Femoral Recon Nail System
Paulo Barbosa, Christopher Finkemeier, Martin Hessmann
The Femoral Recon Nail (FRN) System, developed by the Intramedullary Nailing Expert Group, offers surgical entry point and locking options to accommodate varying preferences, enabling surgeons to treat a broad range of complex femur fractures. The nail was designed to enhance anatomical fit and to avoid complications like distal cortical impingement. The streamlined insertion instruments include features to facilitate implant placement and to reduce surgical time and complexity.
Choice of nail entry point
Obtaining the correct entry point is a key requirement in every intramedullary nailing procedure to avoid complications, especially valgus/varus deformities. The choice of the entry point depends on several factors including the fracture characteristics, associated injuries, and the technical familiarity of the surgeon with each nailing method. Many surgeons use nails that are designed for various entry points, as shown in these numbers: 9% lateral entry point, 28% piriformis fossa entry point, and 63% greater trochanter entry point nails.
Regional characteristics also play an important role in deciding the femoral nail entry point. For example, in the US, many surgeons are trained to use nails with a piriformis fossa entry point, but in other regions the greater trochanter is the option most frequently used.
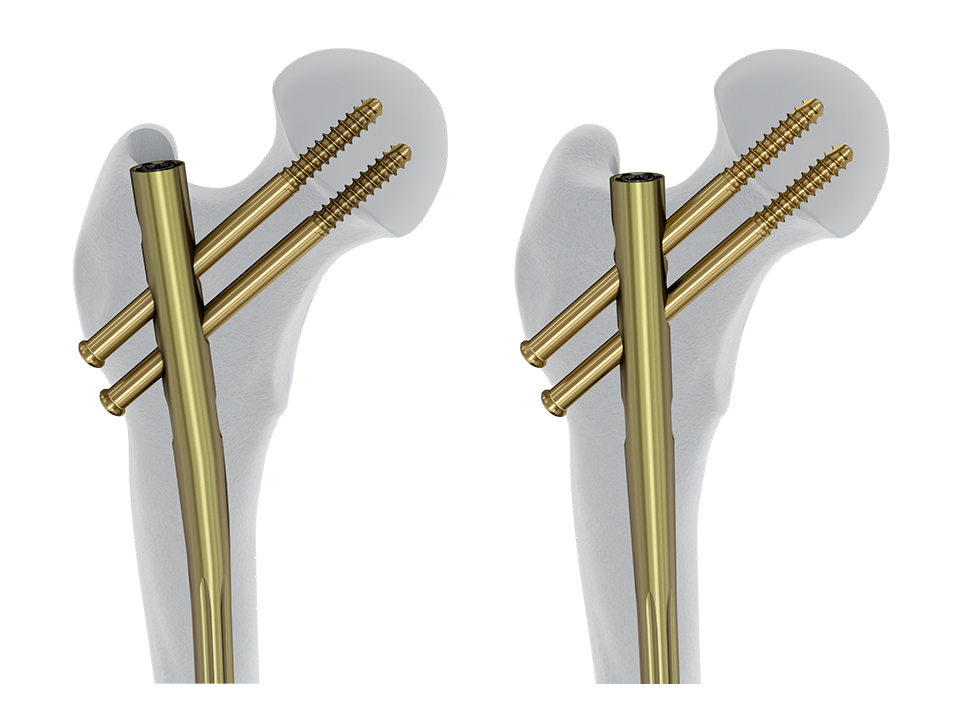
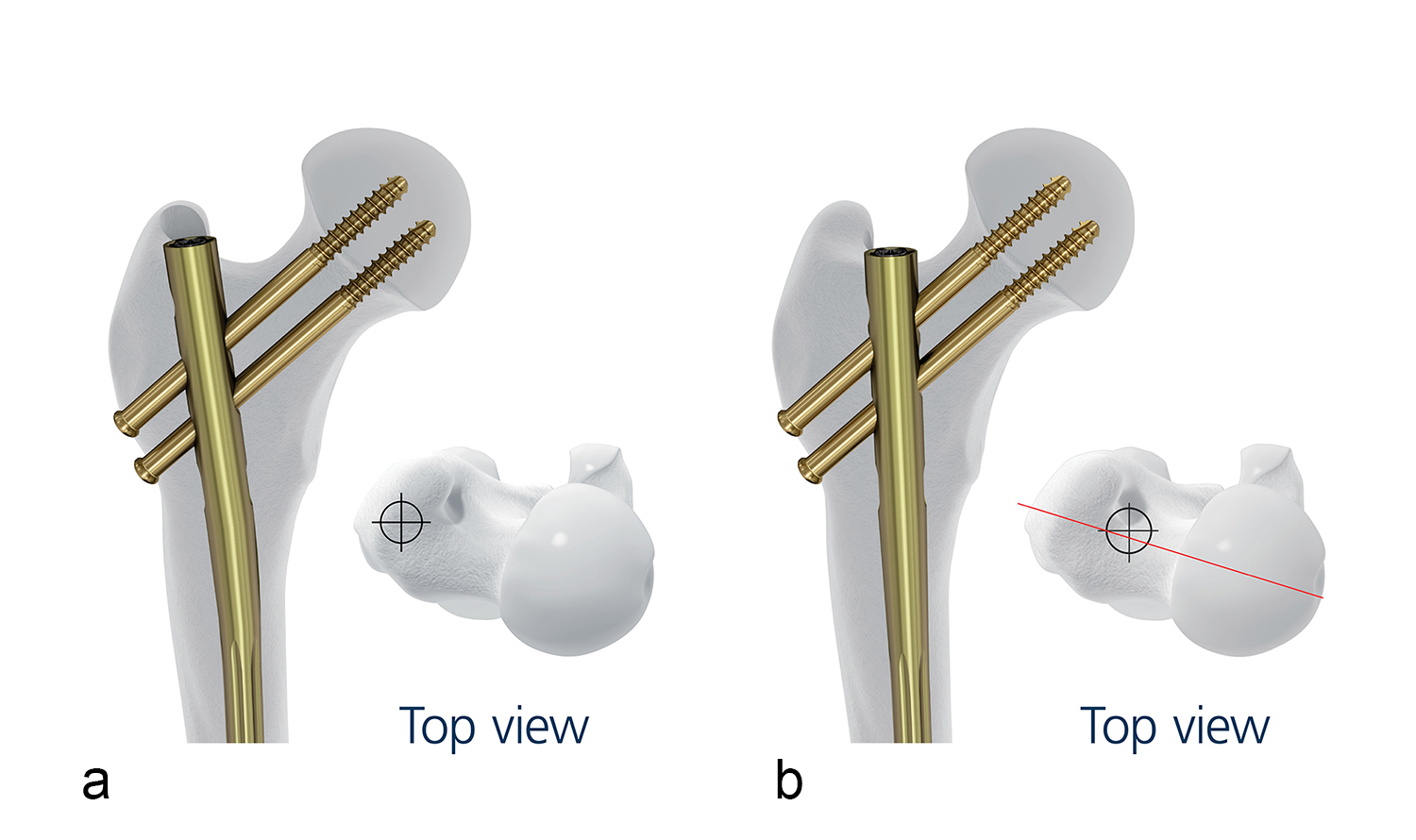
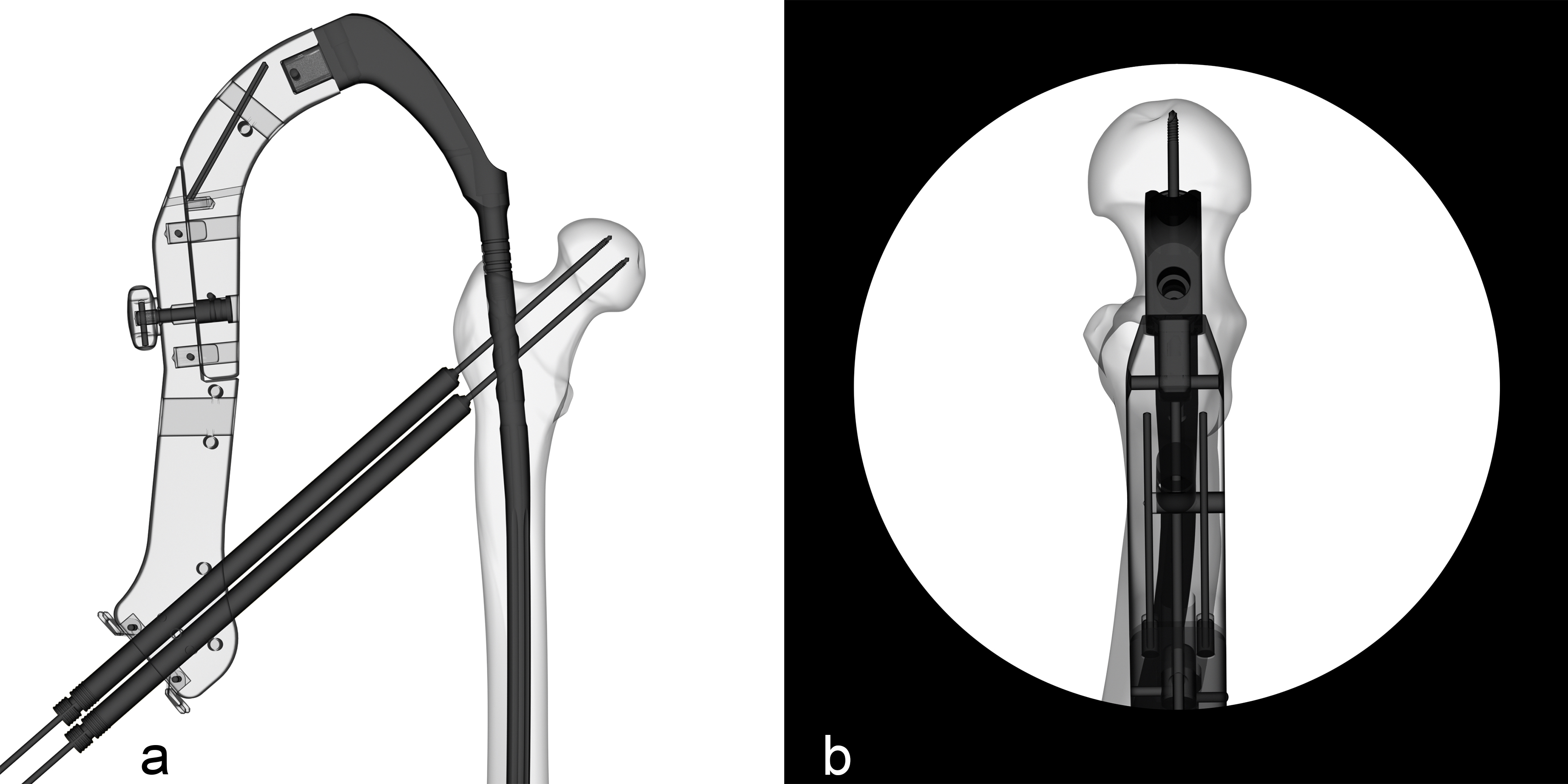
The FRN system offers surgeons the choice to use nails for a piriformis fossa entry point as well as for a trochanter tip entry point (Fig 1). In the AP view, the entry point for the tip of trochanter nail is on the tip or slightly lateral to the tip of the greater trochanter, in the curved extension of the medullary cavity (Fig 1a). This represents a point, 5° lateral of the femoral shaft axis, measured from a point just below the lesser trochanter. The entry point for the piriformis fossa nail is in line with the medullary canal in the AP and lateral views (Fig 1b).
Avoidance of distal cortical impingement
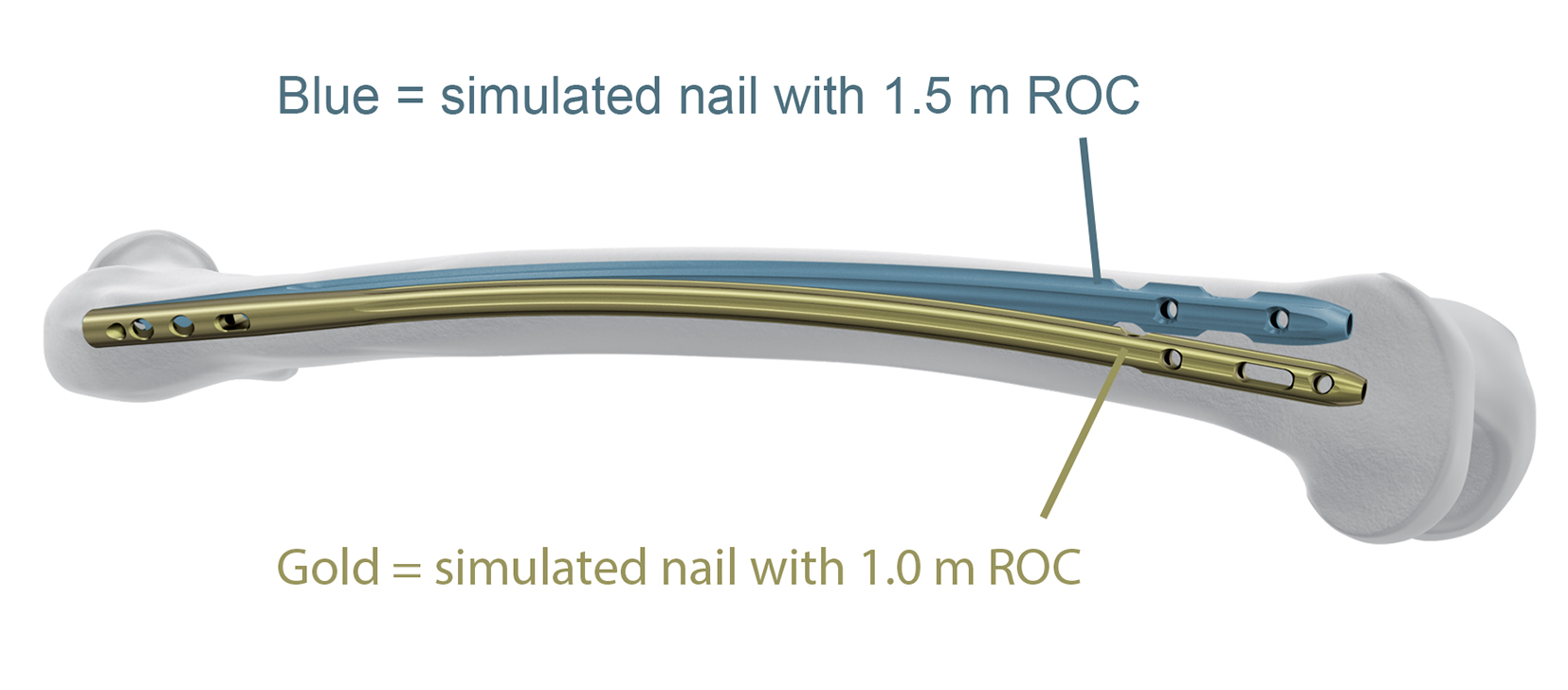
In addition to offering nails for different surgical entry points, the FRN system is also designed to solve a potential operative complication called distal cortical impingement [1]. This is often the result of the antecurvature bow of the patients femoral anatomy being greater than the curve of the nail. This geometrical mismatch may lead to anterior perforation of the cortex which may require revision surgery. The nails of the FRN System are specifically designed to enhance the anatomical fit by reducing the nail radius of curvature (ROC) to 1.0 m (Fig 2). This value is based on a multi-ethnic 3-D computational study [2] performed to identify the best ROC for the new nail.
References
1) Roberts JW, Libet LA, Wolinsky PR. Who is in danger? Impingement and penetration of the anterior cortex of the distal femur during intramedullary nailing of proximal femur fractures: preoperatively measurable risk factors. J Trauma Acute Care Surg. 2012 Jul;73(1):249-54.
2) Schmutz B, Amarathunga J, Kmiec S, Jr., Yarlagadda P, Schuetz M. Quantification of cephalomedullary nail fit in the femur using 3D computer modelling: a comparison between 1.0 and 1.5m bow designs. Journal of Orthopaedic Surgery and Research. 2016;11(1):53.
Avoidance of nail prominence
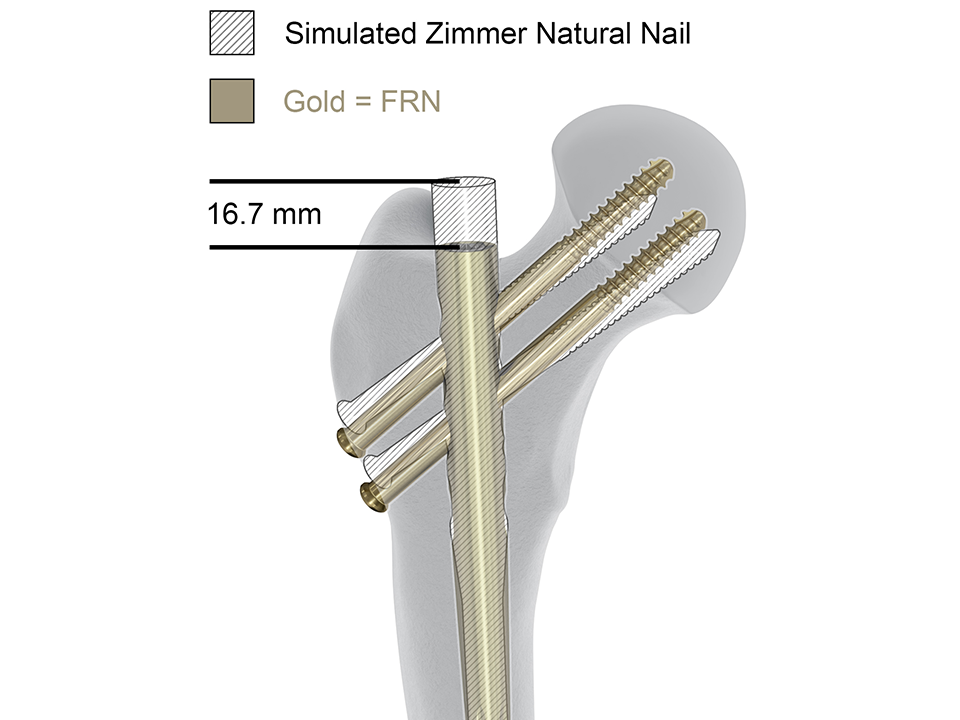
Another anatomical aspect is that some nails may lead to a too proud nail position. The shorter proximal nail end of the FRN reduces the risk of nail prominence compared to the Zimmer Natural Nail (Fig 3).
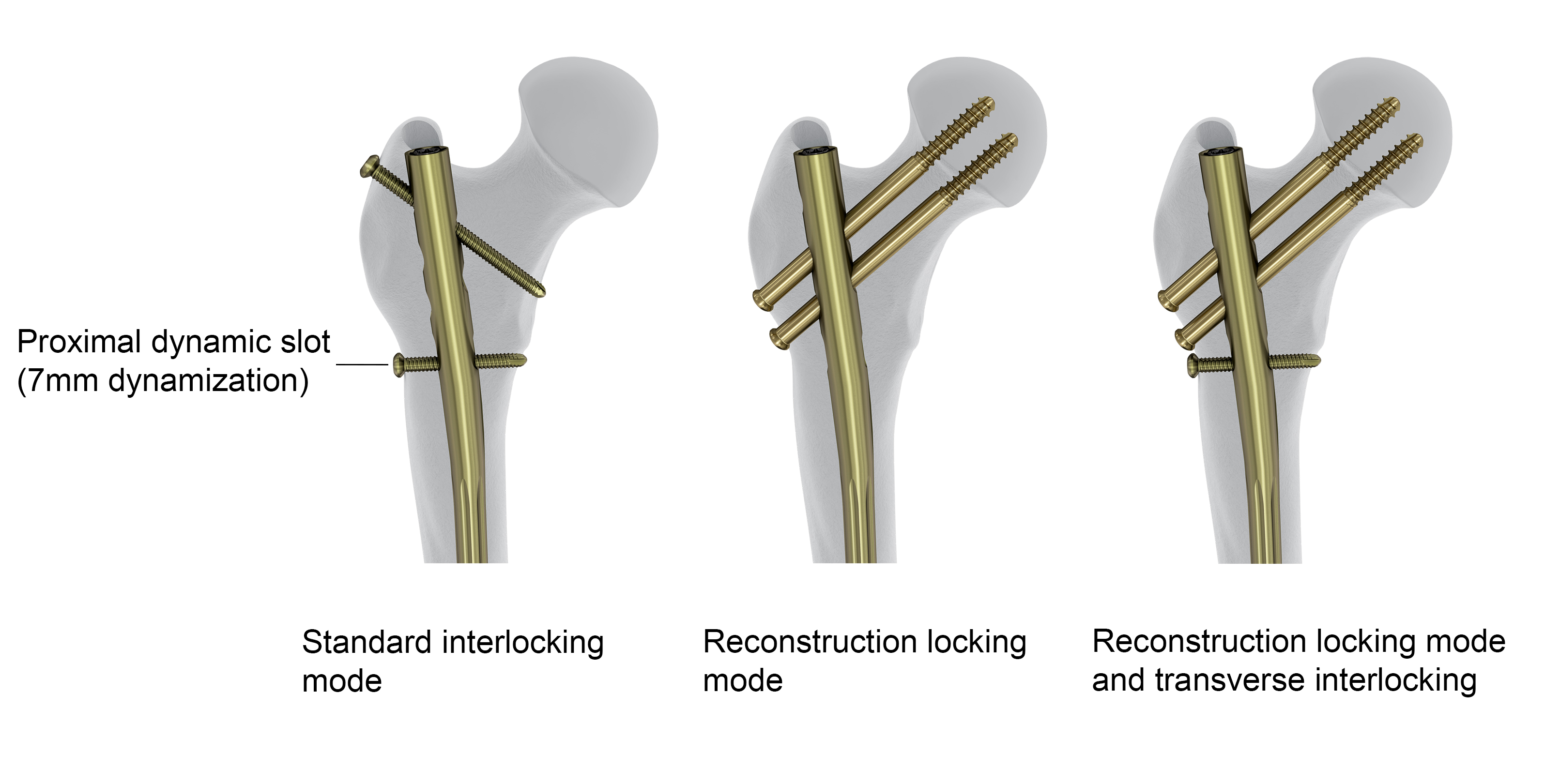
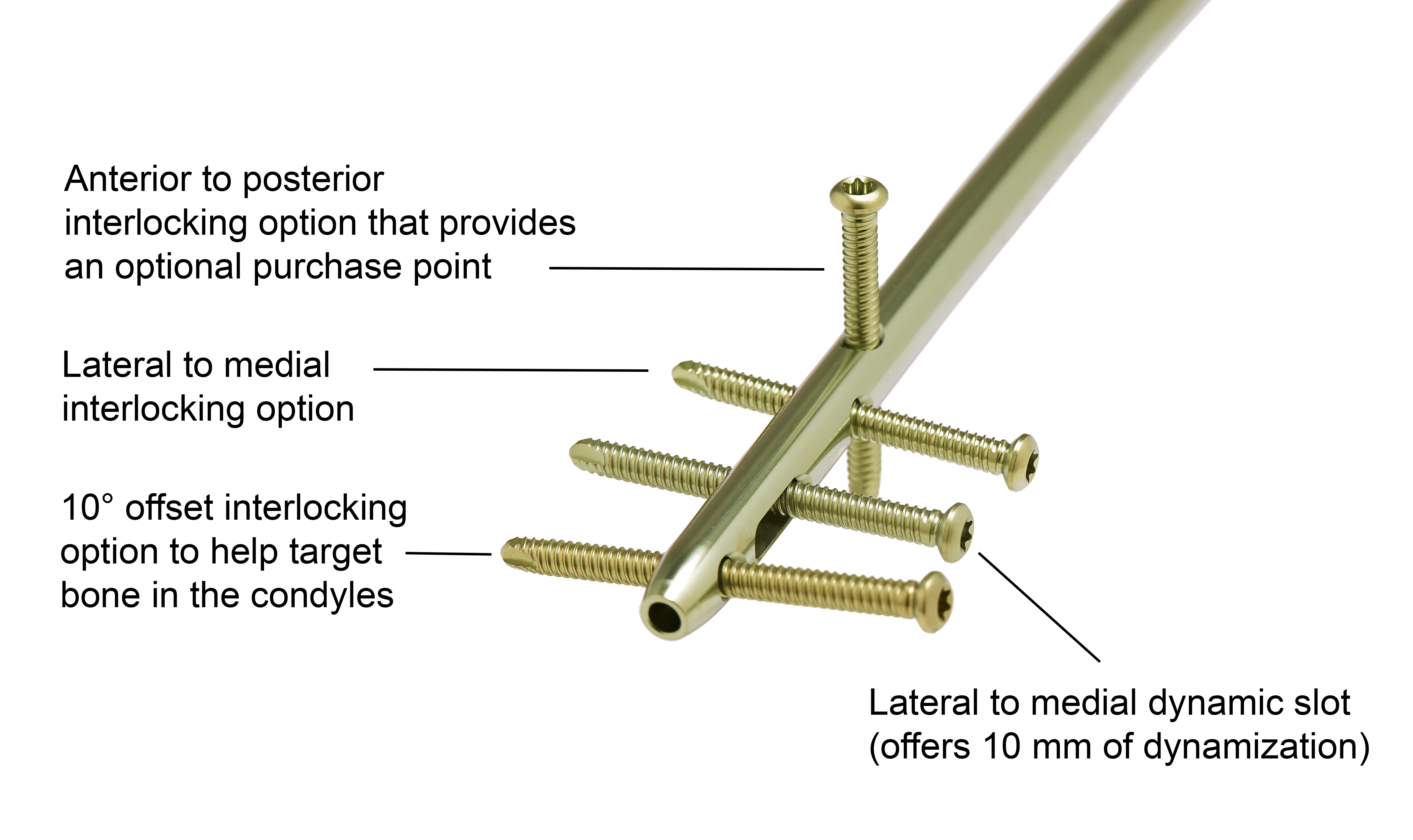
Proximal and distal locking options
Proximal and distal locking influence the anchorage of the nail in the bone and the stability provided at the fracture site. Achieving adequate implant anchorage can be a clinical challenge, especially in metaphyseal areas and in osteoporotic bone. The configuration of proximal and distal locking is also influenced by the fracture pattern and location. The FRN offers a choice of standard and reconstruction locking modes (Fig 4) to allow for the treatment of a variety of femoral fracture types. The nail is equipped with four distal locking options, including an oblique distal hole offset of 10° to better target bone in the condyles and an A/P hole that provides an optional purchase point and improves stability with this multiplanar configuration (Fig 5). There are proximal (7 mm) and distal (10 mm) slots in the nail to allow dynamization if required. If the nail is inserted very distally, it can happen that the distal dynamization slot cant be used. In such a case the use of the proximal dynamization slot is helpful to avoid the risk of nail protrusion into the knee joint.
Nail geometry
The cannulated left and right nails are made of titanium alloy (TAN) and are provided in the following diameters and lengths:
- 9 mm and 10 mm distal nail diameters with non-fluted shaft: 280 mm to 480 mm in 20 mm increments
- 11 mm, 12 mm, and 14 mm distal nail diameters with fluted shaft: 300 mm to 480 mm in 20 mm increments.
All nails with a distal nail diameter of 9 mm to 12 mm have a proximal nail diameter of 13 mm. The nail with a distal nail diameter of 14 mm has a proximal nail diameter of 14 mm. These proximal nail diameters are smaller than those of the Expert LFN and as such require less bone volume to be removed. Although the proximal nail diameters are smaller, mechanical testing has shown that the median fatigue limits of the FRN are significantly higher than the ones of the Expert LFN in standard and reconstruction locking modes.
The nail is designed for two 6.5 mm titanium recon screws in 130° CCD recon locking holes in the reconstruction locking mode at an anatomic anteversion of 14°. All nails use 5.0 mm titanium locking screws, and 5.0 mm angular stable locking screws can also be inserted to provide angular stable fixation.
Indications
The FRN system is intended for treatment of fractures in adults and adolescents (12-21 years) in which the growth plates have fused. Specifically, the system is indicated for:
- Subtrochanteric fractures
- Ipsilateral neck/shaft fractures
- Femoral shaft fractures
- Impending pathologic fractures
- Malunions and nonunions.
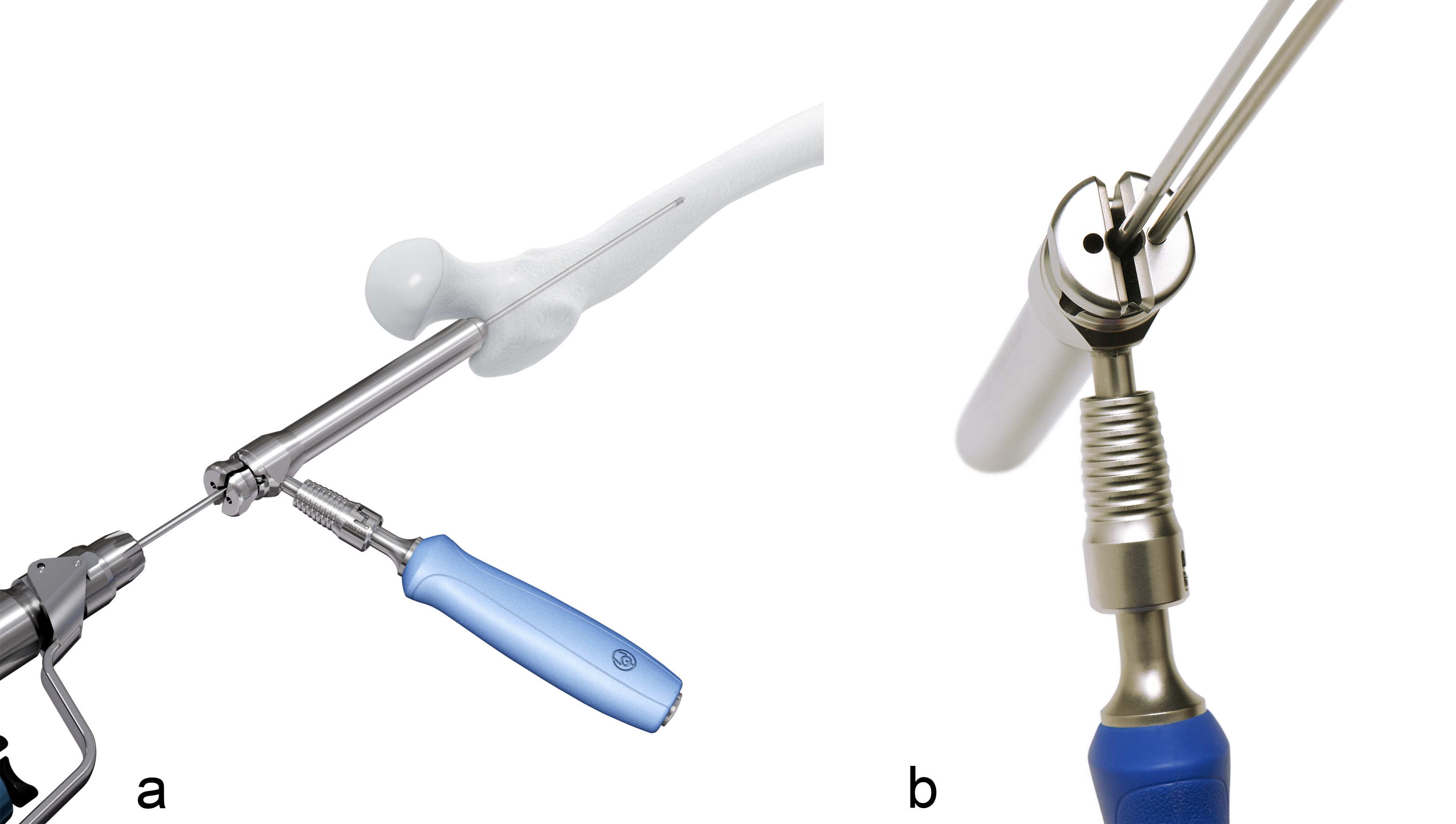
Multihole wire guide
For the accurate insertion of the guide wire, the FRN system offers a multihole wire guide (Fig 1). If the first guide wire is inserted in an incorrect position, a second guide wire can be inserted through one of the additional holes in the multihole wire guide at 5 mm from the central hole. The wire guide can also be rotated in 90° steps to facilitate the insertion of a second guide wire.
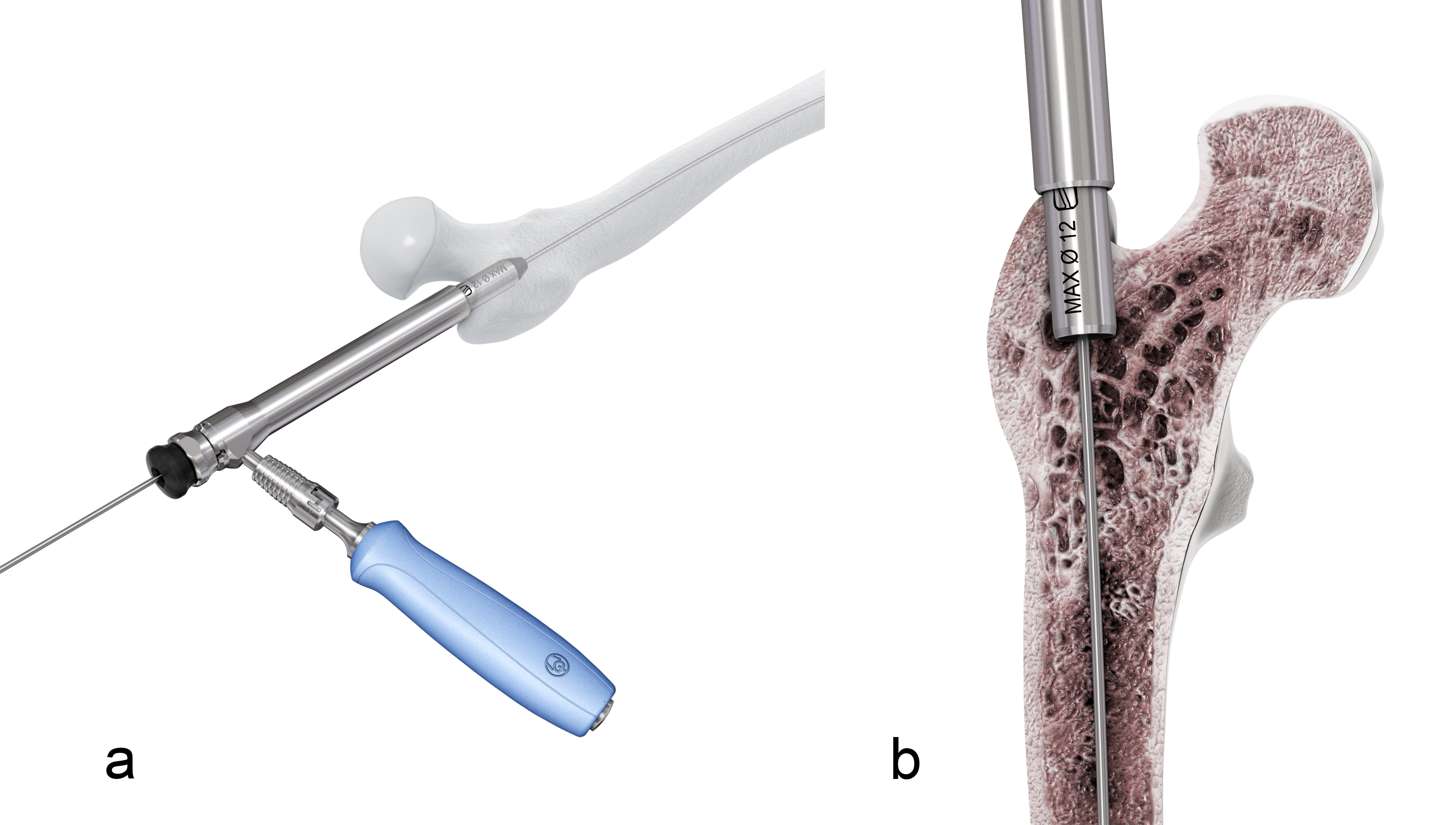
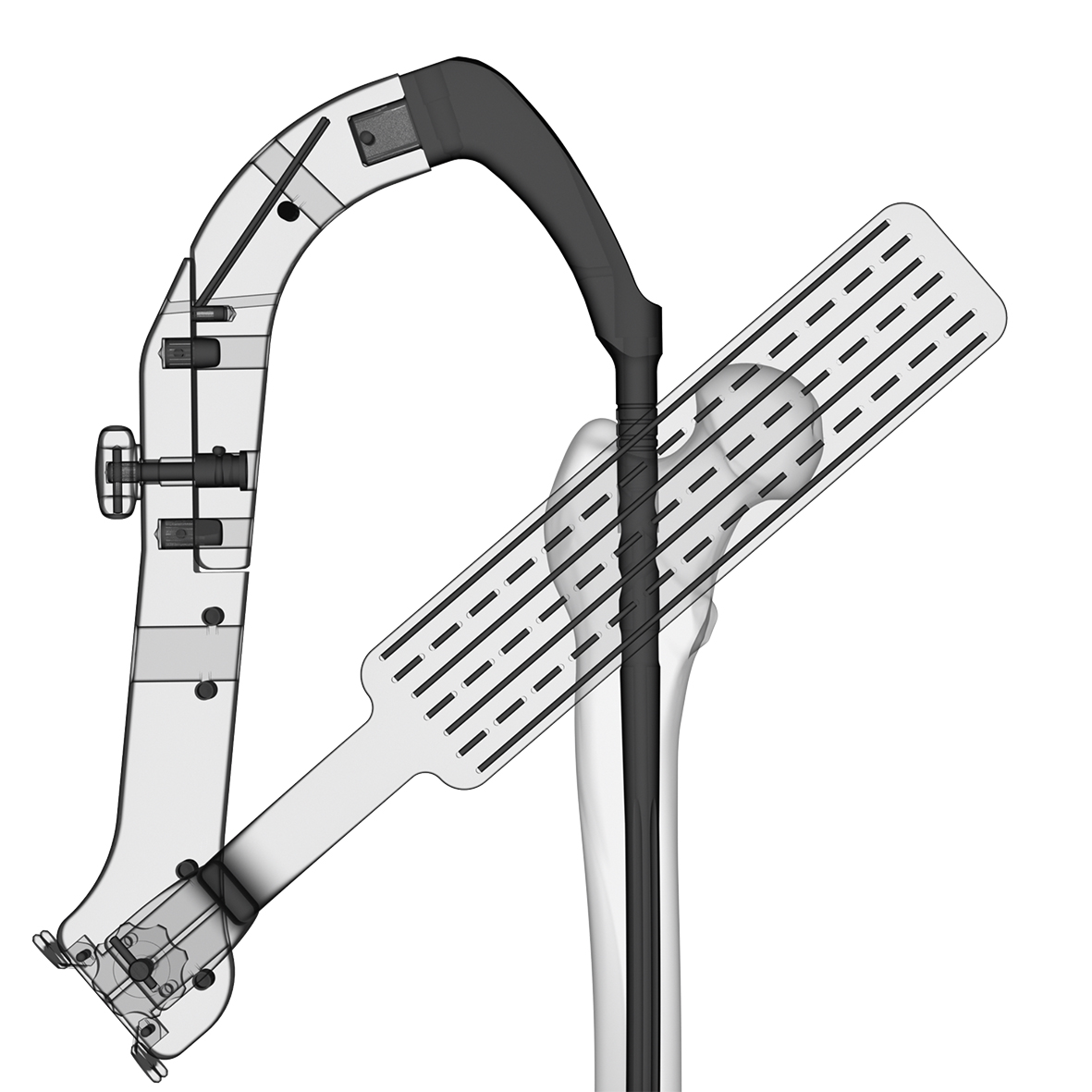
Reamer protection tube
There is an optional reamer protection tube that can be inserted into the bone after opening the femoral canal. This instrument is used to help protect the proximal metaphysis during reaming avoiding undesired enlargement of the entry point or reaming of the lateral wall (Fig 2). The reamer protection tube can only be used with reamer heads up to 12 mm (for 9 mm, 10 mm, and 11 mm nails).
QUICK CLICK Self Retaining Technology
Orthopedic instruments should be intuitive to allow the surgeon and the operating room teams to focus completely on the patient and the procedure. The FRN system is designed to address the need to increase the procedural efficiency in the operating room as described in the following. The QUICK CLICK Self Retaining Technology is designed to ensure a fast and effective assembly of the insertion handle to the nail (Fig 3), potentially improving surgical efficiency and reducing OR time.
Insertion handle and guide wire aiming device
Placement of the guide wires for the recon screws is a critical step in the nailing procedure influencing the clinical success of the implant. Radiolucent insertion handles with radiographic indicators and the optional guide wire aiming device assist in guide wire placement (Figs 4 and 5), which can reduce the required OR time to achieve accurate guide wire positions. The instruments allow the surgeon to identify the predictive pathway of the guide wires before actually inserting any.
Case provided by Christopher Finkemeier, Carmichael, USA
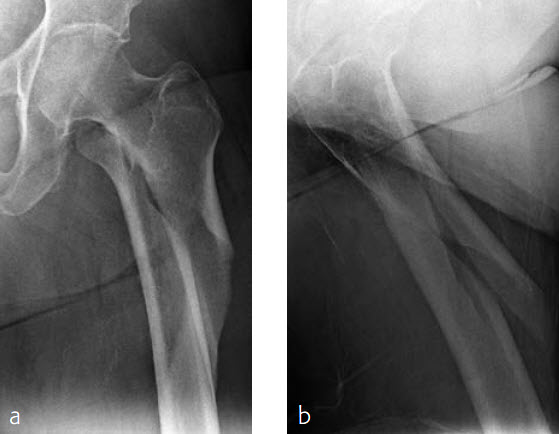
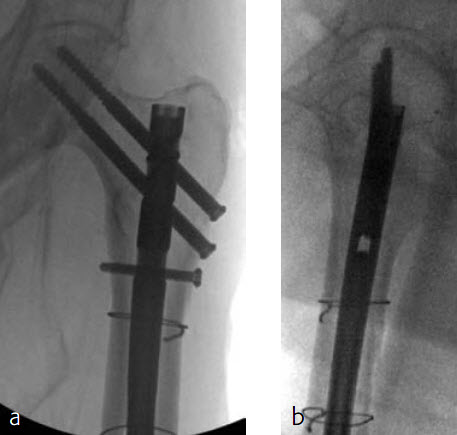
Case 1: Subtrochanteric femur fracture
An 86-year-old patient fell at home while dressing, sustaining a subtrochanteric left femur fracture (Fig 1). The CT scan confirmed no involvement of the intertrochanteric region or the piriformis fossa. Fixation was with FRN for piriformis fossa entry point in reconstruction locking mode and transverse locking (Fig 2).
Case provided by Martin Hessmann, Fulda, Germany
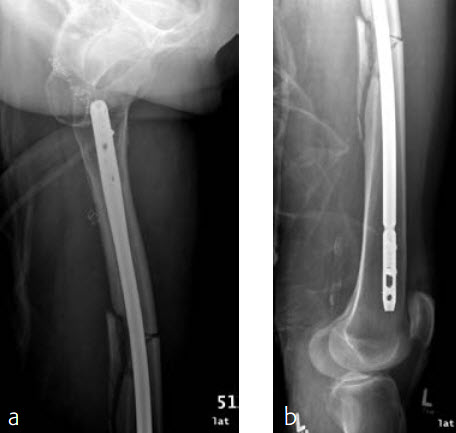
Case 2: Left femur fracture
A 70-year-old female patient suffered an AO 32-B3 fracture of the left femur (Figs 3 and 4). Fixation with the FRN for a tip of the trochanter entry point (nail diameter 10 mm; nail length 400 mm; reaming to 12 mm) in standard interlocking mode (Figs 5 and 6). Proximal locking with antegrade and transverse dynamic locking positions. Distal locking with two lateral to medial locking screws in static locking position.
Advances in Femoral Nailing with special focus on the Femoral Recon Nail system
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.