VA-LCP Proximal Tibial Plate 3.5 System
Matthew Graves, Sean Nork, Christian Ryf
Open reduction and internal fixation with plates and screws is considered to be todays gold standard method for treatment of proximal tibial fractures. A broad variety of plates is available for this anatomic area, with special features providing solutions to different clinical problems.
The VA-Locking Proximal Tibial Plate 3.5 covers various indications with one (small fragment) implant, which had previously been restricted to different plate types (small and large fragment).
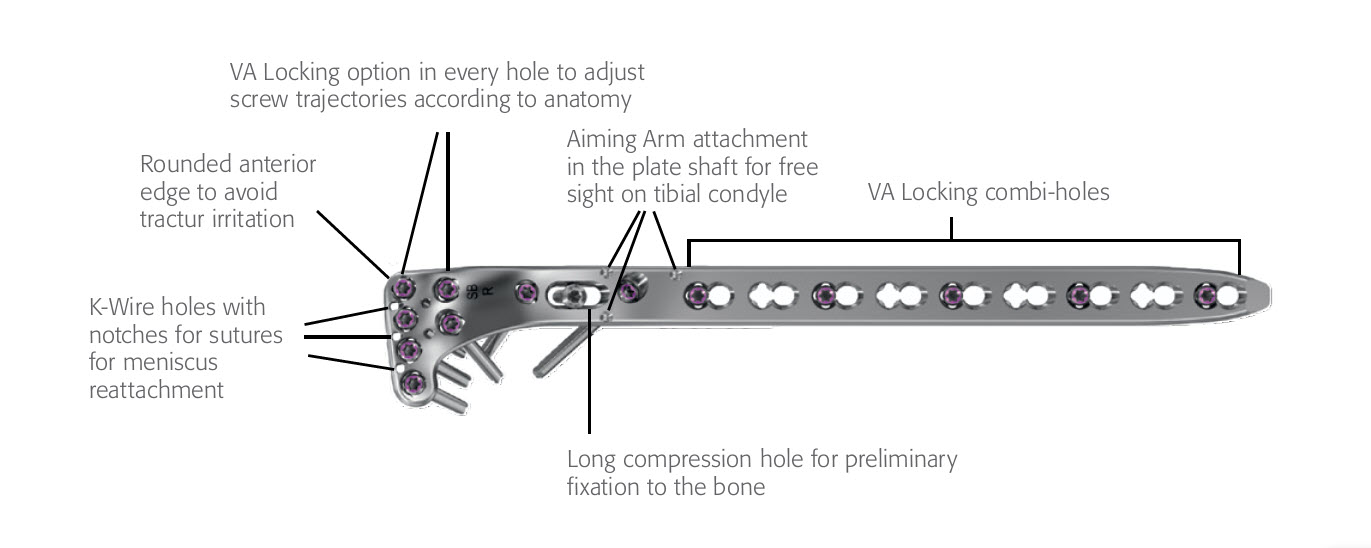
Design features (Fig 1)
- The proximal row of 4 rafting screws ideally supports depression fractures of the tibial plateau.
- The flexible neck area, together with the long-hole accepting compression screws, allows buttressing of split-type fractures.
- In addition, the overall plate stability (same construct stability as a LCP 4.5/5.0 narrow plate in the shaft) allows for the treatment of complex metaphyseal, bicondylar and (associated) shaft fractures with small fragment screws, which have until now been restricted to large fragment plates.
Caring about soft-tissue
Literature shows that the tibia is a highly variable bone. A good plate fit is essential as it supports a stable fracture fixation, improves screw-plate mechanics, prevents malreductions, and consequently avoids impingement of the overlying soft-tissue.
A CT scan study covering 170 bones was performed to define the ideal shape for the VA-LCP Proximal Tibial Plate. As a consequence of the findings of this study, two plate shapes were developed to cover these bone variances and achieve an optimal plate fit (Fig 2).
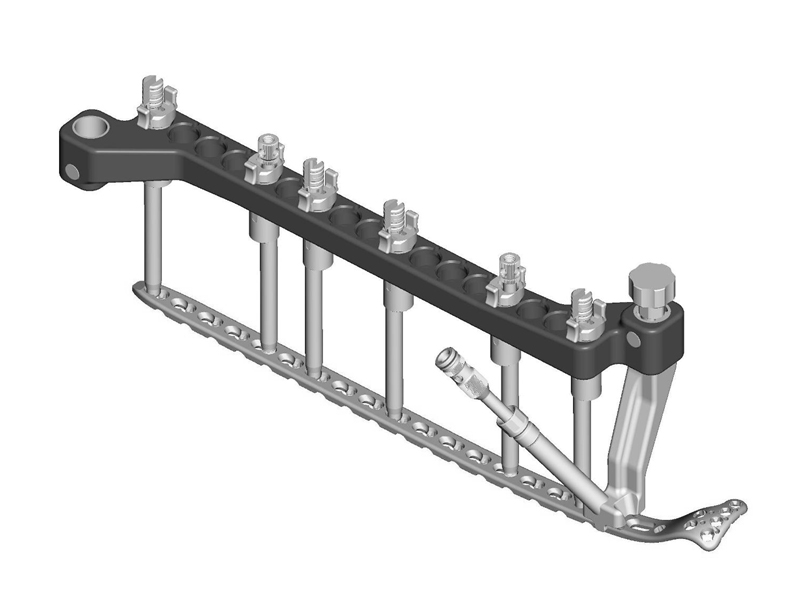
Suture-holes in the plate head facilitate meniscus reattachment, and the aiming arm makes a minimally-invasive percutaneous screw insertion possible.
Variable Angle (VA) screw technology to adapt screw direction according to clinical need
The concept of fixed angle locking screws is both clinically proven and widely spread. But with the VA locking technology, with its screw variability of 15° in each direction (Fig 3), additional clinical problems can also be solved:
- Adapt the screw trajectory to varying tibial plateau inclinations, thereby avoiding joint penetration
- Adapt the screw trajectory to condyle size by distributing screws over the tibial plateau
- Capture the fracture fragments and target specific anatomic regions
- Anchor the screws in good quality bone
- Avoid collisions with other implants or prostheses
- All screw types of the small fragment set can be used in any plate hole (3.5 mm VA Locking Screws, 3.5 mm Cortex Screws, 4 mm Cancellous Bone Screws; in nominal angle also 3.7 mm Dynamic Locking Screws, and 3.5 mm Locking Screws).
First clinical experiences with the VA-LCP Proximal Tibial Plate system
During the Market Preference Evaluation, users of the VA-LCP Proximal Tibial Plate rated the performance of the system in terms of plate fit, aiming arm design and handling, and simplicity of surgical technique as excellent in the majority of cases. Plate fitting, screw configurations, the screw variability, and the handling of screw insertion were also rated as being good in the majority of cases, all indicating that the VA-LCP Proximal Tibial Plate provides an effective proximal tibial fracture solution.
While the Market Preference Evaluation of the new VA-LCP Proximal Tibial Plate 3.5 system outlined its needs, advantages and benefits, a highly sophisticated new plate and screw system is still no guarantee of a good result. The key steps in a successful treatment of a complex proximal tibia fracture remain the same, namely, the choice and careful performance of the adequate approaches and the attentive and anatomical reduction of the joint and the axes. Clearly, an exact preoperative plan is also essential in order to fulfill all the biomechanical requirements. However, the new VA-LCP Proximal Tibial Plate 3.5 system offers a comprehensive variety of screw options, instruments, and plate features that support the surgeon to implement the above mentioned key steps, for a successful outcome.
An aiming arm is available for minimally-invasive screw insertion, and is suitable for all plate types (right, left, small bend, large bend).
Case provided by Christian Ryf, Davos, Switzerland
Case: Hiking accident
A 70-year-old female patient had an accident while hiking. Osteoporosis was preexisting but with asymptomatic moderate degenerative osteoarthritis of the knee with chondrocalcinosis of the lateral compartment (Fig 1 and 2).
The area was functional soon after treatment (Fig 3), and the patient was able to experience weight bearing of 20 kg for the first 6 weeks. She was completely pain free after 6 weeks (Fig 4) with excellent muscular function and coordination, therefore unlimited weight bearing after the first follow-up was enabled.
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.