MidShaft Clavicle Fractures: Change of Paradigms
Fractures of the clavicle are common injuries, representing 35% of all fractures and occurring with an incidence of 64 per 100,000 [1]. They are seen in up to 45% of all injuries of the shoulder girdle and are located in the midshaft area in approximately 80% of cases [2].
Midshaft clavicle fractures occur either isolated, or in combination with other injuries. Until recently, the nonoperative treatment was considered the gold standard, avoiding surgery-specific risks. Therefore midshaft clavicle fractures are either redressed in a figure-of-eightbandage for several weeks or immobilized in an arm sling (eg, Gilchrist bandage). Two prospective randomized studies comparing both methods across 234 participants in total were not able to detect significant differences in functional or other outcome parameters reported for either trial [3].
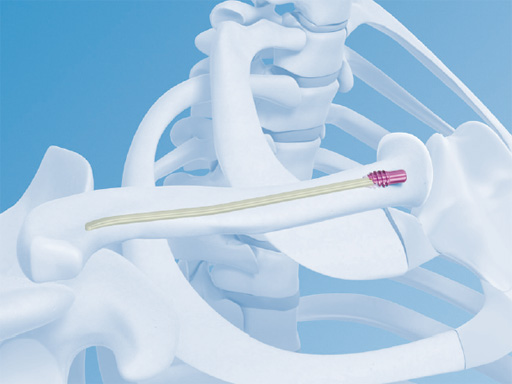
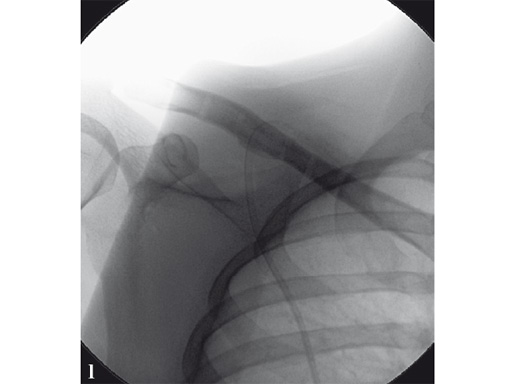
Fig 1 3.5 mm LCP superior clavicle with extension/3.5 mm LCP superior anterior clavicle with extension (short versions of both plates are identical).
The main purpose of these bandages is initial pain relief. Fracture reduction is not usually performed. The fractures typically heal in the preexisting deformity, in which remodeling can be observed to various extents. However, often a shortening of the affected clavicle can be observed. This results in a shift of the scapula with a change in tensioning of the affected shoulder girdle muscles. Healing with a shortening of 2 cm or more shows a clinically significant deterioration of results [47]. In addition, the development of a nonunion is well known and not uncommon after nonoperative treatment. The incidence depends on the type of fracture and ranges from 6 to 15% [4]. Khan was able to determine a calculated probability of nonunion at 24 weeks after clavicle shaft fractures depending on age, sex, comminution, and displacement [8]. Females over 70 years of age with displaced and comminuted fractures have the worst prognoses with an estimated likelihood of nonunion at 49%.
Previously just the following, rare indications for surgery were generally accepted:
- Risk of fracture perforation
- Open fractures
- Neurovascular injuries
- Additional blunt chest trauma with ipsilateral rip fractures
- Shortening of more than 2 cm
In contrast to this, several studies with a high level of evidence have recently been published, and are able to show that surgical treatment has significantly better results [7, 916]. One major advantage of surgery is the ability to achieve and maintain reduction of the fracture to avoid nonunion and shortening. But even if there is just a slight displacement of the fracture, stabilization with a plate or nail provides both improved pain relief and quicker return to activities of daily living. Therefore, it now seems justified to extend the range of indications for surgery.
The Canadian Orthopaedic Trauma Society published a prospective randomized multicenter trial in 2007 [10]. They compared nonoperative treatment with plate fixation of displaced midshaft clavicle fractures of 132 cases. At 1-year follow-up the clinical results in terms of Constant and DASH scores improved significantly at all time-points. The mean time of radiographic union was 16.4 weeks after surgery with a lower rate of malunion and nonunion compared with nonoperative treatment. Compared to the nonoperative group, patients treated with plate osteosynthesis were significantly more likely to be satisfied with the appearance and function of the shoulder.
Meanwhile, further prospective randomized studies have been published which also demonstrate the superiority of plate fixation of midshaft clavicle fractures compared to nonoperative treatment [7, 11]. Minimally invasive intramedullary fixation methods were also able to show excellent results superior to nonoperative treatment with high level-1 evidence [7, 9, 1113]. However, in contrast to plate fixation the range of indications is reduced and has to be respected to avoid known complications, such as telescoping, secondary implant migration, and secondary loss of reduction. In particular, complications are frequently seen in comminuted fractures. They should be treated by plate fixation. In order to extend their spectrum of indications, nailing systems with angular stability are being developed, since the so-called end cap is not sufficient to stabilize these fractures.
Using plate fixation angular stable systems prevail nowadays. They provide both biomechanical and clinically superior results. At present, various precontoured plates are available. At first glance they seem to be user-friendly since intraoperative bending of the implants according to the shape of the clavicle seems to be less often necessary. In addition, it is beneficial to have a template in multifragmentary fracture situations to allow reduction of the fragments against the plate. The clavicle has a complex three-dimensional structure with high variability [17, 18]. Consequently, it is not easy to fix all clavicles with just one plate shape, the plates may require bending adjustments in some cases.
There is no evidence currently available as to whether the superior, anterior, anteroinferior, or anterosuperior placement is clinically more favorable. Each position has different advantages and disadvantages in terms of its biomechanics, the interference with muscle attachments, the risk of injury of neurovascular structures during placement of angular stable screws, and prominence of plate position requiring later implant removal.
Recently published hints demonstrate that unicortical fixation using precontoured plates and locking screws has a similar biomechanical profile to gold standard nonlocked bicortical screws in cyclic axial compression and load to failure [19]. This may be a factor in lowering the risk and incidence of iatrogenic neurovascular structural damage while drilling, and may also result in lower refracture rates after implant removal. Especially in the midshaft area these structures are very close to the clavicle, resulting in a tip contact of screws in up to 20% of cases [2022].
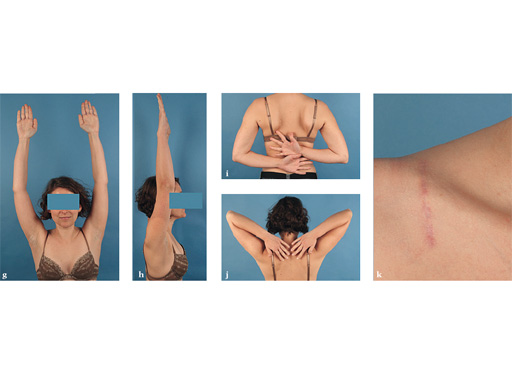
Synthes offers a variety of anatomical precontoured plates: the superior, anterosuperior, and anterior clavicle plates. The anterosuperior clavicle plates are also offered with a so-called lateral extension accepting insertion of six 2.7 mm-head locking screws. This also helps to extend the range of indications for even lateral comminuted clavicle fractures. Open reduction and plate fixation can be classically performed via a sabre-cut incision. Alternatively a minimally invasive approach can be used very nicely and is recommended by the authors. The 3.5 mm clavicle hook LCP and the titanium elastic nail complete the repertoire. It is therefore possible to address every midshaft clavicle fracture individually.
References
1 Postacchini F, Gumina S, de Santis P, et al (2002). Epidemiology of clavicle fractures. J Shoulder Elbow Surg; 11(5):452456.
2 Schiffer G, Faymonville C, Skouras E, et al (2010) Midclavicular fracture: not just a trivial injury: current treatment options. Dtsch Arztebl Int; 107(41):711717.
3 Lenza M, Belloti JC, Andriolo RB, et al (2009) Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst Rev; (2):CD007121.
4 Zlowodzki M, Zelle BA, Cole PA, et al (2005) Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma; 19(7):504507.
5 Lazarides S, Zafiropoulos G (2006) Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elbow Surg; 15(2):191194.
6 Ledger M, Leeks N, Ackland T, et al (2005) Short malunions of the clavicle: an anatomic and functional study. J Shoulder Elbow Surg; 14(4):349354.
7 Judd DB, Pallis MP, Smith E, et al (2009) Acute operative stabilization versus nonoperative management of clavicle fractures. Am J. Orthop; 38(7):341345.
8 Khan LA, Bradnock TJ, et al (2009) Fractures of the clavicle. J Bone Joint Surg Am; 91(2):447460.
9 Witzel K (2007) [Intramedullary osteosynthesis in fractures of the mid-third of the clavicle in sports traumatology]. Z Orthop Unfall; 145(5):639642. German.
10 Canadian Orthopaedic Trauma Society (2007) Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am; 89(1):110.
11 Smekal V, Irenberger A, Struve P, et al (2009) Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma; 23(2):106112.
12 Duan X, Zhong G, Cen S, et al (2011) Plating versus intramedullary pin or conservative treatment for midshaft fracture of clavicle: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg; Epub ahead of print.
13 Ferran NA, Hodgson P, Vannet N, et al (2010) Locked intramedullary fixation vs plating for displaced and shortened mid-shaft clavicle fractures: a randomized clinical trial. J Shoulder Elbow Surg; 19(6):783789.
14 Kulshrestha V, Roy T, Audige L (2011) Operative versus nonoperative management of displaced midshaft clavicle fractures: a prospective cohort study. J Orthop Trauma; 25(1):3138.
15 Pearson AM, Tosteson AN, Koval KJ, et al (2010) Is surgery for displaced, midshaft clavicle fractures in adults cost-effective? Results based on a multicenter randomized, controlled trial. J Orthop Trauma; 24(7):426433.
16 Lenza M, Belloti JC, Gomes Dos Santos JB, et al (2009) Surgical interventions for treating acute fractures or non-union of the middle third of the clavicle. Cochrane Database Syst Rev; (4):CD007428.
17 Andermahr J, Jubel A, Elsner A, et al (2007) Anatomy of the clavicle and the intramedullary nailing of midclavicular fractures. Clin Anat; 20(1):4856.
18 Daruwalla ZJ, Courtis P, Fitzpatrick C, et al (2010) Anatomic variation of the clavicle: A novel three-dimensional study. Clin Anat; 23(2):199209.
19 Hamman D, Lindsey D, Dragoo J (2011) Biomechanical analysis of bicortical versus unicortical locked plating of mid-clavicular fractures. Arch Orthop Trauma Surg; 131(6):773778.
20 Werner SD, Reed J, Hanson T, et al (2011) Anatomic Relationships After Instrumentation of the Midshaft Clavicle With 3.5-mm Reconstruction Plating: An Anatomic Study. J Orthop Trauma; Epub ahead of print.
21 Sinha A, Edwin J, Sreeharsha B, et al (2011) A radiological study to define safe zones for drilling during plating of clavicle fractures. J Bone Joint Surg Br; 93(9):12471252.
22 Qin D, Zhang Q, Zhang YZ et al (2010) Safe drilling angles and depths for plate-screw fixation of the clavicle: avoidance of inadvertent iatrogenic subclavian neurovascular bundle injury. J Trauma; 69(1):162168.
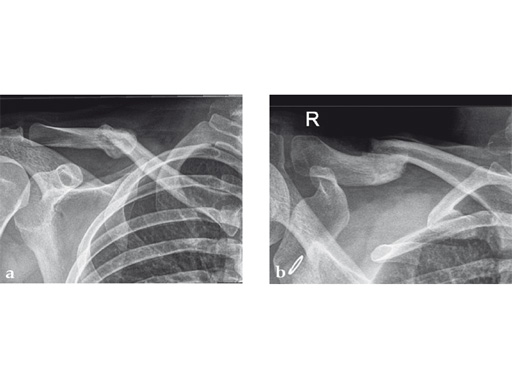
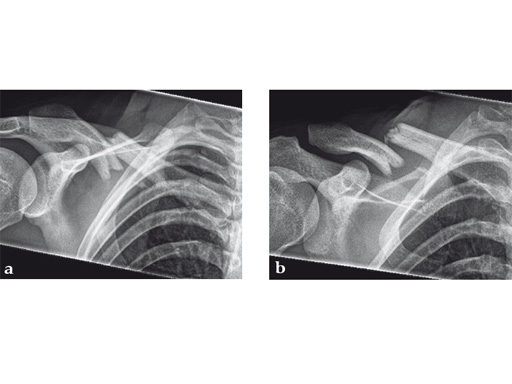
Case 1: a 30-year-old woman sustained a midshaft clavicle fracture. it healed with 2.1 cm shortening over 4 years after nonoperative treatment.
Case provided by Norbert Sdkamp and Martin Jaeger, Freiburg, Germany
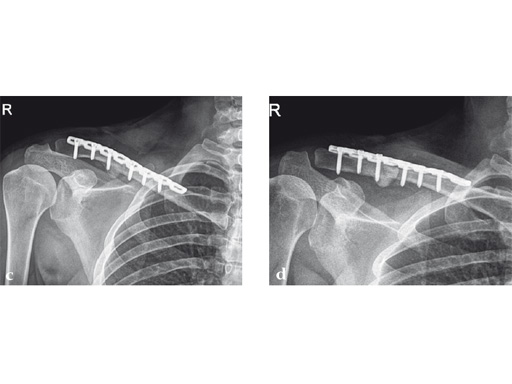
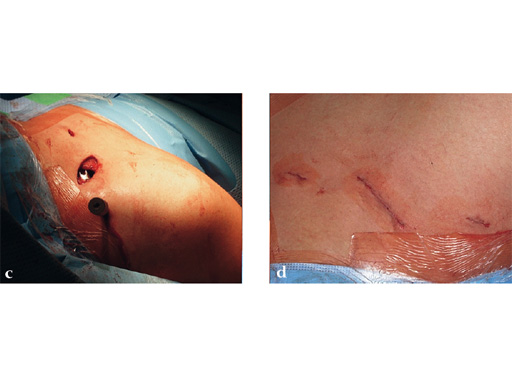
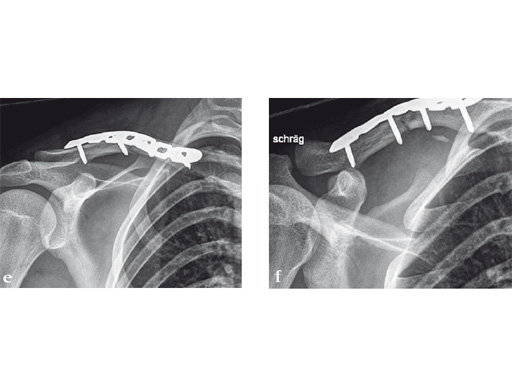
Case 2: a 29-year-old man sustained a midshaft clavicle fracture while playing soccer.
Case provided by Norbert Sdkamp and Martin Jaeger, Freiburg, Germany
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.