AO Trauma Course—Shoulder and Elbow Trauma
Participants will learn the current management of patient pain, dysfunction, deformity, and cosmesis related to trauma of the shoulder and elbow. Fractures from the sternoclavicular joint to the forearm will be covered as well as joint injuries and dislocations and soft-tissue injuries (the acute trauma phase and the posttraumatic sequelae such as malunion, nonunion, infection, etc).
This course is aimed at orthopedic and trauma surgeons with at least 3 years of experience who want to develop expertise in shoulder and elbow fracture care or surgeons with many years of experience who want to update their knowledge.
Participants should also have completed the AO Trauma Course—Advanced Principles of Fracture Management.
Why you should choose this course
Top national, regional, and international faculty
2-3 days in duration
For surgeons who already treat shoulder and elbow trauma fractures
Network with colleagues from all over the world
CME credits
Course content
-
Course modules
- Module 1—Clavicle
- Module 2—Scapula
- Module 3—Proximal Humerus
- Module 4—Humeral shaft
- Module 5—Distal humerus, proximal ulna, and proximal radius
- Module 6—Elbow and radial and ulnar shaft
-
Small group discussions
Clavicle:
- Operative treatment of a diaphyseal fracture
- Failed treatment of a diaphyseal clavicle fracture
- Lateral clavicle fracture (and discuss associated injuries)
- AC ligament injury
- Malunion of clavicle
Scapula:
- Displaced scapular body fracture
- Floating shoulder
- Articular glenoid fracture
Proximal humerus:
- Multimorbid, frail patient with complex fracture (reverse prosthesis)
- Loss of reduction (Failed tuberosity fixation with a focus on prevention)
- Implant cutout (varus displaced, 4-fragment, osteoporotic, multimorbid with a focus on prevention)
- Intraarticular screw penetration
- Avascular necrosis
Humeral shaft
- Nonunion
- Multi-fragment fracture of the humeral shaft
- Radial nerve involvement
Distal humerus:
- Low supracondylar fracture in osteoporotic patient
OR
Intercondylar fracture of distal humerus
Proximal ulna:
- Multi-fragmentary proximal ulnar fracture (olecranon and coronoid)
Proximal radius:
- Compression fracture (Essex-Lopresti)
Elbow and radial and ulnar shaft
- Simple elbow dislocation
- Complex fracture-dislocation of the elbow
- Complex open multi-fragmentary forearm fracture
- Complex closed multi-fragmentary forearm fracture
Distal radius and ulna:
- Extraarticular distal radius fracture
- Radiocarpal fracture dislocation (volar)
- Radiocarpal fracture dislocation (dorsal)
- Complex multifragmentary articular fracture
- Ulnar extra articular
- Elderly indications for nonoperative intervention
Carpus:
- Scaphoid fracture
- Perilunate fracture dislocation
Hand:
- Fifth metacarpal extraarticular fracture (Boxer's)
- Multiple metacarpals with or without CMC dislocations
-
Anatomical Specimen Workshops (full day)*
Anterior exposures:
- Clavicle
- Humerus
- Elbow
- Distal radius
Posterior exposures:
- Scapula
- Humerus
- Distal humerus and proximal ulna
Course details may be subject to change. Please check your chosen date and location for the detailed program.
Target audience
- Orthopedic and trauma surgeons with at least 3 years of experience who want to develop expertise in upper extremity fracture care.
- Surgeons with many years of experience who want to update their knowledge.
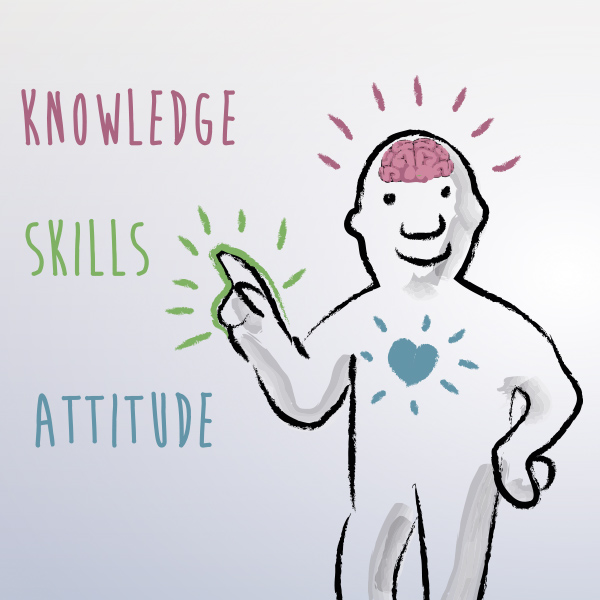
Competencies
The curriculum is based upon 7 competencies:
- Perform an appropriate assessment of the patient with trauma to the shoulder, humeral shaft, elbow, forearm, wrist, and hand
- Identify the minimal quality requirements for each assessment tool and the optimal way to gather the required information
- Perform a thorough, stepwise analysis of the problem (what is the mechanical, biological, and soft tissue situation and problem)
- Identify the advantages and disadvantages of the treatment options and decide with the patient which is best for their specific needs
- Develop a comprehensive plan based on the needs of the patient, the injury, the patient factors, and the available surgical options
- Complete the plan (perform operative procedures and nonoperative care)
- Provide and communicate overall care, integrating the team, family, and supporting care system
What does competency-based curriculum development mean?
Upper extremity education taskforce
The upper extremity education taskforce is a group of experts who build and continously improve our educational program. It consists of three international program editors (IPEs).

Odette Koch (ZA)
Term: 2022–2024

Sami Roukoz (LB)
Term 2023–2025

Pedro Labronici (BR)
Term: 2024–2026
See a full list of all regional program contributors and past international program editors.
Not the right course?
Find our list of all curricula courses here.