Tibial Tuberosity Advancement (TTA) System
Erik Asimus, Brian Beale, Randy Boudrieau, Loïc Déjardin, Michael Kowaleski
Cranial cruciate ligament (CrCL) failure in dogs is a pervasive injury that results in abnormal joint motion, progressive osteoarthritis, meniscal lesions, and loss of function. Several high tibial osteotomies, among which the forerunner is the tibial plateau leveling osteotomy (TPLO), have been devised over the past 20 years to neutralize the cranial tibial thrust (CrTT) force. This tibiofemoral shear force is responsible for joint instability following CrCL failure. The Tibial Tuberosity Advancement (TTA) system has been used as an alternative to the TPLO to restore joint stability during weight-bearing.
Unlike the TPLO, which relies on a reduction of the tibial plateau slope via a radial osteotomy, neutralization of the CrTT with the TTA is achieved by advancing the tibial tuberosity until the angle between the straight patellar ligament and the tibial plateau remains 90 or less, regardless of the stifle joint flexion/extension angle. The advancement of the tibial tuberosity is allowed by creating an osteotomy of the tibial crest in the frontal plane followed by plate stabilization after placement of a wedge within the osteotomy to maintain the gap width. A bone graft is placed within the osteotomy gap to enhance healing. Furthermore, the TTA can be used to treat CrCL rupture cases with concomitant medial patellar luxation (MPL) via the use of offset spacers that induce a lateral transposition of the tibial crest.
System design
The TTA system (Fig 1) is indicated for the treatment of CrCL disease in canines. It is compatible with small and mini fragment systems and the plate is available in right and left versions as well as in the following sizes:
- 2.4 mm/2.7 mm TTA plate: 53 mm (size 4) and 65 mm (size 5)
- 2.4 mm/3.5 mm TTA plate: 78 mm (size 6), 90 mm (size 7) and 104 mm (size 8).
The locking screw trajectories in the proximal plate section are designed to optimize screw purchase within the tibial crest. Furthermore, the incorporation of locking technology (Fig 2) permits a fixed-angle device to increase construct stability.
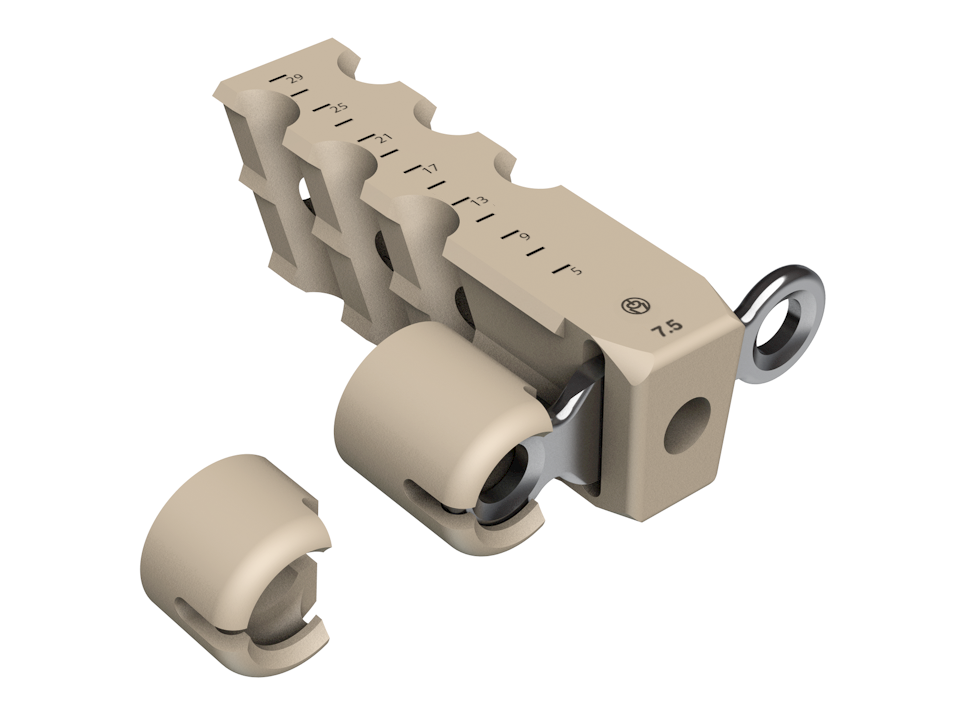
Wedges and spacers are made of radiolucent PEEK (Fig 3). The Wedges are available in 8 widths (4.5, 6, 7.5, 9, 10.5, 12, 13.5 and 15 mm) and can easily be cut to the desired length to accommodate the tibial width using the graduated length markings. Additionally, 3 or 5 mm PEEK offset spacers may be snapped to the wedge allowing for simultaneous treatment of MPL (Fig 4).
Case 1: 2-year-old labrador retriever
(Case provided by Karen Perry and Loïc Djardin, East Lansing, USA)
A 2-year-old labrador retriever presented for assessment of a moderate intermittent weight-bearing left pelvic limb lameness of four months duration. Orthopedic examination revealed moderate stifle joint effusion, medial buttress formation of the proximal tibia, crepitus, and a moderate pain response upon manipulation and extension of the stifle joint. Joint laxity was evident with both cranial drawer and CrTT. There was also mild effusion palpable in the right stifle joint, but this was otherwise unremarkable upon examination.
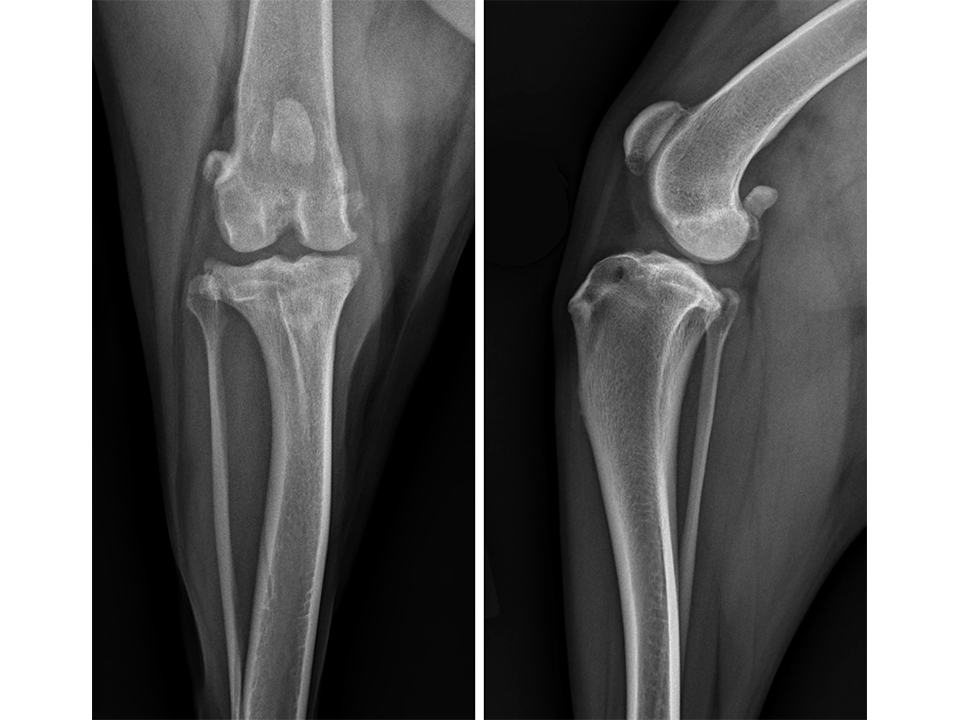
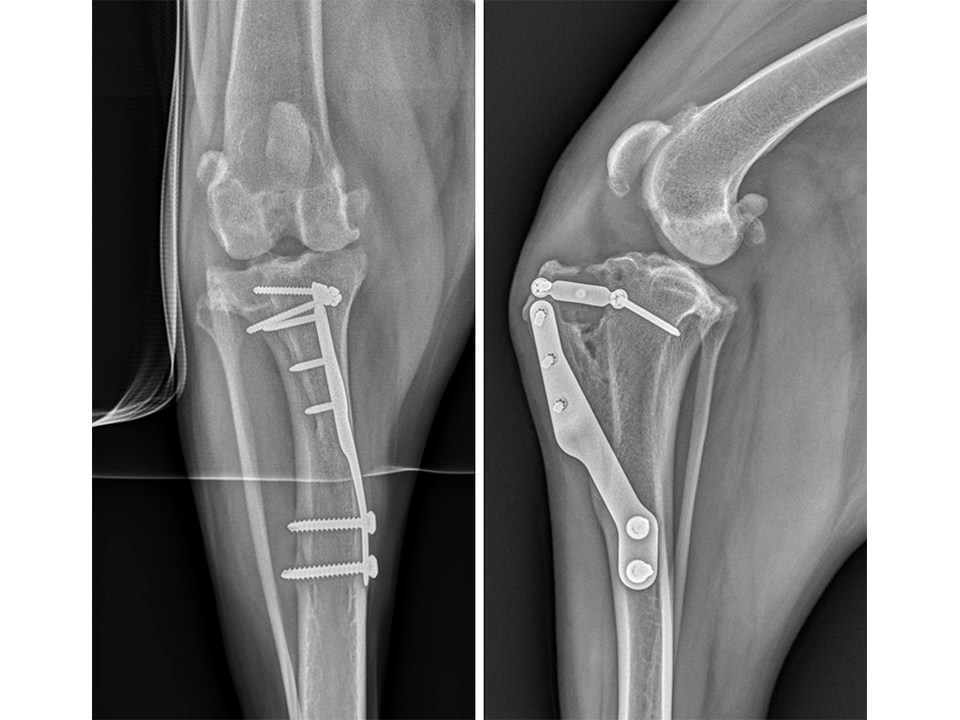
Radiographs of both stifle joints (Fig 5 and 6) revealed bilateral moderate joint effusion and minimal bony proliferation along the distal aspect of the patella. Considering the clinical findings, these radiographic signs were interpreted as minimal bilateral osteoarthritis secondary to CrCL disease.
The left stifle was evaluated for a Tibial Tuberosity Advancement (TTA) and the owner was advised that stabilization of the right stifle would likely be required in the future. Preoperative TTA planning was conducted using anatomic tibial plateau and patellar tendon angle landmarks. A 13.5 mm wedge and a size 6 plate were selected.
Under anesthesia, exploration of the left stifle joint revealed a partial rupture of the CrCL, the remnants of which were debrided. A caudal pole tear of the medial meniscus was identified and medial caudal pole hemimeniscectomy performed.
A frontal plane bicortical osteotomy of the distal half of the tibial tuberosity was created. The size 6 plate was anatomically contoured to fit the medial surface of the tibia. The cranial edge of the plate was placed parallel to the cranial aspect of the tibial tuberosity at the level of the insertion of the straight patellar tendon. The proximal screw hole in the distal plate section was positioned over the cranial cortex of the tibia. The most proximal screw hole in the plate was appropriately positioned. The plate was then secured to the medial surface of the tibial tuberosity using three 2.4 mm locking screws in the proximal portion of the plate. The osteotomy was completed proximally and the spreader was used to distract the osteotomy. A depth gauge was used to measure the width of the tibial tuberosity proximally and the 13.5 mm wedge length was trimmed accordingly. The cranial and caudal tabs of the wedge were contoured to fit the medial tibial cortex. Pointed reduction forceps were used to compress the distal end of the tibial tuberosity to the tibial shaft ensuring adequate bony contact at this level. A 2.4 mm cortical screw was inserted into the caudal tab of the wedge, angling caudally and distally. A 3.5 mm cortical screw was inserted into the proximal screw hole in the distal plate now overlying the center of the tibial diaphysis. A 2.4 mm cortical screw was then inserted into the cranial tab of the wedge, angling cranially and proximally. Finally, a 3.5 mm cortical screw was inserted into the distal screw hole in the distal plate. Stability in CrTT was ensured. The surgical site was flushed and a bone graft inserted into the osteotomy gap (Osteoallograft Orthomix Fine). Closure was routine.
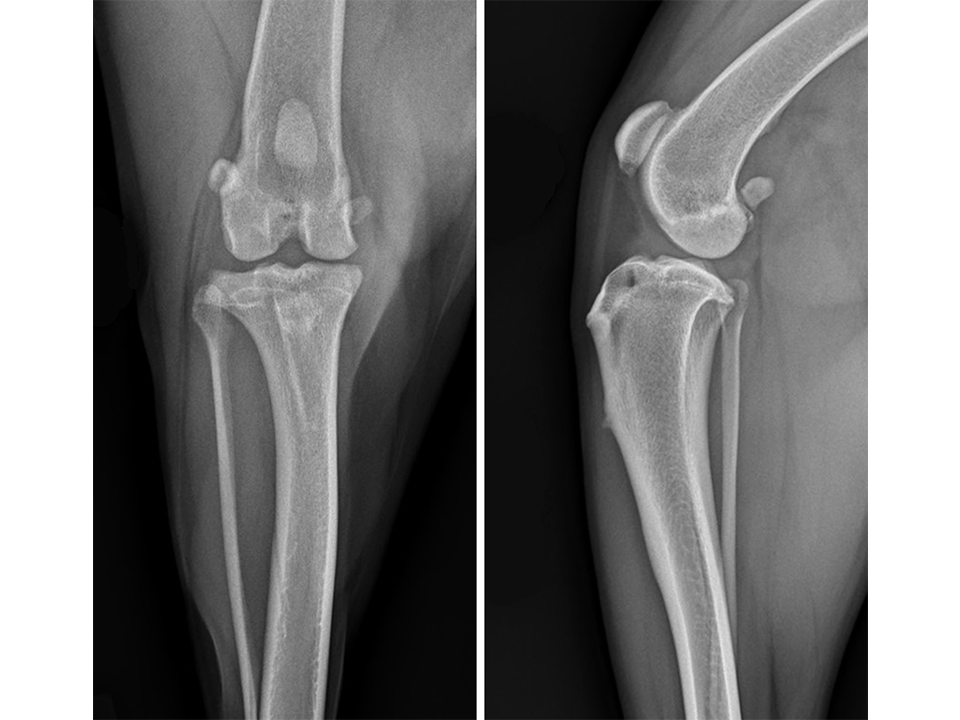
Immediate postoperative radiographs (Fig 7) revealed satisfactory implant and osteotomy positioning. Radiographs obtained 10 weeks postoperatively (Fig 8) showed no evidence of implant-associated complications and partial bone healing within the osteotomy gap. Osteoarthritic changes within the joint were static. Clinically at this stage, mild bilateral pelvic limb lameness was apparent bilateral stifle joint effusion. The left stifle joint was stable in CrTT with no pain response upon stifle joint manipulation.
The patient presented again 11 months postoperatively for assessment of right pelvic limb lameness associated with CrCL rupture. At this stage severe right pelvic limb lameness was evident but no lameness of the left pelvic limb was observed. While the right stifle joint was unstable in cranial drawer and CrTT, the left stifle remained stable with no pain response upon palpation over the implants and a normal range of motion of the joint. Radiographs of the previously operated left stifle (Fig 9) revealed no implant-associated complications and healing of the osteotomy. The osteoarthritic changes were static radiographically. TTA was performed on the right tibia at this time using a 13.5 mm wedge and a size 6 plate as had been used on the left previously.
Case 2: 18-month-old labrador retriever
(Case provided by Karen Perry and Loc Djardin, East Lansing, USA)
An 18-month-old labrador retriever presented for assessment of right pelvic limb lameness of ten days duration. A left TTA had been performed 6 months previously for treatment of CrCL disease. Gait assessment revealed a severe weight-bearing right pelvic limb lameness. Orthopedic examination revealed moderate right stifle joint effusion, medial buttress formation of the proximal tibia, and a palpable click upon manipulation of the stifle joint. Grade one MPL was also evident. There was a severe pain response upon manipulation of the right stifle joint and laxity was evident in both cranial drawer and CrTT. The left stifle was stable in CrTT with no pain response on palpation over the previously placed implants. There were no other salient findings on the orthopedic exam.
Radiographs of the right stifle (Fig 10) revealed moderate joint effusion and periarticular osteophytosis likely secondary to CrCL disease with concomitant MPL.
The right stifle joint was considered a suitable candidate for a tibial tuberosity transposition and advancement (TTTA) to stabilize the CrCL deficient stifle and realign the quadriceps mechanism with one surgical procedure. Preoperative TTTA planning was conducted as previously described and a 12 mm wedge and a size 7 plate were selected.
Under anesthesia, exploration of the right stifle joint revealed complete rupture of the CrCL, the remnants of which were debrided. Compression injury to the caudal horn of the medial meniscus was identified and medial hemi-meniscectomy of the caudal pole performed.
Following a frontal plane osteotomy of the tibial tuberosity, it was estimated that to re-align the quadriceps mechanism appropriately, 5 mm of lateralization of the tibial tuberosity would be required. The size 7 plate was contoured to fit the medial surface of the tibia, while at the same time placing an additional slight bend to the plate at the midportion so as to allow this lateralization to occur. Plate application, tibial tuberosity advancement, and trimming of the wedge were performed as described in the previous case; a 5 mm spacer was additionally attached to the cranial tab of the wedge in order to also transpose the tibial tuberosity laterally. The medial cortex of the tibia was recessed slightly using a high-speed drill immediately caudal to the distal extent of the osteotomy to allow unrestrained positioning of the additional curve in the contoured plate. Plate fixation was achieved using 2.4 mm locking and 3.5 mm standard cortical screws identical to the previous case. The wedge was secured in place using two 2.4 mm standard cortical screws with the cranial screw applied through the spacer. Stability in CrTT was ensured as was mediolateral stability of the patella. The surgical site was flushed and a bone graft inserted into the osteotomy gap (Osteoallograft Orthomix Fine). Closure was routine.
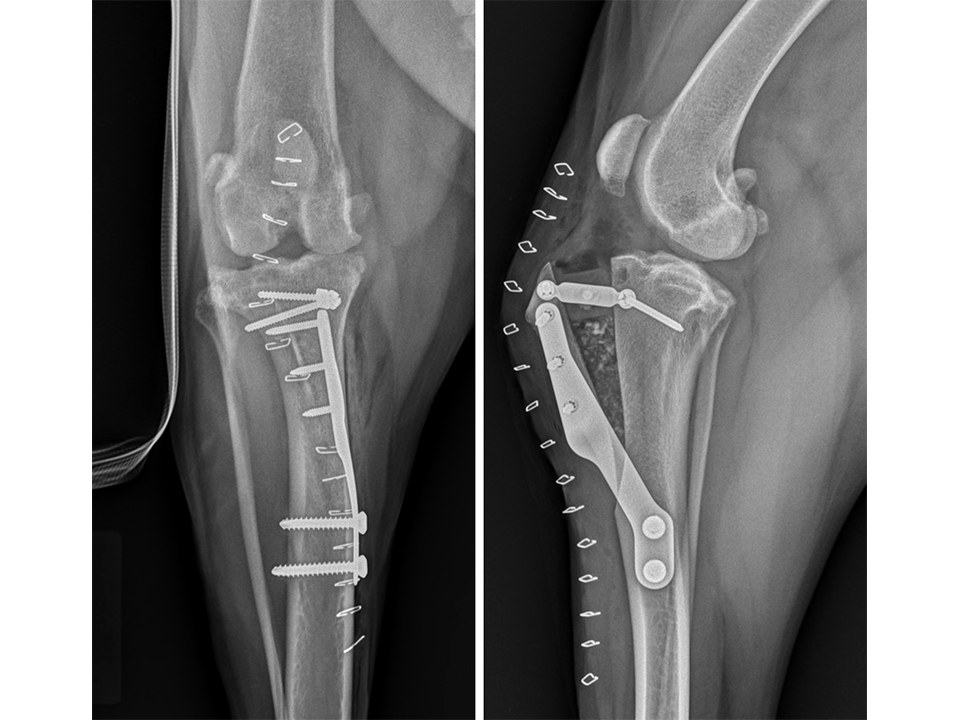
Immediate postoperative radiographs (Fig 11) revealed satisfactory implant and osteotomy positioning with the patella appropriately positioned within the femoral sulcus. There was no laxity in CrTT and the patella could not be luxated. Radiographs obtained 10 weeks postoperatively (Fig 12) revealed no evidence of implant-associated complications and smooth osseous proliferation bridging the osteotomy gap. Osteoarthritic changes within the joint were mildly progressive. Clinically at this stage, no pelvic limb lameness was evident. The range of motion of the right stifle joint was within normal limits. The stifle was stable in CrTT and the patella could not be luxated. No pain response was noted with the physical examination.
VET Tibial Tuberosity Advancement System
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.