TomoFix Medial High Tibia
High-tibial osteotomy is a widely accepted technique in the treatment of varus malalignment and medial osteoarthritis of the knee. Middleand long-term results are good if the indications are respected and an adequate correction is achieved. Corrective osteotomy of the proximal tibia may be performed by a subtractive technique (closed-wedge), by a barrel-vault (dome) osteotomy, or by an additive technique (openwedge). The closed-wedge technique with removal of a bone wedge through a lateral approach and fixation with staples, a plate, or a tension-band system has disadvantages such as risk of peroneal nerve injuries, the need of osteotomy of the fibula, or separation of the proximal tibiofibular joint and of detachment of the extensor muscles. Large corrections cause significant shortening of the leg and an offset of the proximal tibia, which may compromise placement of the tibial component in a total-knee replacement. Open-wedge osteotomy from the medial side can be performed without any muscle detachment, the correction can be fine-tuned during the procedure and no leg shortening occurs. Open-wedge osteotomy has regained interest with the development of stable implants which enable the surgeon to fix the correction and to avoid bone grafts in most cases.
The existing TomoFix medial high tibia (TomoFix MHT) for openwedge osteotomies has been redesigned for better soft-tissue protection and to minimize rotation during compression.
The precontoured plate now has a chamfer at the proximal part and rounded edges at the lateral rims of the plate. A MIPO tapered end at the distal end was added to have a smoother pass to the bone. The two upper LCP holes in the distal part were slightly repositioned in line with the axis of the plate to eliminate the rotation of the plate during compression with cortex screws because of the former asymmetrical alignment of the holes. The two most distal LCP holes were changed to isolated LCP holes to hinder the use of cortex screws.
In a biomechanical comparison, the plates were tested after a right osteotomy. The results show a higher number of cycles with the new TomoFix MHT due to improvements in the manufacturing process. The quality of bone healing with the new TomoFix MHT is similar to the former one but the healing time is expected to be faster and insertion easier. The less prominent design reduces the pain and the higher stiffness activates the use of the compression screw. Handling, use, hospitalizations time, and all other biomechanical characteristics are comparable with the former plate.
The former TomoFix MHT will be replaced with the new version, the article numbers in the catalogue will remain the same.
Osteotomy around the knee has regained interest in the last years. The effect of malalignment on joint overload and osteoarthritis of the knee is well recognized, and the positive effect of correction of malalignment especially in the metaphyseal areas of tibia and femur on pain and function has been proven. The development of the TomoFix implants and the related instruments and techniques has popularized osteotomy in the German-speaking countries. The techniques have now also spread to the Asian world. The authors present an update on tibial osteotomy using the TomoFix implants.
High tibial osteotomy is a widely accepted technique in the treatment of varus malalignment and medial osteoarthritis of the knee since the work of Marquet and Coventry. Middle and long-term results are good if the indications are respected and an adequate correction is achieved. Corrective osteotomy of the proximal tibia may be performed by a subtractive technique (closed wedge), by a barrel-vault (dome) osteotomy or by an additive technique (open wedge). The closed wedge technique with removal of a bone wedge through a lateral approach and fixation with staples, a plate or a tension-band system has, until recently, been the most popular. Disadvantages of this technique are the risk of peroneal nerve injuries, the need for osteotomy of the fibula or separation of the proximal tibiofibular joint, and of detachment of the extensor muscles. Large corrections cause significant shortening of the leg and an offset of the proximal tibia, which may compromise placement of the tibial component of a total knee replacement. Open wedge osteotomy from the medial side can be performed without any muscle detachment, the correction can be fine-tuned during the procedure, and no leg shortening occurs. Whereas this technique was described some time ago, few surgeons used this method, since the harvest of bicortical bone grafts from the pelvic crest to fill the osteotomy caused significant morbidity. However, open wedge osteotomy has regained interest with the development of stable implants which enable the surgeon to fix the correction and to avoid bone grafts in most cases.
Technique
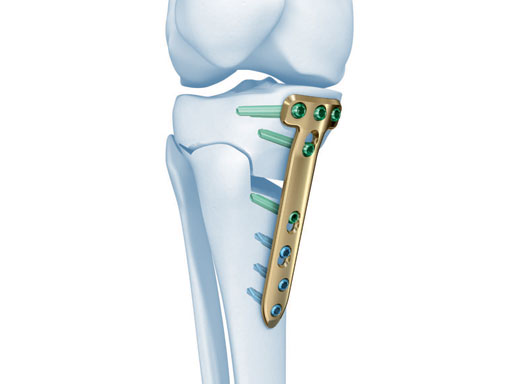
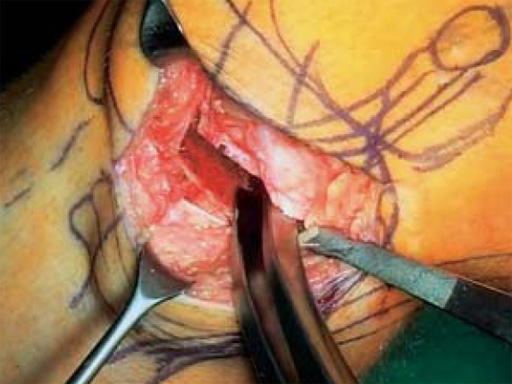
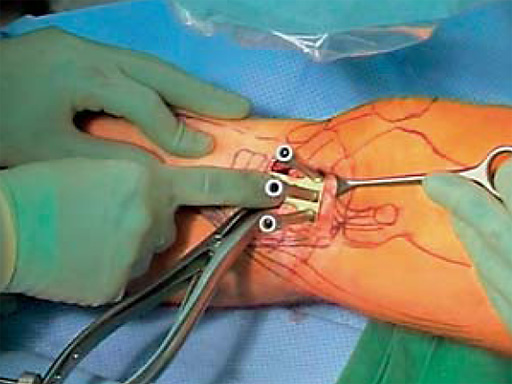
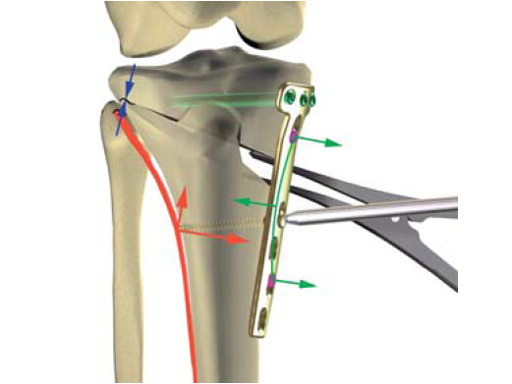
The correction is planned on a long-leg standing x-ray. After surgery, the mechanical axis should pass through a point 63% on the lateral side of the total width of the tibial plateau in the frontal plane. A transverse or slightly oblique incision is used to avoid damage to the saphenous nerve. The distal fibers of the medial collateral ligament are detached from the tibia. Under fluoroscopic control, two wires are placed in the proximal tibia marking the transverse osteotomy plane. The cut usually starts at the upper margin of the pes anserinus and ends at the tip of the fibula on the lateral side. The wires are placed exactly parallel to the tibial plateau thus taking into consideration the individual tibial slope of the patient. An incomplete cut of the posterior two-thirds of the proximal tibia is performed with an oscillating saw guided by the wires. Continuous irrigation avoids burn injury to the bone. A second osteotomy is now performed in the anterior third of the tibia in an angle of 100 ending above the patellar tendon insertion. A smaller saw blade is used and the complete anterior cortex is cut exactly in the frontal plane. The osteotomy is now gradually opened by inserting flat chisels or a spreader-chisel into the posterior osteotomy cleft. This process may take some minutes and can usually be completed without fracture of the lateral cortex. A bone spreader is now placed in the posteromedial edge of the tibia and the chisels are removed. The leg is extended and the correction is checked with the fluoroscope. A long metal rod is placed between center of the hip joint and center of the ankle joint. The projection of this rod should be at the planned point of correction on the tibial plateau lateral of the midline. Eccentric collapse of the medial joint space may cause accidental overcorrection. In this case pressure on the foot may simulate loading and body weight. The correction can be fine-tuned by opening or closing the spreader. The TomoFix Medial Tibia Plate is now placed in a subcutaneous pocket. The implant is precontoured and usually fits well to the bone surface. The distance holders avoid compression of the medial collateral ligament and the pes anserinus. Three proximal bolts are placed near the subchondral sclerosis zone. The position of the bolts is adapted to the anatomy of the proximal tibia giving optimum purchase for the bolts. An oblique lag screw is inserted distal to the osteotomy. This screw in the first combination hole allows careful compression of the lateral osteotomy hinge and pretensioning of the implant. A stab incision is created on the shaft and the implant is fixed monocortically with bolts. The lag screw and the distance holders are replaced by bolts. The medial collateral ligament is released longitudinally to reduce medial compartment pressure and the wound is closed in layers. An overflow drain may be used. Clinical and experimental work has proven that when this technique is closely followed, corrections up to and over 15 mm can be performed without bone grafting or use of bone substitutes.
The patient is mobilized on crutches on day one after surgery. Partial weight bearing is allowed from the beginning. Biomechanical and RSA studies have proven that postoperative loading of the implant by body weight in standard partial weight bearing and early full weightbearing conditions did not cause loss of correction. Our group now allows the patients to walk without crutches as soon as the postoperative pain allows after this type of surgery. Members of the Knee Expert Group (KNEG) have presently implanted over 1,500 TomoFix medial tibia. The results are extremely positive in respect to osteotomy healing, implant failure, and surgical complications.
Perspectives
The KNEG is working on further improvements to the implants. The TomoFix Medial Tibia Shaft will get slimmer, as the combination holes on the shaft will be exchanged against simple locking holes. The edges will be rounded to help avoid morbidity from the implant. These design modifications have been tested biomechanically and no disadvantages have been recognized against the present plate design. In addition, a smaller version of the plate is presently in preparation, mainly adapted to the specific anatomy of the Asian proximal tibia. Development of this plate is strongly supported by the input of our Japanese friends R Takeuchi and T Sawaguchi. First prototypes will undergo biomechanical testing in the near future.
Literature
- Agneskirchner JD, Freiling D, Hurschler C et al (2006) Primary stability of four different implants for opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc; 14(3):291300.
- Gaasbeek R, Sonneveld H, van Heerwaarden RJ et al (2004) Distal tuberosity osteotomy in open wedge high tibial osteotomy can prevent patella infera: a new technique. Knee; 11(6):457461.
- Lobenhoffer P, Agneskirchner JD, Galla M (2006) Kniegelenknahe Osteotomien Indikation, Planung und Operationstechnik mit Plattenfixateuren. Stuttgart New York: Georg Thieme Verlag.
- Lobenhoffer P, De Simoni C, Staubli AE (2002) Open wedge high tibial osteotomy with rigid plate fixation. Tech Knee Surg; 1(2):93105.
- Staubli AE, De Simoni C, Babst R et al (2003) TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia - early results in 92 cases. Injury; 34 Suppl 2:B5562.
Osteotomy Guiding Device
The success of lower-limb osteotomies depends on accurate correction of the mechanical axis and stable fixation during consolidation. Exact realignment of the leg requires precise resection of a bone wedge. The high precision reduces the risk of under- or overcorrection which is what improves the quality of an osteotomy and their durability (knee arthroplasty can be delayed or avoided completely).
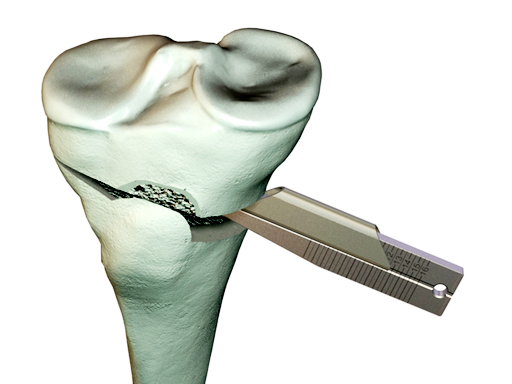
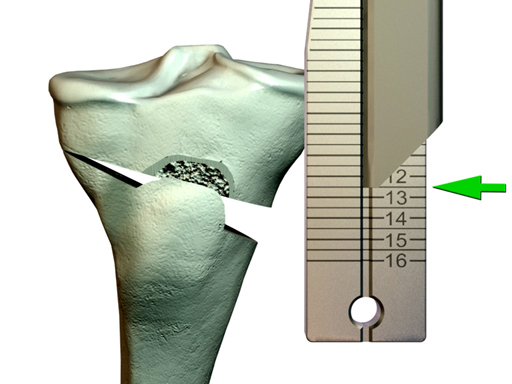
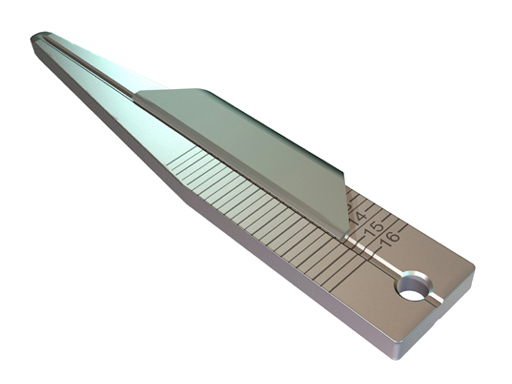
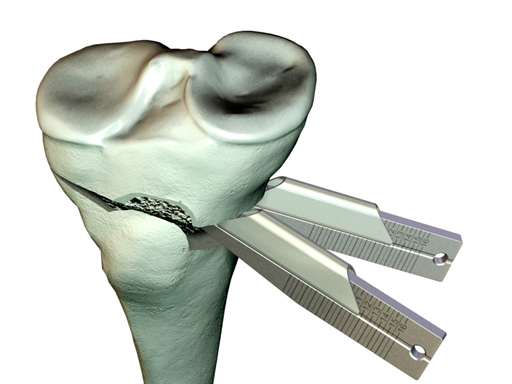
The TomoFix Gap Measuring Device enables simple measuring of the depth of the osteotomy gap and determination of the suitable chronOS block (if used).
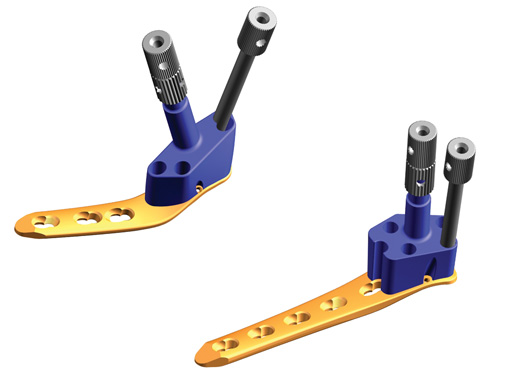
Guiding Blocks
The Guiding Blocks for TOMOFIX are indicated for medial and lateral high tibia osteotomy and lateral distal femur osteotomy. The Guiding Blocks facilitate the placement of the LCP drill sleeves in the head portion of the plates. The Guiding Blocks for the lateral high tibial osteotomy and for the lateral distal femur osteotomy come in a left and right version. The benefits of osteotomy fixation with TOMOFIX plates are early pain-free mobilization of the patient and a minimal risk of secondary loss-of-correction of the osteotomy. Open or closed wedge osteotomy technique is possible with TOMOFIX plates.
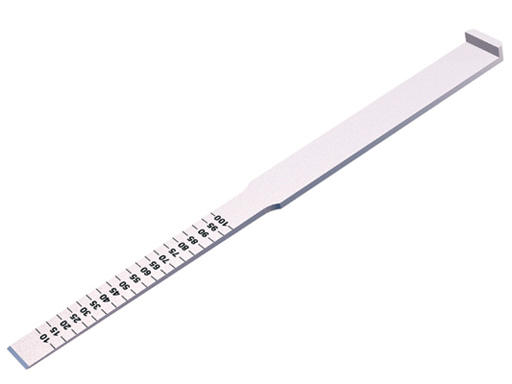
Osteotomy Chisel
Open wedge osteotomy ot the tibia seems to have several advantages over closed wedge osteotomy, including reduced risk of neurologic damage (e.g. peroneal nerve), no shortening of the medial tibial and easier insertion of a future knee arthroplaty if necessary. In addition, the elevation of the proximal tibia can be adjusted more posteriorly or anteriorly according to needs. On the other hand, it is difficult to maintain the open wedge situation with conventional implants.
For the osteotomy, one can use newly developed chisels with rounded edges and measuring scales to determine the depth of penetration. They also come in different widths.
A 68-year-old female.
Case provided by Alex Staubli, Luzern, CH
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.