Long Nail - MultiLoc Humeral Nailing System
Martin Hessmann, Stefaan Nijs
Long nail - MultiLoc Humeral Nailing System
In 2011, the MultiLoc Proximal Humeral Nail (PHN) was launched, which was designed in an effort to improve nailing osteosynthesis stability and thus expand the indications for nailing at the proximal humerus. The nail is Xmas tree in design, with the innovative screw-in-screw technology that improves fixation in osteoporotic bone. The modular implant configuration allows for the treatment of both simple and complex fractures.
A long version of the MultiLoc nail was developed in order to treat such issues as fractures of the humeral diaphysis, fractures of the proximal humerus with diaphyseal extension, as well as combined fractures of the proximal humerus and the humeral diaphysis. This longer version nail, which is available in 7.0 mm and 8.5 mm diameters and in lengths from 180 mm to 315 mm, completes the MultiLoc Humeral Nailing System creating a single comprehensive system for all fractures amenable for nailing.
The straight nail design, with its corresponding central insertion point, improves anchorage in the strong subchondral bone at this location, and potentially avoids insertion through the fracture site in typical 3-part fractures, while preserving the hypovascular supraspinatus footprint. Due to its straight design, the implant can only be used in an antegrade manner. The proximal locking concept of the new long nail is similar to the existing MultiLoc PHN, and comprises the innovative screw-in-screw technology (Fig 1) that permits a more specific treatment of proximal humerus fractures.
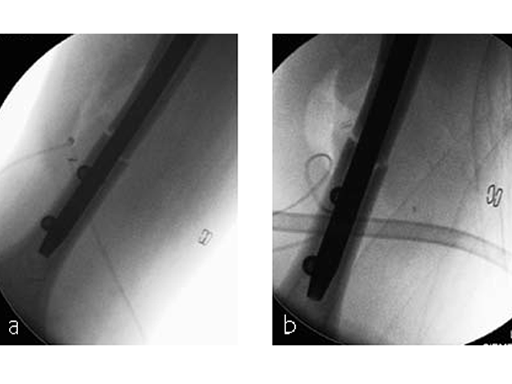
Either an ascending screw to support the medial calcar region or a compression screw for the compression of transverse or short oblique fractures can be inserted in the long nail (see Fig 2). The latter allows bicortical compression, which is an easy-to-handle feature improving rotational stability in transverse and short oblique fractures. The nail must be over-inserted by at least the same amount of interfragmentary travel that is anticipated, because, as compression is applied, the nail will back out at the insertion site. The instrumentation comprises color coding for easy assembly, while self-holding mechanisms facilitate handling of sleeves and screwdrivers. Flippable aiming arms for left and right nail instrumentation help to reduce inventory and costs.
The three distal locking screws, which are placed freehand, are located in two different planes to reduce implant toggling, and increase stability of the osteosynthesis. The locking planes are situated in anatomical anteroposterior and lateral oblique direction at 25 degrees to each other. Due to the three-dimensional distal locking features, which offer the option to insert ASLS screws, distal diaphyseal fractures can also be addressed with antegrade nailing.
In comparison to previous implants, the MultiLoc nail offers clear advantages for stable fixation, especially of complex fractures like combined proximal and diaphyseal fractures and proximal humeral fractures extending into the diaphysis. Based on surgeon opinions, the compression option could also be advantageous in the management of nonunions and situations with delayed fracture healing.
Case 1: AO 12C1 fracture following fall (Case provided by Stefaan Nijs, Leuven, Belgium)
A 54-year-old woman, and otherwise healthy patient, fell during her holidays and sustained an AO 12C1 fracture (Fig 1). There was no major soft tissue trauma. Other lesions: avulsion at the 5th metatarsal base, and concussion.
Surgery took place on day 9 after the accident. The patient left the hospital the day after surgery.
Case 2: Staircase fall (Case provided by Markus Wambacher, Innsbruck, Austria)
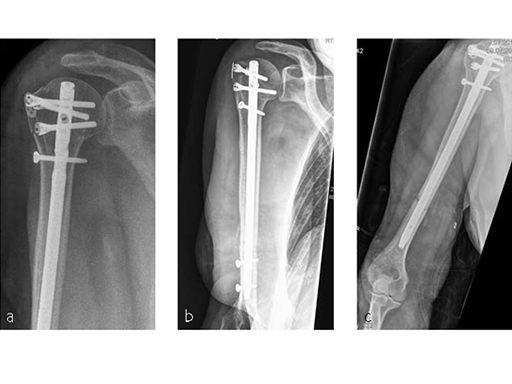
Following a fall downstairs, a 70-year-old woman sustained a head injury with intracerebral and subdural haematoma, as well as a complex fracture of the right humerus, representing a minimal displaced proximal and an oblique fracture in the distal part of the humerus (Fig 3).
After neurosurgical intervention, surgery of the humerus was planned 10 days after the index trauma. The patient was still at the neurological intensive care unit and a preoperative clinical examination of the patient, regarding radial nerve palsy, was not possible. Therefore, a surgical revision with exploration of the radial nerve and an osteosythesis of the humerus using a long MultiLoc Humeral Nail was indicated.
The patient was operated on in beach chair position. For the exploration of the radial nerve, a limited anterolateral approach was used. The nerve was mobilized and retracted laterally. An anterolateral approach to the proximal humerus was performed. The supraspinatus showed a small acute rupture without retraction. The supraspinatus tendon was split to get access to the insertion area on the humeral head. A 270 mm long MultiLock Humeral Nail of 8.5 mm diameter was inserted under visual and x-ray control to the desired endpoint. Reduction of both the proximal and the distal humerus fracture was anatomical. In the lateral view there was a small gap, and it was decided to apply compression after distal locking (Fig 4). Proximally, three MultiLoc screws were inserted and a 2 mm end cap was placed. Finally, the supraspinatus rupture was reconstructed with transosseous sutures and secured with an augmentation plate. The posterior greater tuberosity fracture was secured with Fiber Wire to the MultiLoc screws. Figure 5 illustrates the definitive fixation.
Postoperatively, no sling was used because the patient stayed in medically induced coma.
A new proximal humeral nail with multiple screw placement option
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.