TomoFix Medial Distal Femur (MDF)
The goal of distal femur varus osteotomy is to shift the mechanical leg axis from the lateral to the medial compartment. There are various possibilities for surgical correction of valgus malalignment. The AO Knee Expert Group (KNEG) favors closing wedge osteotomy of the distal femur for valgus correction, because open wedge osteotomy on the lateral side causes significant morbidity due to tensioning of the iliotibial tract, and friction over the implant. The KNEG also found that distal femur opening wedge osteotomy did not show the same healing capacity as on the tibia and that bone grafting was necessary to avoid pseudarthrosis. Biomechanical testing confirmed superior stability of medial closing wedge techniques as compared to lateral open wedge techniques and favorable axial and torsional loading characteristics of an angular stable internal fixator, the TomoFix medial distal femur (MDF).
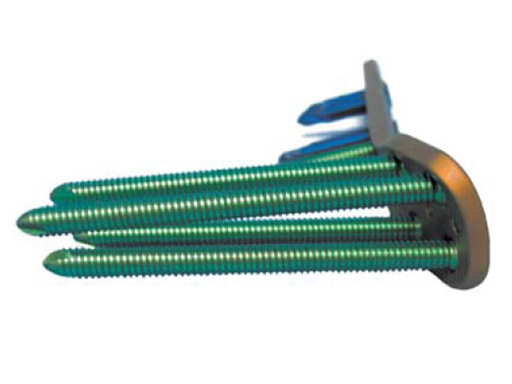
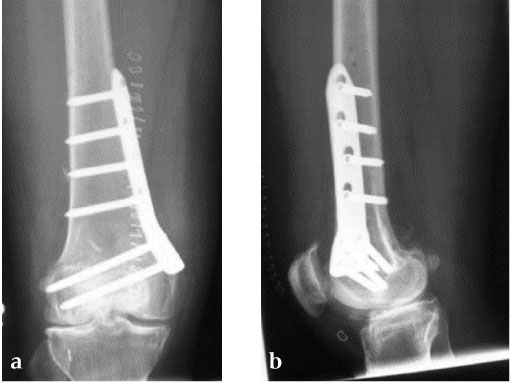
The TomoFix MDF features anatomically preshaped plates with a bending angle of 20. If needed during the operation, this angle can be further bent by using the bending press. The plate profile is 4?mm. The TomoFix MDF is available in a left and right version. The head of the plate offers four isolated LCP holes for 5.0?mm locking head screws. The screw axes of these four LCP holes are converged by 2. Through this alignment a cut-out of the screws can be prevented and the distance to the cruciate ligament is improved. The bolt angulation of 15 in the frontal plane enables use of longer screws and thus a more stable fixation. Bolt placement is easy and safe due to the anatomically adapted shape. The plate shaft features four standard 4.5/5.0 LCP combination holes which are shifted throughout the longitudinal axis. The end of the plate has a bullet nose for use of a MIO technique. Specific guiding blocks for the left and right plates help to insert the drill socket in the correct axis onto the plate.
The plate is inserted distally under the vastus medial muscle after screwing the threaded LCP drill guides into the four distal plate holes using the guiding block. The distal drill holes are oriented in a 20 angle inclination on the frontal plane to avoid a posterior perforation of locking head screws in the distal femur.
Biomechanical studies demonstrate that interfragmentary compression has a positive effect on bone healing. For this reason a lag screw is positioned in the dynamic compression unit directly above the osteotomy for compression of the osteotomy site.
The Patient can be mobilised as early as day one after surgery. Partial weight bearing is recommended for 6 weeks, active movement of the knee is encouraged. X-ray control after 6 weeks should demonstrate bony healing. Full weight bearing can be allowed in many cases after this time period, if the osteotomy site is still painful and bone healing is incomplete, weight bearing should be delayed for further 34 weeks.
Osteotomy around the knee has regained interest in the last years. The effect of malalignment on joint overload and osteoarthritis of the knee is well recognized, and the positive effect of correction of malalignment especially in the metaphyseal areas of tibia and femur on pain and function has been proven. The development of the TomoFix implants and the related instruments and techniques has popularized osteotomy in the German-speaking countries. The techniques have now also spread to the Asian world. The authors present an update on femoral osteotomy using the TomoFix implants.
Distal femoral varus osteotomyThe goal of distal femoral varus osteotomy is to shift the mechanical leg axis from the lateral to the medial compartment. There are various possibilities for surgical correction of valgus malalignment. Open wedge lateral osteotomy or dome osteotomies of the distal femur have been widely used in recent years. Unfortunately, local complaints occurred in many cases mostly caused by the fixation methods (ie, frequent irritations of the iliotibial tract and loss of correction). Therefore new improved surgical technique based on an incomplete medial closing wedge osteotomy with an internal plate fixator was developed.
Technique
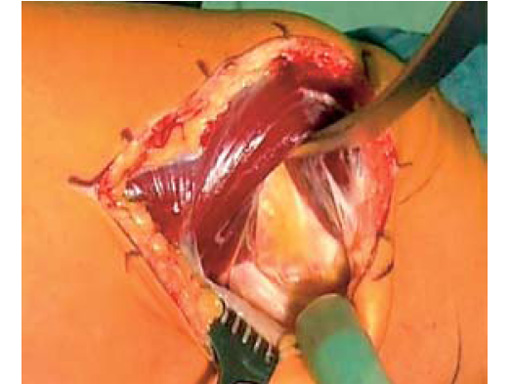
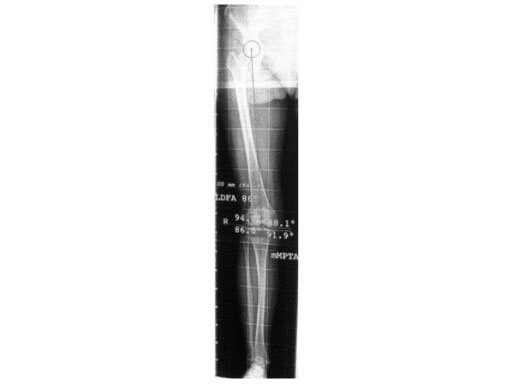
An anteromedial skin incision is used. This skin incision can be reused and expanded during subsequent knee surgery. The vastus medialis muscle is dissected from the septum, the medial patellofemoral ligament (MPFL) and the distal insertion of the vastus medialis muscle are partially incised. Two blunt Hohmann retractors are placed around the distal femur. The oblique osteotomy starts in the medial supracondylar area and ends in the lateral condyle, approximately 10 mm inside the lateral cortex. For guiding the closing wedge osteotomy of the distal femur a specific saw guide will be available soon. Alternatively, it is possible to use K-wires inserted under image intensifier control to mark the bone cuts. The saw cuts are made with retractors protecting the soft tissue and vessels. The wedge is removed and the height and depth of the osteotomy can be measured. At this time it is possible to make modifications concerning the wedge size. Closing the wedge must be done gradually by gentle compression of the lower leg laterally, and stabilizing the knee joint medially near the area of osteotomy. This may take several minutes to enable plastic deformation of the lateral cortex to close the osteotomy gap. Leg alignment is checked radiologically after closing with a rigid alignment bar positioned between hip and ankle center. The bar representing the weight-bearing line should pass the preoperatively defined mechanical axis. The plate is inserted from distal under the vastus medialis muscle. The distal drill holes are oriented in a 20 angle inclination on the frontal plane to avoid a posterior perforation of locking head screws in the distal femur. The distal four bolts are placed. A lag screw is positioned in the dynamic hole directly above the osteotomy for compression of the osteotomy site. The screw should be tightened carefully using the image intensifier. The plate is now fixed to the shaft with bolts monocortically, and the lag screw is replaced by a bolt bicortically. The wound is closed in layers after insertion of a drain. The patient is mobilized on the first day after surgery. Partial weight bearing is recommended for 6 weeks, active movement of the knee is enhanced. Biomechanical testing confirmed superior stability of medial closing wedge techniques as compared to lateral open wedge techniques and favourable axial and torsional loading characteristics of the TomoFix medial distal femur (MDF) plate. The plate is now available, as well as a booklet on the operative technique.
Literature
- Lobenhoffer P, Agneskirchner JD, Galla M (2006) Kniegelenknahe OsteotomienIndikation, Planung und Operationstechnik mit Plattenfixateuren. Stuttgart New York: Georg Thieme Verlag.
- Van Heerwaarden R, Wymenga A, Freiling D et al (2007) Distal medial closed wedge varus femur osteotomy stabilized with the TomoFix plate fixator. Operative Techniques in Orthopaedics; February:1221.
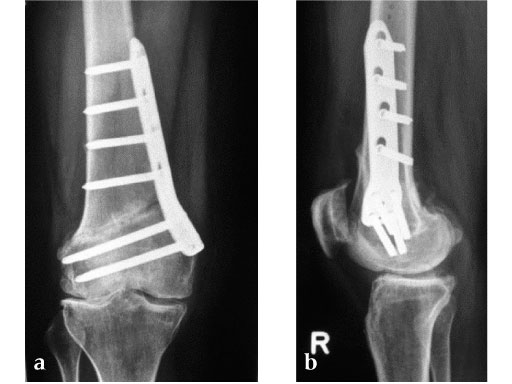
27-year-old male developed severe lateral joint line pain after lateral menicectomy.
Case provided by Philipp Lobenhoffer, Hannover, DE
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO”
The brands and labels “approved by AO Technical Commission” and “approved by AO”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.