MultiLoc Proximal Humeral Nail
Martin Hessmann, Stefaan Nijs
Angular stable plating and nailing are well-established procedures to treat proximal humeral fractures. However, the complication rates of these treatment options remain high, mainly due to the complicated fracture pattern, the complexity of the local anatomy, compromised vascularity after fracture of the humeral head, and poor bone anchorage due to osteoporosis. The MultiLoc Proximal Humeral Nail (MultiLoc PHN) was developed in an effort to improve nailing osteosynthesis stability and thus expand the indications for nailing at the proximal humerus. The new nail is intended for the treatment of fractures of the proximal humerus, including two-part surgical neck fractures, three-part fractures, and four-part fractures.
Design features
Recent clinical studies revealed good clinical results for Xmas tree type intramedullary nailing devices in complex fracture patterns [1]. The stability provided by plate and nail osteosynthesis was analyzed in a biomechanical study [2].
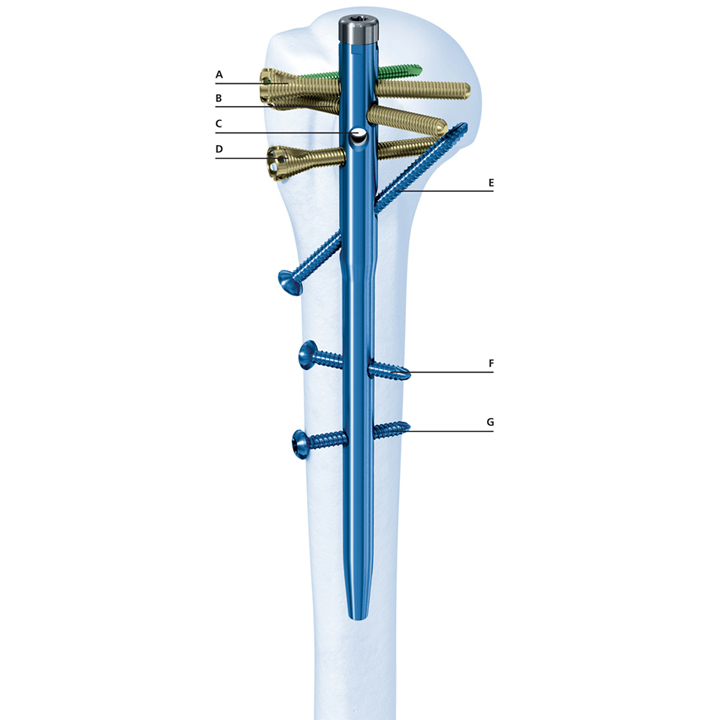
The MultiLoc PHN is a Xmas tree type nail with an innovative screw-in-screw technology, which allows treatment of both simple and complicated fractures (Fig 1). The nail is cannulated and has a straight design to allow for a central nail insertion in line with the medullary canal. The MultiLoc PHN includes four multiplanar and angular stable proximal locking options, one ascending locking option, and two distal locking options.
Angular stability of the proximal locking holes is achieved through a polyethylene inlay with bore holes which are slightly smaller in dimension than the screws. Ascending and distal locking is compatible with 4.0 mm locking screws (nonangular stable) or 4.0 mm angular stable locking system screws (angular stable). The ascending screw is specifically useful in varus type fractures with medial comminution. A biomechanical study showed the improved stability provided by the ascending screw and the MultiLoc screws of the new nail. The 160 mm long left and right cannulated nails are available in diameters of 8.0 mm and 9.5 mm. The diameter of the nail thus can be adapted to the width of the medullary cavity, which is especially useful in elderly patients with osteoporotic bone.
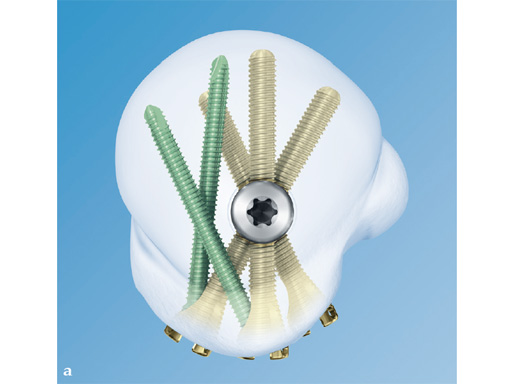
Screw-in-screw technology
Through the screw heads of the MultiLoc screws (countersinkable head design with a locking inner thread in the screw head, four suture holes, and blunt screw tip), additional 3.5 mm locking screws may be inserted into the humeral head to enhance stability (Fig 2). This screw versatility is beneficial to address the various fragments in complex fractures and is thus a clear advantage over the expert humeral nailing system or the unreamed humeral nail/PHN system. The design of the MultiLoc PHN allows the 3.5 mm locking screws to be inserted into the densest bone in the humeral head, which is posteromedial [3].
Long MultiLoc Nail
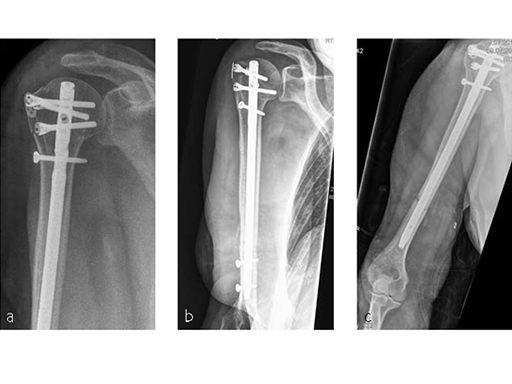
A long version of the MultiLoc nail (Fig 3) was developed in order to treat such issues as fractures of the humeral diaphysis, fractures of the proximal humerus with diaphyseal extension, as well as combined fractures of the proximal humerus and the humeral diaphysis. This longer version nail, which is available in 7.0 mm and 8.5 mm diameters and in lengths from 180 mm to 315 mm, completes the MultiLoc Humeral Nailing System creating a single comprehensive system for all fractures amenable for nailing.
References
1 Mittlmeier TW, Stedtfeld HW, Ewert A, et al (2003) Stabilization of proximal humeral fractures with an angular and sliding stable antegrade locking nail (Targon PHN). J Bone Joint Surg Am; 85-A(Suppl.4):136-146.
2 Hessmann MH, Hansen WS, Krummenauer F, et al (2005) Locked plate fixation and intramedullary nailing for proximal humerus fractures: a biomechanical evaluation. J Trauma; 58(6):1194-1201.
3 Lill H, Hepp P, Gowin W, et al (2002) [Age- and gender-related distribution of bone mineral density and mechanical properties of the proximal humerus.] Rofo 174(12):1544-1550. German.
AO Research Institute: Biomechanical Evaluation of Three Different Locking Options Using MultiLoc PHN for Intramedullary Nailing of Proximal Humeral Fractures in a Three-Part Fracture In Vitro Model
Objective
The treatment of unstable three- and four-part proximal humeral fractures remains challenging. Clinical outcomes using standard osteosynthesis treatments are not yet satisfactory, especially in osteoporotic bone. That is why optimization of the implant design accounting for good quality and osteoporotic bone is of major interest. An extended version of MultiLoc PHN intramedullary nail was recently developed for simple and complex fractures of the proximal humerus. In addition to the possibility for multiplanar distal fixation with two angle-stable locking screws (ASLS) and three proximal humeral head screws (standard), this nail introduces the screw-in-screw concept including one additional locking screw in each of the proximal screws. Later on, a calcar screw starting in the lateral cortex of the shaft and ending in the cancellous bone of the humeral head calcar region can be optionally purchased. The purpose of these design adaptations is to improve implant anchoring to bone and support the head fragment, thereby increasing construct stability.
The aim of this biomechanical study was to investigate three different locking options using MultiLoc PHN (short) for intramedullary nailing of proximal humeral fractures, and answer the question whether its design adaptations with two additional screw-in-screw and a calcar screw provide a better interfragmentary stability compared to the standard version with three proximal screws in an established anatomical specimen biomechanical three-part proximal humeral fracture model.
Materials/methods
Eighteen fresh frozen anatomical specimen humeri (-20°C, 9 female and 9 male donors, mean age 74.8, range 50-96), dissected from soft tissue, excluding the supra- and infraspinatus tendons, were randomly assigned to three study groups and instrumented with either standard, two additional screw-in-screw, or two screw-in-screw plus one additional calcar screw option according to predefined steps.
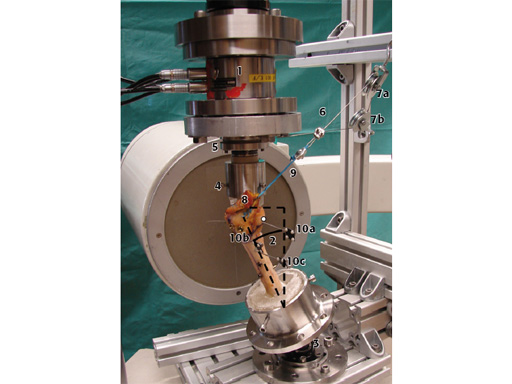
A recently introduced biomechanical in vitro testing model for three-part proximal humeral fractures simulated with a transversal wedge and a sagittal cut, including cyclic axial loading with increasing peak load (0.05 N/cycle, 2 Hz) and simultaneous pulling forces at the rotator cuff was used (Fig 4) [1]. Interfragmentary motions were analyzed using motion tracking. Statistical differences between the study groups were detected by ANOVA and Bonferroni PostHoc tests. Significance level was set to P > .05.
Results
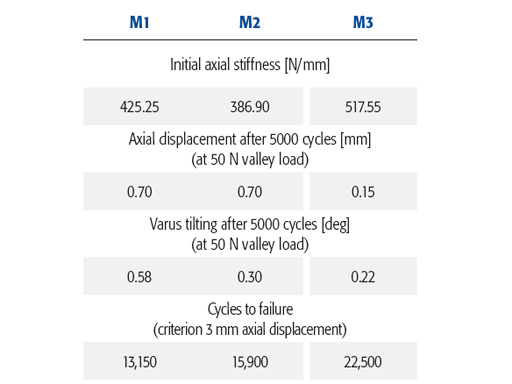
The MultiLoc PHN with a calcar screw and two screw-in-screw showed a superior initial axial construct stiffness, minimal axial displacement, reflecting highest head stability against migration along the nail, and highest number of cycles to failure during the cyclic test (Table 1). In addition, both options with two screw-in-screw aiming volumes in the posteromedial humeral part with better bone quality were superior with regard to varus tilting of the humeral head, compared to the standard configuration.
Conclusion
All three MultiLoc PHN locking options performed very well biomechanically compared to other existing implants for the same indications and would be a good choice for treatment of proximal humeral fractures. The configuration with a calcar screw and two screw-in-screw was superior in most aspects (compared to the other two configurations) while both options with two screw-in-screw showed better behavior with regard to varus collapse, confirming that the screw-in-screw concept can be used to increase osteosynthesis stability in poor bone quality.
References
1 Brianza S, Plecko M, Gueorguiev B, et al (2010) Biomechanical evaluation of a new fixation technique for internal fixation of three-part proximal humerus fractures in a novel cadaveric model. Clin Biomech; 25:886-892.
Case provided by Martin H Hessmann, Fulda, Germany
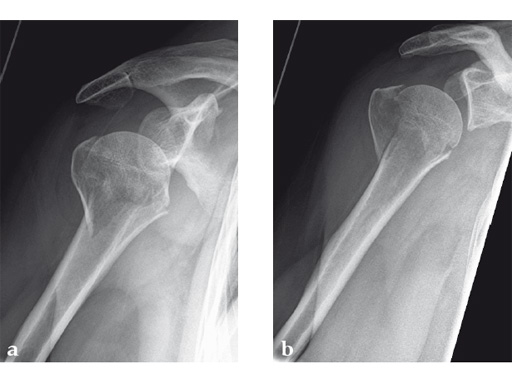
Case 1: A three-part valgus impacted fracture of the proximal humerus in a 47-year-old woman.
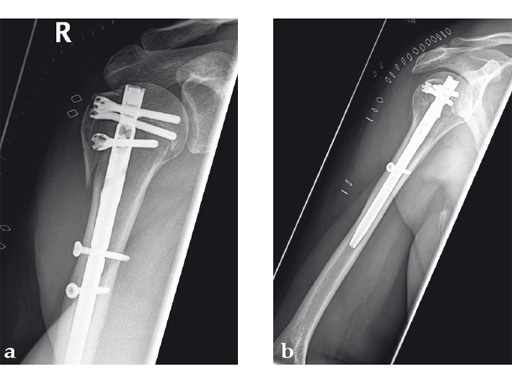
Case provided by Stefaan Nijs, Leuven, Belgium
Case 2: Three-part valgus displaced fracture of the proximal humerus in a 63-year-old man.
The tuberosities have been reduced and fixed using intertubercular sutures (Fig 4). To reconstruct the medial support a calcar screw has been used. This determines the height of the nail. Therefore a 1 cm end cap has been used to get support for the proximal end of the nail in the part of the bone with the best bone quality.
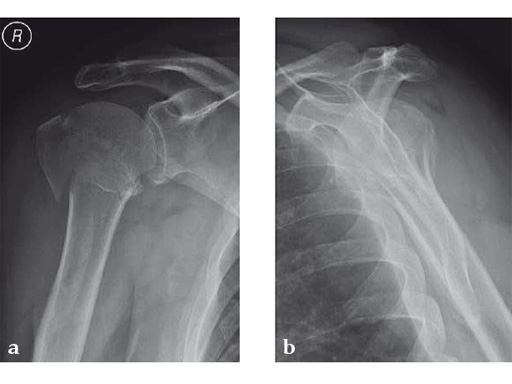
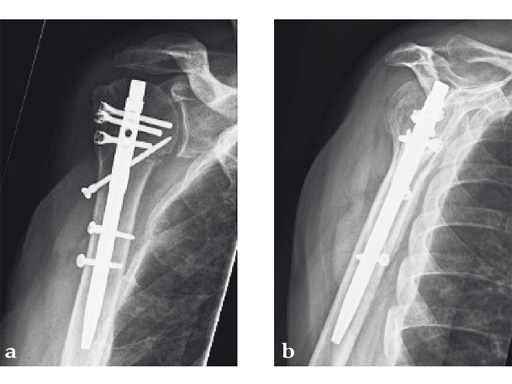
Case provided by Stefaan Nijs, Leuven, Belgium
Case 3: Three-part varus displaced fracture with head-split component in a 60-year-old woman.
This case is an illustration of the application of the new nail in a borderline indication. Head-split fractures remain a challenge whatever implant is used for fixation.
Case provided by Stefaan Nijs, Leuven, Belgium
Case 4: AO 12C1 fracture following fall
A 54-year-old woman, and otherwise healthy patient, fell during her holidays and sustained an AO 12C1 fracture. There was no major soft tissue trauma. Other lesions: avulsion at the 5th metatarsal base, and concussion. Surgery took place on day 9 after the accident. The patient left the hospital the day after surgery.
Case provided by Markus Wambacher, Innsbruck, Austria
Case 5: Staircase fall
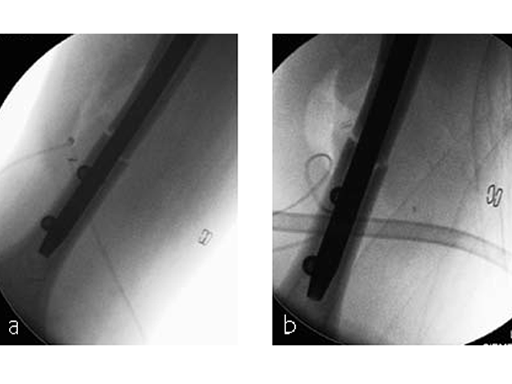
Following a fall downstairs, a 70-year-old woman sustained a head injury with intracerebral and subdural haematoma, as well as a complex fracture of the right humerus, representing a minimal displaced proximal and an oblique fracture in the distal part of the humerus (Fig 11).
After neurosurgical intervention, surgery of the humerus was planned 10 days after the index trauma. The patient was still at the neurological intensive care unit and a preoperative clinical examination of the patient, regarding radial nerve palsy, was not possible. Therefore, a surgical revision with exploration of the radial nerve and an osteosythesis of the humerus using a long MultiLoc Humeral Nail was indicated.
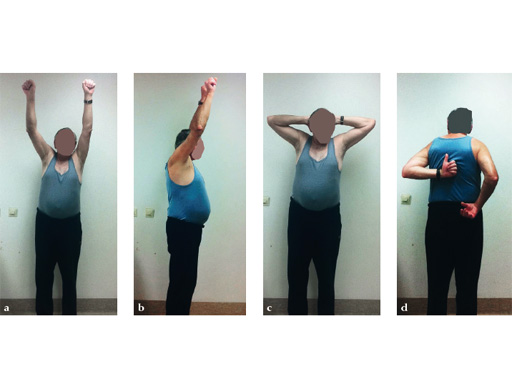
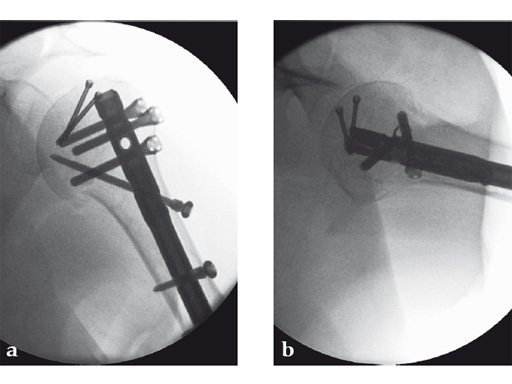
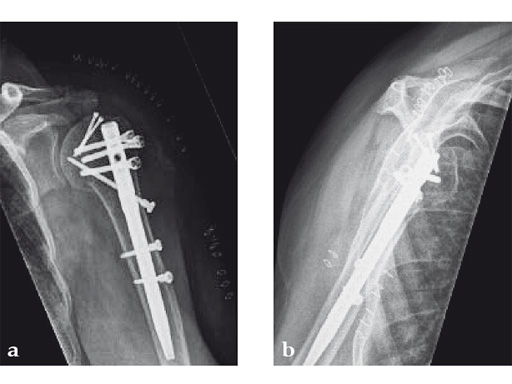
The patient was operated on in beach chair position. For the exploration of the radial nerve, a limited anterolateral approach was used. The nerve was mobilized and retracted laterally. An anterolateral approach to the proximal humerus was performed. The supraspinatus showed a small acute rupture without retraction. The supraspinatus tendon was split to get access to the insertion area on the humeral head. A 270 mm long MultiLoc Humeral Nail of 8.5 mm diameter was inserted under visual and x-ray control to the desired endpoint. Reduction of both the proximal and the distal humerus fracture was anatomical. In the lateral view there was a small gap, and it was decided to apply compression after distal locking (Fig 12). Proximally, three MultiLoc screws were inserted and a 2 mm end cap was placed. Finally, the supraspinatus rupture was reconstructed with transosseous sutures and secured with an augmentation plate. The posterior greater tuberosity fracture was secured with Fiber Wire to the MultiLoc screws. Fig 13 illustrates the definitive fixation.
Postoperatively, no sling was used because the patient stayed in medically induced coma.
The Multiloc Nail - A new proximal humeral nail with multiple screw placement options
Latest advances in IM nailing techniques
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.