Distal Humerus Plate (DHP)
Treatment of distal humeral fractures using the standard reconstruction plates has shown to be difficult and may lead to poor results in osteoporotic bone and in very distal fractures, where the LC-DCP or standard reconstruction plates do not provide sufficient stability. The Distal Humerus Plate (DHP) was developed to allow treatment of difficult fractures, allowing fixation of bone very distally, and increasing the number of fixation possibilities which provide high stability of fixation with less risk of loss of reduction and allow early functional mobilization. The DHP is indicated for intraarticular fractures of the distal humerus, supracondylar fractures of the distal humerus, and nonunions of the distal humerus.
The DHP systems consist of dorsolateral plates, with or without support, right and left, with 3, 5, 7, 9, or 14 holes and medial plates, right and left with 3, 5, 7, 9, or 14 holes, to fit all different fracture patterns and fracture extensions.
The DHP is available in stainless steel and titanium. On the medial plate the distal screws are directed from the epicondyle to the trochlea.
On the dorsolateral plate the distal screws are directed to the capitellum. In addition the screws of the lateral support are inserted through the capitellum. The screw is designed for least interference with other screws, the insertion is done through an aiming device which also provides the necessary interfragmental compression if needed. The distal part of a dorsolateral or medial plate has threaded holes which accommodate either locking head screws 2.7 mm (head LCP 2.4) or standard cortex 2.4 mm screws.
The shafts of the plates have LCP combi-holes designed to be used either with 3.5 mm locking head screws or with standard cortex screws 3.5 mm.
The LCP Distal Humerus has been developed for fractures in the metaphyseal area that may reach into the shaft. The distal end is anatomically contoured to the distal humerus, with three isolated round combination holes. This new round hole allows to use 3.5 conventional cortical screws to facilitate optimal screw positioning in the joint block of the distal humerus. The screws in the distal section are angled to allow optimal fixation of the screws without penetrating the joint. The reconstruction cuts in the plate shaft, allowing easy and accurate bending of the plate to adapt to the variance of the diaphyseal anatomy. The LCP Distal Humerus is available in titanium and stainless steel, in five different lengths with 7, 9, 11, 13 and 15 holes.
Angular stability is beneficial for distal humeral fracture fixation in osteoporotic bone.
Objective
Fracture fixation in osteoporotic bone is still a considerable problem in trauma surgery, especially in the metaphyseal areas. Postoperative loss of reduction is observed frequently. Current implant developments for fracture fixation at the distal humerus incorporate the locked screw concept (LCP) as well as the concept of anatomically preshaped plates which allow placement of several screws of smaller diameter within the metaphyseal regions (Distal Humerus PlateDHP).
The purpose of this study was to biomechanically investigate whether these implant concepts are advantageous in the treatment of distal humeral fractures if compared to Conventional Reconstruction Plates (CRP).
Materials/methods
Three groups (CRP n=8, LCP and DHP n=12) of human cadaver humeri were formed with similar distributions of bone mineral density (BMD, obtained by pQCT). In each specimen an unstable low distal humeral fracture (13-C2) was simulated by means of an intraarticular, sagittal saw cut of 0.5 mm thickness and a 5 mm supracondylar osteotomy gap representing metaphyseal comminution. In all groups double plate osteosynthesis was performed in 90 configuration according to standard AO technique.
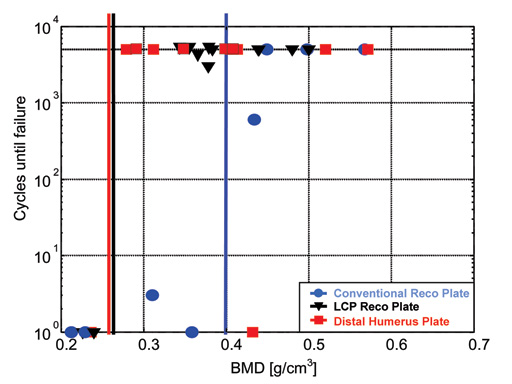
Cyclic loads of 150N were applied in flexion up to 5000 cycles. Physiological conditions of force transmission were used (60% applied to the capitulum, 40% to the trochlea). Relative fragment movements were determined in the frontal and sagittal planes. Criteria for failure were screw pull-out or distal fragment rotation of more than 5 in the sagittal plane.
Results
No differences between the 3 groups were apparent at BMD values above 0.4 g/cm3; all specimens survived the full test duration. DHP and LCP implants (2/12 failures each) showed improved resistance to implant or screw loosening as compared to CRPs (5/8 failures) with decreasing BMD. The improvement was quantified by the borderline of BMD, below which the constructs were likely to fail (failure-limit). This failurelimit was located at higher BMD values for the CRP group (0.4 g/cm3) than for the LCP and DHP groups (0.25 g/cm3).
Conclusion
Anatomically pre-shaped plates with several metaphyseal screws and locked screw concepts improve stable fracture fixation of the distal humerus, especially in osteoporotic bone.
Fig
Implants tested: conventional reconstruction plates, LCP reconstruction plates and distal humerus plates (from left) applied to human distal humerus specimens in 90 configuration.
A specially adapted Guiding Block allows easy and correct insertion of the drill sleeves in the distal plate area.
85-year-old woman, 13-C3, low supracondylar fracture treated with DHP.
40-year-old man, 13-C3 fracture treated with DHP.
23-year-old man, 13-C3 fracture treated with DHP.
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.