USS Fracture MIS
Thoracolumbar fractures predominately result from motor vehicle accidents, work related injuries, and an increased incidence of fractures from the aging osteoporotic population. In many parts of the world, the golden standard of care for unstable spine fractures involves stabilization with a Schanz pedicle screw-clamp system (USS Fracture).
Over the years, the trend to minimize iatrogenic trauma during spine fracture surgery has been supported by the excellent clinical outcomes of patients and the development of minimally invasive stabilization systems. Yet, the currently available minimal invasive stabilization systems have, so far, not been dedicated to the treatment of spine fractures according to AO principles.
Until now surgeons often had to make compromises in the minimally invasive surgical treatment of spine fractures because the available systems allowed only very limited active kyphosis correction and distraction. Instead, most systems relied on an indirect correction of the deformity by positioning the patient on the operating table. Hence, they were only able to stabilize the correction, which was achieved by closed reduction.
With USS Fracture MIS, there is now the opportunity to bridge this gap and address the treatment of spine fractures in a minimally invasive way in accordance with acknowledged AO principles.
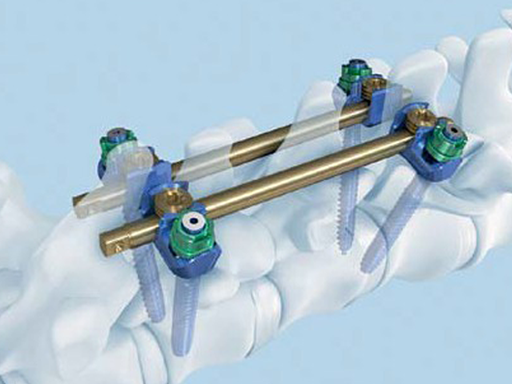
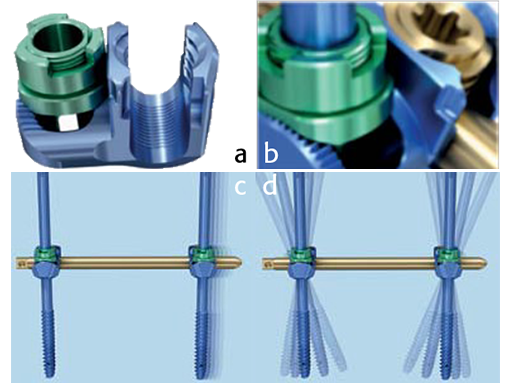
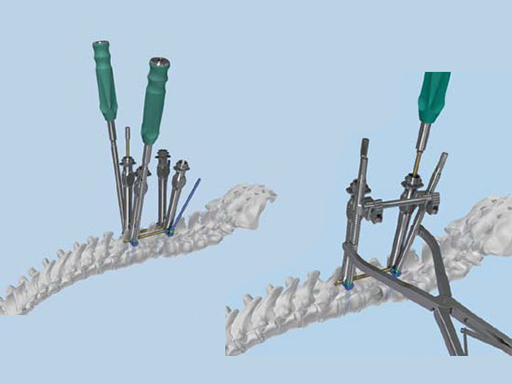
The USS Fracture MIS system makes the AO fracture treatment philosophy applicable for the first time in a minimally invasive way by enabling an active repositioning of fractures through an independent, nearly stepless correction of the deformity based on distraction and lordosis. USS Fracture MIS has a specialized clamp with two independent locking mechanisms (MIS fracture clamp), which allow for control of sagittal alignment ( 20) as well as height restoration.
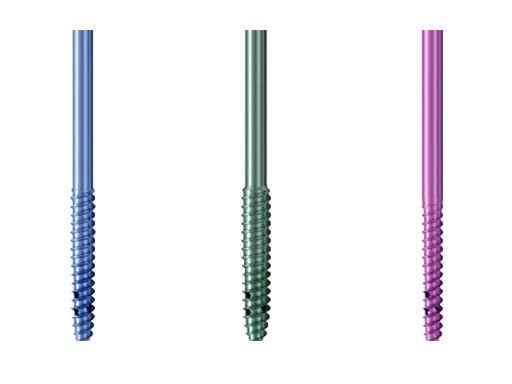
Together with the perforated Schanz screws, it delivers a unique solution for a broad range of indications.
The USS Fracture MIS system is appropriate for a range of clinical conditions including fractures, tumours, degenerative disc disease, post traumatic deformities, and spondylolisthesis of the posterior thoracolumbar spine.
Contra indications for USS Fracture MIS as a stand-alone are: fractures and tumors with severe anterior vertebral body destruction, where an additional anterior column reconstruction is required. Additionally it should not be used in severe osteoporosis without augmentation. However, in Europe, USS Fracture MIS Perforated complements USS Fracture MIS and addresses the growing population of osteoporotic patients requiring fracture procedures by offering perforated Schanz screws that allow additional cement augmentation.
Case: minimally invasive fracture treatment for an incomplete burst fracture
Case provided by Frank Kandziora, Frankfurt, Germany
A 50-year-old female patient fell down the stairs, suffering severe back pain. The initial examination showed pain at the thoracolumbar junction and no neurologic deficit.
Preoperative analysis
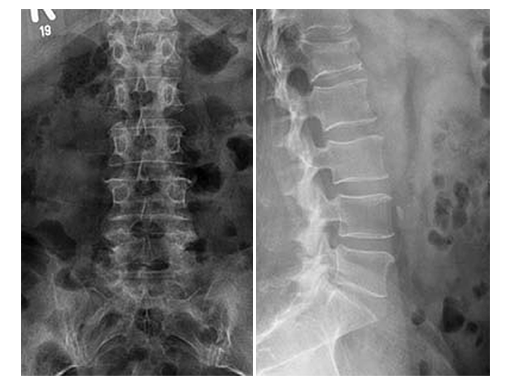
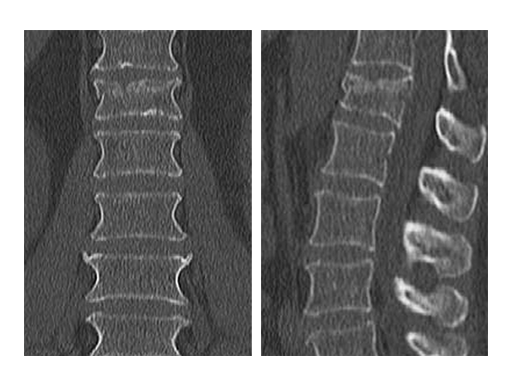
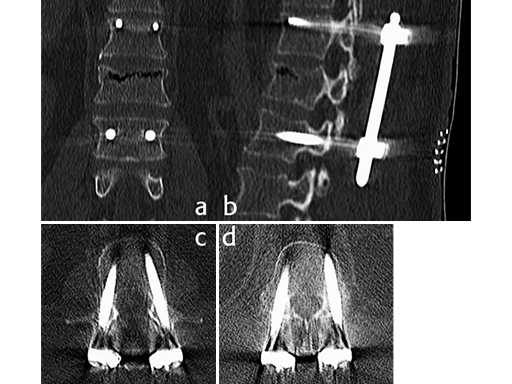
X-rays and CT scans were performed for preoperative analysis, definition of the fracture type and surgical pre-op planning.
The lateral x-ray and CT scans showed a typical wedge deformity of the fractured vertebral body (L1). The fracture included the cranial endplate as well as the anterior and posterior wall.
Additionally, a MRI scan was performed to analyze the integrity of the soft tissue in detail. The lateral MRI clearly showed a ruptured intervertebral disc at the level T12/L1.
Based on the Magerl Classification [1], the final classification of the fracture concluded in AO Type A 3.1.1. This fracture type is also referred to as an instable incomplete burst fracture including posterior wall involvement.
Surgical plan
The incomplete burst fracture associated with the destruction of the intervertebral disc resulted in the planning of a two staged approach. In a first immediate surgery, the unstable fracture was stabilized by posterior percutaneous AP and lateral preoperative CT scans. fixation. In a second surgery, a cranial hemi-vertebrectomy was performed. Reconstruction was done using an autologous iliac crest bone graft and a plate to achieve a mono-segmental fusion.
First surgery Intraoperative
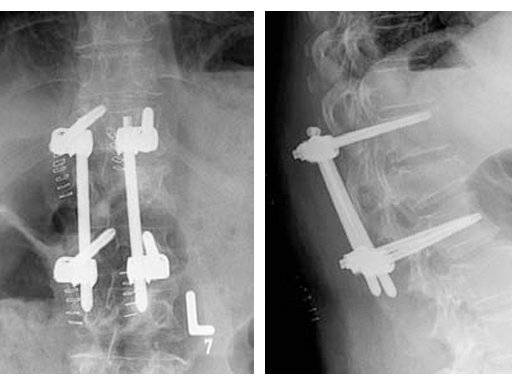
Based on the preoperative analysis and the surgical plan, the patient was positioned supine for the first surgery and the fracture was stabilized with a bridging construct (T12-L2) from posterior. Due to the ruptured disc, an anterior reconstruction of the spine was planned for a later stage surgery. The posterior stabilization was considered to be sufficient to bridge the fracture and time between both surgeries.
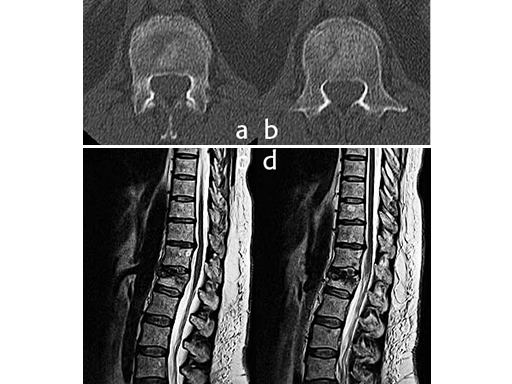
Using the USS Fracture MIS system for the initial stabilization allowed for a minimally invasive approach with intraoperative active reduction of the spinal fracture. The unique design of the fracture clamp allowed for independent correction of the sagittal alignment (Fig a) as well as height readjustment (Fig b).
For this patient, independent lordosis correction, height readjustment, and spinal stabilization were the primary goal of surgery. As percutaneous toploading pedicle screw systems cannot provide independent correction of the flexion-compression deformity, the fracture clamps and Schanz screws of the USS Fracture MIS system were used to overcome this disadvantage.
Due to the minimally invasive approach, the patient experienced less blood loss and muscle trauma compared to the traditional open approach.
Second surgery for anterior column reconstruction
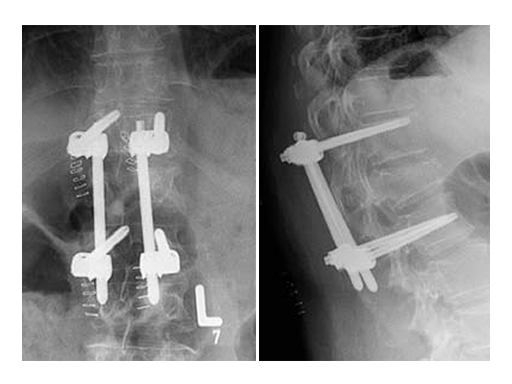
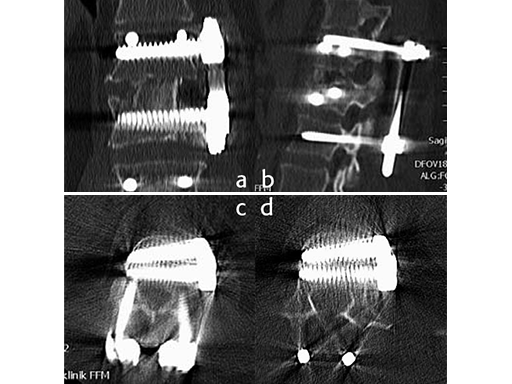
As a result of the ruptured disc and the fractured superior endplate, a hemivertebrectomy was performed and reconstruction was performed using an autologous iliac crest bone graft. To keep the graft in place and to allow for early posterior implant removal, an ArcoFix plate was used, allowing for slight compression as well as final sagittal reconstruction.
The hemivertebrectomy and the placement of the bone graft and ArcoFix plate were performed applying thorascopically assisted surgical technique.
Postoperative follow up
The minimally invasive approach with USS Fracture MIS allowed for this patients fast recovery, and supported earlier discharge. The patient was back home eight days after the second surgery.
References
- Magerl F, Aebi M, Gertzbein SD, et al (1994) A comprehensive classification of thoracic and lumbar injuries, Eur Spine J 3(4):184201
Follow up CT Scans (AP, lateral and coronal) after the second surgery.
Minimal invasive treatment in Thoracolumbar Fractures
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.