearing was possible with little pain.
Twelve-week follow-up shows callus formation, and the patient was able to fully bear weight without any pain.
The nail was removed 15 months postinjury as planned. There is good callus formation and proper healing of the tibia fracture.
Latest advances in IM nailing techniques
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.