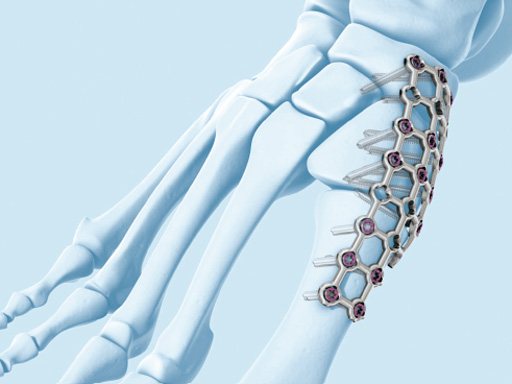
VA-LCP Forefoot/Midfoot set
Andrew Sands, Per-Henrik Agren, Juan Gerstner, Leslie Grujic, Ian Winson
Rigid fixation in the foot has recently taken an evolutionary step. The VA-LCP forefoot/midfoot set represents a leap of technology which allows the adaptive application of fixation to meet virtually any need in fracture treatment or reconstruction.
The variable angle locking screws (2.4 or 2.7 mm) can be placed and locked 15 from perpendicular in any plane. The overall plane is 30. This allows fixed angle fixation in juxtaposition to joints which is particularly important in the midfoot, where tolerances are small and joint contours vary. In addition, screws can be converged, diverged, or staggered optimizing the stability of the construct.
The variable angle locking compression forefoot/midfoot set is a revolutionary development in the treatment of reconstruction and fracture care. These implants provide a means of tailoring fixation to virtually any fracture or reconstructive surgical plan. In the short time since its release, additional applications for these implants have been found. The use of this set can facilitate the precise tailoring of fixation to meet any problem the surgeon may face. The authors feel confident that the use of these implants in conjunction with meticulous soft-tissue technique, respect for the blood supply, and early motion will improve the functional outcome of patients.
The implants are general and specific. Plate design took into consideration the specific anatomical entities, such as the talar neck, navicular, cuboid, first tarsometatarsal (TMT), and metatarsophalangeal (MTP) plates. Others, the X plate, T, L, and U plates, the straight plate, and the clover can be placed where a need exists. These designs can be adapted to virtually any fracture or reconstructive need in the foot. An example is the fixation of tarsal navicular fractures where the contour of the talonaviclar joint requires meticulous screw placement.
Among the specific plates, the first MTP arthrodesis plate is available in left and right, and 0, 5, or 10 of dorsiflexion. This plate can be used with a ball-and-socket reaming set allowing precise positioning while maximizing apposition of the subchondral surfaces. Additionally it can be used with or without lag screw augmentation depending on the individual case. Another design consideration was the management of bone loss and the need for interposition bone graft.
The plates designed for use at the TMT joints provide rigid fixation and stability and generate compression without the need for lag screw fixation. This is of particular benefit in patients whose bone quality may make lag screw fixation difficult, who risk fracture or breakout of the screws. In these cases the locking compression plates and their valuable angled locked screw provide resistance to shear and bending forces which might otherwise compromise lag screw fixation.
In the treatment of fractures, the navicular and cuboid plates have proved very useful. The navicular plate can be positioned from plantarmedial to dorsolateral depending on the fracture pattern. Fracture of the navicular demonstrates the greatest application of variable angle screw placement. Screw placement can be optimized about the concavity of the navicular without violating the subchondral bone on either side. Of course, care must be taken to minimize soft tissue undermining maintenance of blood supply, but this too is aided by the variability of screw placement.
Similarly, the cuboid plate is designed to efficiently restore length and height of this bone which is vital in the treatment of injury compromising the lateral column of the foot. Again, the utility of variable angle screw placement should not be understated in this application. Screw placement can be varied, adhering to the contour of the calcaneocuboid and TMT joint surfaces optimizing the integrity of the construct.
The mesh plate, originally designed to address traumafractures and dislocations/subluxationsof the intertarsal region from Chopart to Lisfranc, can be cut and contoured to stabilize the midfoot medially, laterally, or in combination. Therefore, it is an ideal implant in case of bone loss or an adjunct in the reconstruction of neuropathic collapse.
Another new concept that is introduced in the VA set is the opening wedge implants and tools.In deformity correction many things can be achieved with angular correction. The opening wedge plates and the opening wedge-distractor gauge make it possible to perform corrections with a positive distracting correction without bonegrafting. The distractor gauge is used in a transverse osteotomy to open it up and make a correction that is measured and then secured with a plate with a metal wedge, spreading the cortices under the securing plate. Possible indications could be metatarsal and tarsal corrections where shortening is not desired.
Compression is afford ed by the use of a compressive forceps and beaded, threaded pins. The plates possess a pin-slot at one end and a corresponding pin-hole in the other. The technique consists of fixing the plate to bone using a beaded pin through the hole and engaging the opposite cortex. After manual compression is applied to maximize the compressive effect, a second beaded, threaded pin is placed through the slot, again, engaging the opposite cortex. The ratcheted compression forceps is then applied and by virtue of the slot, the two surfaces are translated together. The slotted side of the plate is now fixed with cortex or locking screws, depending on the need and preference of the surgeon. If a lag screw is used first as in standard technique, then the plate must be placed in neutralization without compression. If the plate is used without lag screws, the controlled compression (ball squeezer) can aid in achieving compression across the fusion site. The other screw holes can then be filled with locking screws to achieve a fixed angle arrangement.
This technique allows for uniform compression across a joint surface. In certain cases, a second pair of beaded pins can be placed outside the plate to generate greater compression or to distribute force more evenly.
Applying compression this way may preclude the need for lag screw fixation that might otherwise require a separate or larger incision, more dissection, or undermining of tissue.
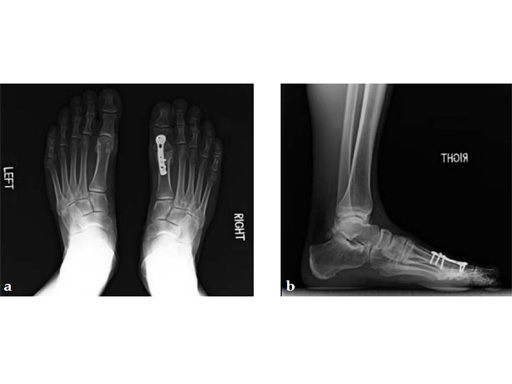
Case 1: First MP fusion VA-LCP
A 57-year-old woman has suffered rheumatoid arthritis for several years. She presented with pain and deformity in the left forefoot moreso than in the right. Clinical examination reveals severe hallux valgus deformity and dislocation of MP joints 11 through V, with synovitis.
Case provided by Juan Bernardo Gerstner, Cali, Columbia
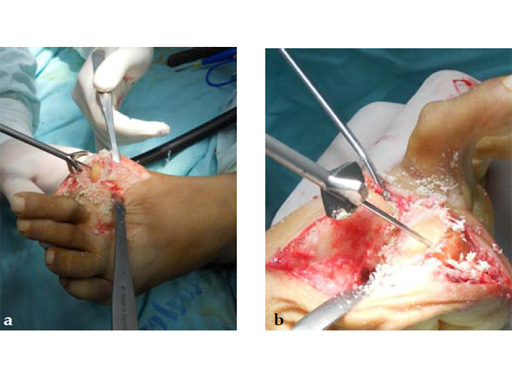
A dorsal transtendinous approach was used and reaming of the first MT head and basal articular surface of the proximal phalanx was performed with the new reamers (see Fig. 3a-b).
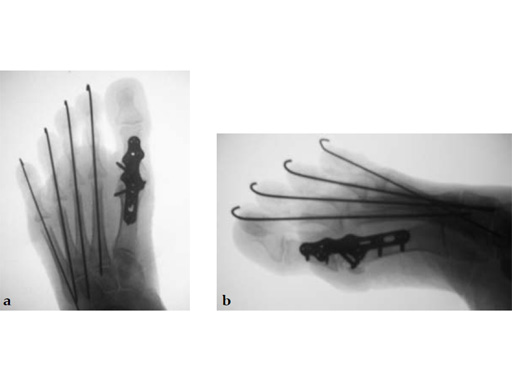
A left MP fusion was performed as well as a II to V MT head resection arthroplasty, and fixed with K-wires for 4 weeks (see Fig. 4a-b). The patient was weight bearing immediately with wooden shoes and K-wires were removed 4 weeks postoperatively.
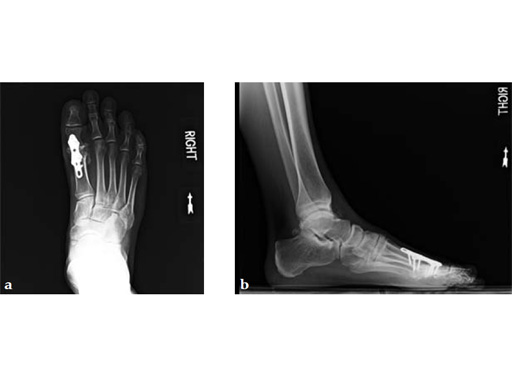
Case 2: First MTP fusion plate
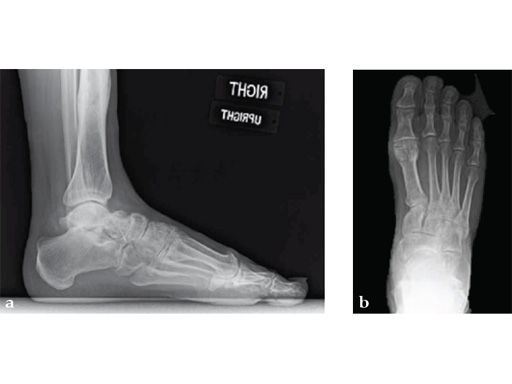
A 38-year-old man presented for opinion after two attempts to fuse the big toe MTP joint. The AP view is significant for luscency at the joint line. The lateral view is notable for loosening of the hardware and malposition because of the dorsiflexion built in to the precontoured implant. Revision was planned using a 0 variable angle locking/compression hallux MTP plate.
Case provided by Michael Castro, Scottsdale, Arizona
At 10 weeks postoperatively (see Fig. 2ab) the patient had no pain with weight bearing. The lateral view demonstrates improved position of the toe using a 0angle plate.
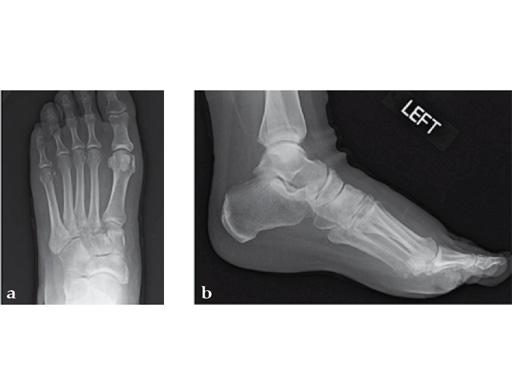
Case 3: First TMT fusion plate
A 48-year-old woman, with hallus valgus and hypermobile medial column, also resulting in pes plano abductovalgus (flatfoot).
Case provided by Andrew Sands, New York, New York, USA
Surgery consisted of first TMT and intertarsal corrective osteotomy plus fusion with movement of the first MT lateral and plantar. This corrects the hallus valgus as well as the PPAV (and stabilizes the medial column).
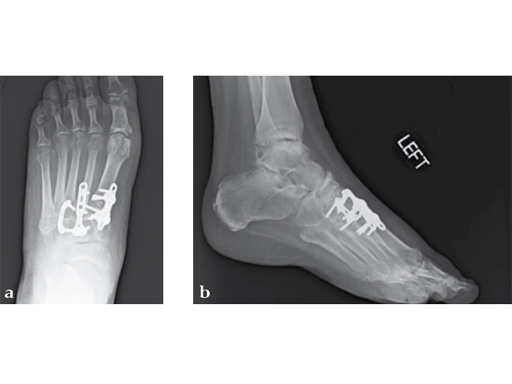
Case 4: First TMT fusion plate
A 60-year-old woman with pes plano abductovalgus (flatfoot deformity).
Case provided by Andrew Sands, New York, New York, USA
The patient was treated by headless compression screw 6.5 tuber osteotomy, TMT plantarflexing osteotomy, and first TMT fusion a plate.
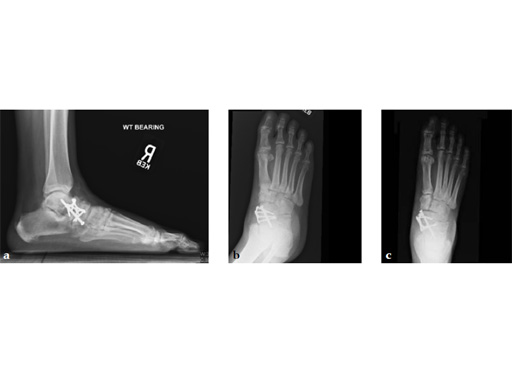
Case 5: First TMT, straight fusion and TMT fusion plates
A 46-year-old obese woman with coronary artery disease had sustained a Lisfranc injury while performing an exercise program. She was unable to weight bear and used an electric scooter.
In an effort to restore her ability to exercise and taking into consideration her body weight and upper extremity weakness, a decision was made to use the variable angle locking compression plate. These postoperative x-rays were obtained at 3 months, one month after beginning weight bearing. The patients pain was reduced and she was able to resume a progressive exercise program after 4 months following surgery.
Case provided by Michael Castro, Scottsdale, Arizona
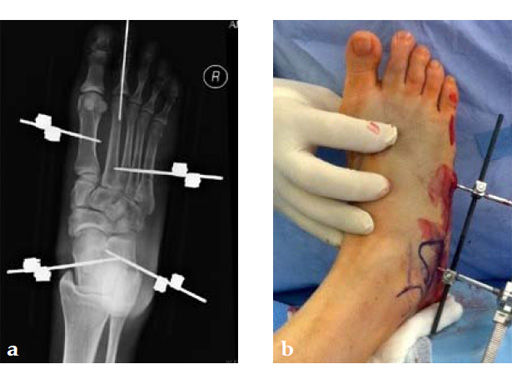
Case 6: VA -locking mesh plate
A 46-year-old female pedestrian was run over. Her foot was crushed by a car. It was a closed injury. She had no other bodily injuries and no medical problems. She sustained massive swelling and shear dorsal soft-tissue injury.
Case provided by Andrew Sands, New York, New York, USA
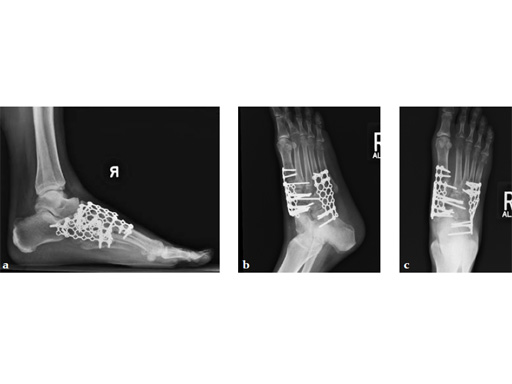
Case 7: VA -locking X-plate
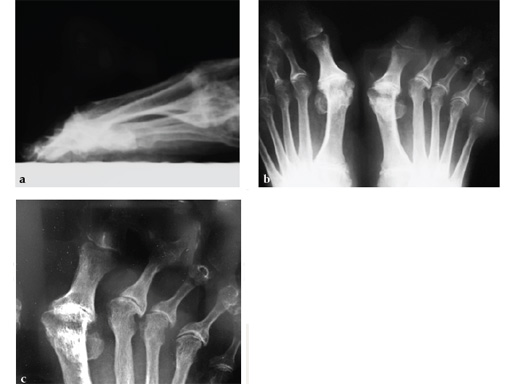
A 49-year-old woman had extreme pain in the talonavicular joint.
Case provided by Andrew Sands, New York, New York, USA
As isolated fusion of the talonavicular joint is often hard to achieve, a 4.0 mm lag screw a plus X-plate was used (see Fig. 2a-c).
Fusion of the talonavicular joint while saving the rest of the hindfoot complex motion was achieved (see Fig. 4a-c).
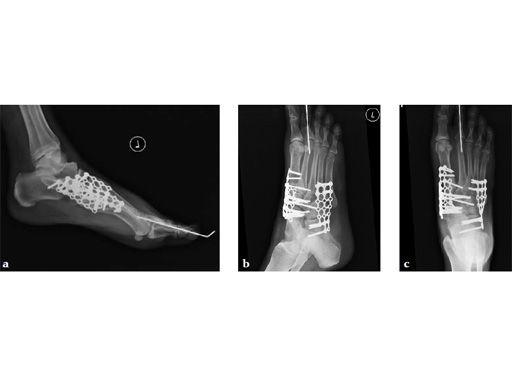
Case 8: VA -locking X-plate
A 38-year-old man fell from a 7-foot height while at work. The patient was seen at an urgent care facility and diagnosed with an ankle sprain. He was placed in a stirrup brace and instructed to bear weight as tolerated.
Case provided by Michael Castro, Scottsdale, Arizona
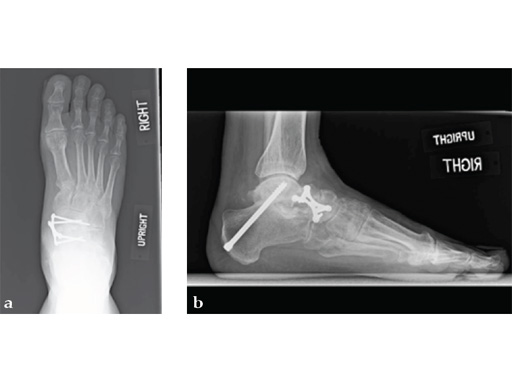
After 4 months the patient presented for a second opinion. His complaint was pain to the lateral column and subtalar joint. The preoperative lateral x-ray is notable for a malunited talar neck fracture with subluxation of the subtalar joint. The disproportion of the medial and lateral columns and a cavovarus position of the foot are seen on both the AP and lateral views. The degenerative changes at both the talonavicular and subtalar joints are significant.
The patient was treated with arthrodesis of the talonavicular and subtalar joints. The compression/ distraction device was used to restore the length of the medial column. The articular surface of the subtalar joint was prepared arthroscopically. The talonavicular joint was debrided then packed with a tricalcium matrix. Length was maintained using a locking X-plate. The subtalar joint was then fixed with a 6.5 mm headless compression screw.
The patient returned to work 3 months after surgery. He wears an ankle brace when on uneven surfaces. His lateral column and subtalar pain have resolved.
New Treatment Concepts in Forefoot and Midfoot
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.