The new VA-LCP Periprosthetic Proximal Femur Plating System
Karl Stoffel, Mark Lee, Cong-Feng Luo, Rodrigo Pesantez, Christopher Finkemeier, George Haidukewych, Frank Liporace, Cory Collinge, Bruce Ziran, Christoph Sommer
The new 3.5/4.5 Variable Angle LCP® Periprosthetic Proximal Femur Plating System was developed for treatment of Vancouver types A and B fractures. It is offered in stainless steel.
The modular system consists of anatomically pre-shaped plates with variable angle locking screw technology. The versatility of the system allows the surgeon to connect the plate components in various configurations in response to different fracture patterns. The number of plate holes and their location were chosen to facilitate high fixation density around an intramedullary implant. The distal spanning attachment plate is intended to prevent fractures of the intact distal femur rather than span a fracture. It is designed to avoid abrupt stiffness changes in the fixation construct by distributing the load among multiple fixation points in the lateral femoral condyle.
Clinical problem
Incidence of periprosthetic and peri-implant femoral fractures
Hip arthroplasty is a commonly performed procedure to treat various hip pathologies. Due to the general aging of the population and increased lifestyle demands, the number of people receiving hip replacements is expected to rise [1]. The demand for primary total hip arthroplasties (THAs) in the United States is estimated to grow by 174% from 2005 to 2030 [2]. Total hip revisions are projected to grow by 137% in this time span [2].
As the number of THAs increase, the number of periprosthetic femoral fractures (PFFs) that occur intraoperatively and postoperatively is also expected to rise Although rare, PFF is a severe complication of THA. Following primary THA the 20-year probability of sustaining a postoperative PFF is reported to be 7.7% after placement of an uncemented stem and 2.1% after placement of a cemented stem [3]. The cumulative 20-year postoperative PFF risk increased to 11% [4] for revision THA. Most PFFs are caused by low-energy trauma events [5, 6]. A metaanalysis suggested that female gender, rheumatoid arthritis, and revision arthroplasty are major risk factors for the development of PFF after THA [7].
A non-prosthetic peri-implant fracture is a challenging clinical problem with a high rate of postoperative complications [8]. Chan et al [8] concluded that these fractures are distinct from periprosthetic fractures and should be understood as a separate entity. Ipsilateral refracture of the femur after intramedullary nail fixation is a sub-entity of femoral peri-implant fractures. A study [9] of 609 patients with pertrochanteric hip fracture treated with short and long intramedullary nails described an ipsilateral fracture rate between 1.6% at 1 year and 8.9% at 5 years. A retrospective study [10] noted 15 peri-implant fractures in a series of 705 proximal femoral nails inserted between 2006 and 2015 (fracture rate, 2.1%). If nail revision is not indicated and if the nail is short, fracture fixation could be achieved with a proximal femoral plate bridging the fracture. Such a plate will benefit from plate features, which facilitate plate anchorage around the nail.
Fracture classification of periprosthetic femoral fractures
The Unified Classification System for Periprosthetic Fractures was introduced in 2013 [11]. It also classifies fractures about or in a bone with a non-arthroplasty implant. Since many publications on PFFs use the Vancouver classification [1] system we refer to it in this article. The Vancouver classification system is based on fracture location, the stability of the femoral component, and the quality of the bone stock. Type A fractures are confined to the greater (AG) or lesser (AL) trochanter. Type B fractures are diaphyseal, around the prosthesis or immediately distal to it, and are divided into three subtypes: B1, B2, and B3, characterized by a well-fixed stem, an unstable or loose stem with good quality of the surrounding bone stock, and an unstable or loose stem with inadequate surrounding bone stock, respectively [1]. Stoffel et al [12] presented an algorithmic approach to identifying loose stems around proximal femoral periprosthetic fractures, taking patient history, stem design, and plain x-rays into consideration. Type C fractures occur below the tip of the prosthesis. Based on 1049 PFFs that were reported to the Swedish National Hip Arthroplasty between 1979 and 2000, Lindahl et al found [13] that more than 80% of the fractures were type B fractures (type A: 4%, type B1: 29%, type B2: 53%, type B3: 4%, and type C: 10%).
Complications after surgical treatment of periprosthetic femoral fractures
Most PFFs are treated surgically including open reduction and internal fixation (ORIF), revision THA, and revision THA in combination with ORIF [12]. Most treatment protocols are based on the Vancouver classification. Type A fractures may be treated either conservatively or surgically, depending on the stability of the fracture [12]. In general, it is accepted that types B1 and C fractures should be treated with ORIF. Type B2 fractures typically require revision THA with a longer stem (and additional ORIF as needed). In selected cases with B2 fractures, internal fixation with plate, screws and cerclage can be a viable alternative option [14]. Revision THA with more complex reconstruction procedures are usually used for type B3 fractures. Since many PFFs require ORIF as part of their treatment there is a need for adequate implants including plates, screws, cerclage wires and cables. Their use is challenging because patients often have diminished bone quality and the physical presence of the THA, and possibly a cement mantle, obstruct adequate proximal fixation. High failure rates have been reported for plate fixation of PFFs [13]. Advances in plating techniques and technology have improved the outcomes of PFF treatment [15].
Internal fixation is frequently achieved with locking plates, using minimally invasive surgery and indirect fracture reduction techniques leading to favorable results [15]. In a series of 60 consecutive type B1 and type C fractures treated with locked plating three fractures had to be reoperated due to failure of fixation (failure rate 5%) [16]. A retrospective review [17] of 14 patients (11 patients with revision arthroplasties) led to less favorable results. In nine fractures that were only treated with locked plating there were five failures because of plate breakage or plate pullout (failure rate, 56%) leading the authors to recommend the use of additional struts to treat these fractures. Another study [18] reported that in case of transverse type B1 fractures around the stem tip locked plating alone has a high failure rate, which emphasizes the importance of using additional fixation for the treatment of this fracture pattern. These studies imply that better implants are required for the treatment of PFFs.
There are concerns that stress risers at the end of a locking plate construct may lead to complications like refracture of the femur [19, 20]. A strategy to avoid potential complications is to protect the femur with femoral-spanning plates. Moloney et al [21] concluded that for treatment of type B1 fractures a plate fixation that spans the length of the femur to the level of the femoral condyles is associated with a decreased rate of nonunion and refracture compared with short plate fixation.
The rate and strength of healing is intimately linked to the integrity of surrounding soft tissues [22]. A loss of periosteal blood supply and soft tissue stripping increase the risk of nonunion, failure, and refracture [15]. The use of more streamlined implants may better preserve the periosteal blood supply and facilitate bone perfusion and biological response and may reduce the likelihood of implant removal due to irritation [23, 24].
References
1. Stoffel K, Blauth M, Joeris A, et al. Fracture fixation versus revision arthroplasty in Vancouver type B2 and B3 periprosthetic femoral fractures: a systematic review. Arch Orthop Trauma Surg. Oct 2020;140(10):1381–1394.
2. Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. Apr 2007;89(4):780–785.
3. Abdel MP, Watts CD, Houdek MT, et al. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Joint J. Apr 2016;98-B(4):461–467.
4. Abdel MP, Houdek MT, Watts CD, et al. Epidemiology of periprosthetic femoral fractures in 5417 revision total hip arthroplasties: a 40-year experience. Bone Joint J. Apr 2016;98-B(4):468–474.
5. Zuurmond RG, van Wijhe W, van Raay JJ, et al. High incidence of complications and poor clinical outcome in the operative treatment of periprosthetic femoral fractures: an analysis of 71 cases. Injury. Jun 2010;41(6):629–633.
6. Legosz P, Platek AE, Rys-Czaporowska A, et al. Correlations between Vancouver type of periprosthetic femur fracture and treatment outcomes. J Orthop. May 2019;16(6):517–521.
7. Bissias C, Kaspiris A, Kalogeropoulos A, et al. Factors affecting the incidence of postoperative periprosthetic fractures following primary and revision hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. Jan 2021;16(1):15.
8. Chan LWM, Gardner AW, Wong MK, et al. Non-prosthetic peri-implant fractures: classification, management and outcomes. Arch Orthop Trauma Surg. 2018 Jun;138(6):791–802.
9. Lindvall E, Ghaffar S, Martirosian A, et al. Short versus long intramedullary nails in the treatment of pertrochanteric hip fractures: incidence of ipsilateral fractures and costs associated with each implant. J Orthop Trauma. 2016 Mar;30(3):119–124.
10. Müller F, Galler M, Zellner M, et al. Peri-implant femoral fractures: the risk is more than three times higher within PFN compared with DHS. Injury. 2016 Oct;47(10):2189–2194.
11. Duncan CP, Haddad FS. Classification. In: Schütz M, Perka C, ed. Periprosthetic Fracture Management. Stuttgart: Georg Thieme; 2013:47–90.
12. Stoffel K, Horn T, Zagra L, et al. Periprosthetic fractures of the proximal femur: beyond the Vancouver classification. EFORT Open Rev. Aug 2020;5(7):449–456.
13. Lindahl H, Malchau H, Odén A, et al. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br. 2006 Jan;88(1):26–30.
14. Spina M, Scvalvi A. Vancouver B2 periprosthetic femoral fractures: a comparative study of stem revision versus internal fixation with plate. Eur J Orthop Surg Traumatol. 2018;28:1133–1142.
15. Marsland D, Mears SC. A review of periprosthetic femoral fractures associated with total hip arthroplasty. Geriatr Orthop Surg Rehabil. 2012 Sep;3(3):107–120.
16. Froberg L, Troelsen A, Brix M. Periprosthetic Vancouver type B1 and C fractures treated by locking-plate osteosynthesis. Acta Orthop. 2012 Dec;83(6):648–652.
17. Buttaro MA, Farfalli G, Paredes Nunez M, et al. Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg Am. 2007;89(9):1964–1969.
18. Min BW, Lee KJ, Cho CH, et al. High failure rates of locking compression plate osteosynthesis with transverse fracture around a well-fixed stem tip for periprosthetic femoral fracture. J Clin Med. 2020 Nov 22;9(11):3758.
19. Graham SM, Moazen M, Leonidou A, et al. Locking plate fixation for Vancouver B1 periprosthetic femoral fractures: a critical analysis of 135 cases. J Orthop Sci. 2013 May;18(3):426–436.
20. Vicenti G, Bizzoca D, Solarino G, et al. Periprosthetic femoral re-fractures pathogenesis, classification, and surgical implications. Injury. 2020 Nov 11;S0020-1383(20)30954–30962.
21. Moloney GB, Westrick ER, Siska PA, et al. Treatment of periprosthetic femur fractures around a well-fixed hip arthroplasty implant: span the whole bone. Arch Orthop Trauma Surg. 2014 Jan;134(1):9–14.
22. Davis KM, Griffin KS, Chu TG, et al. Muscle-bone interactions during fracture healing. J Musculoskelet Neuronal Interact. Mar 2015;15(1):1–9.
23. Firoozabadi R, Graves M, Krieg J, et al. Achieving construct stability in periprosthetic femur fracture treatment. Advances Orthop Surg. 2014;1–4.
24. Smolle MA, Hörlesberger N, Maurer-Ertl W, et al. Periprosthetic fractures of hip and knee: a morbidity and mortality analysis. Injury. Open access published Jan 19, 2021.
Approach to develop better treatment solutions
Realizing the deficiencies in the treatment of PFFs and peri-implant femoral fractures, the AO Technical Commission formed a dedicated Periprosthetic Fracture Task Force (PFTF) which was mandated to develop better osteosynthesis solutions for these challenging fractures in cooperation with DePuy Synthes (DPS). Medical members of the PFTF were Karl Stoffel (chair), Mark Lee, Christopher Finkemeier, Michael Blauth, Steve Velkes, George Haidukewych, Cory Collinge, Frank Liporace, and Bruce Ziran (Fig 1).
The PFTF identified following main requirements for the development of a state-of-the-art proximal femoral plating system (focusing on types A and B fractures):
- Modular implant configuration to address a wide variety of PFFs.
- Implant system with many fixation options to achieve high osteosynthesis stability in poor bone quality.
- Implant design to facilitate fracture fixation in presence of THAs and other intramedullary implants (eg, short proximal nails).
- Soft tissue friendly solution that minimizes damage to the blood supply.
- Implant that allows to span and protect the whole femur.
The medical members of the Lower Extremity Expert Group (Christoph Sommer, Rodrigo Pesantez, and Cong-Feng Luo) accompanied the development to refine the implant design. Various Anatomy Labs were performed to optimize the surgical technique (Fig 2).
In addition to a proximal plating system, the PFTF and the Intramedullary Nailing Expert Group developed a new retrograde femoral nail with an innovative locking attachment plate (RFN-Advanced Retrograde Femoral Nailing System) for native and periprosthetic distal femoral fractures associated with total knee arthroplasties which was launched in 2020.
Solutions
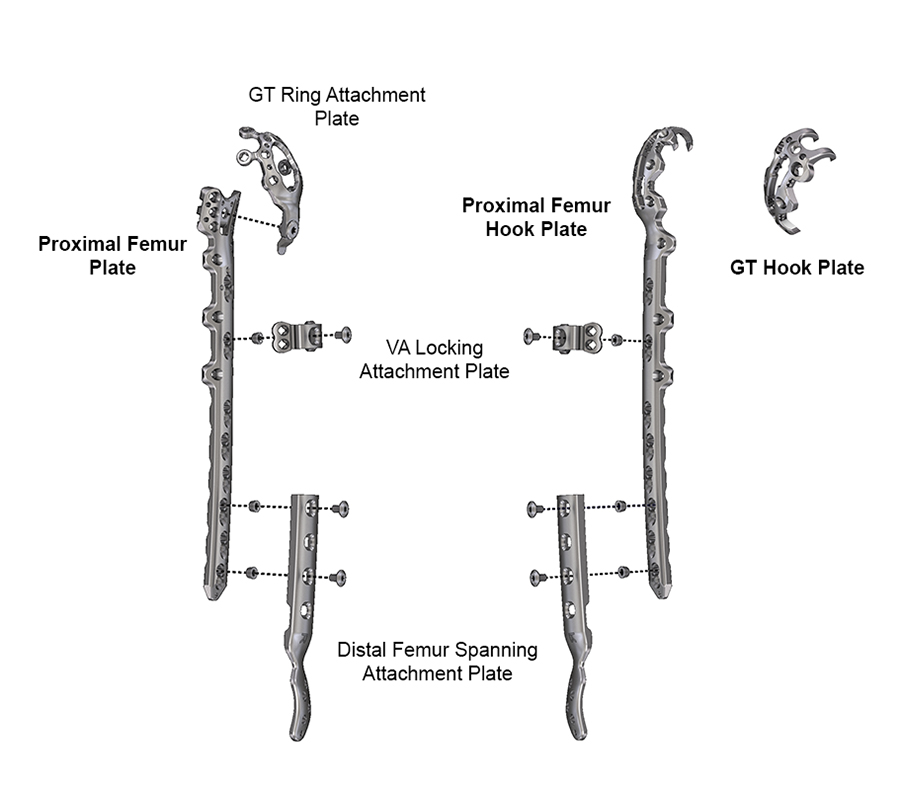
The 3.5/4.5 Variable Angle LCP® Periprosthetic Proximal Femur Plating System addresses the identified clinical needs by providing two main proximal plate options and three additional attachment plates with dedicated plate features (Fig 3). The anatomically shaped plate variations and compact plate connections were designed to minimize soft tissue irritations. The modular aspect of this system allows the surgeon to connect the available devices in various configurations, thereby focusing on the variety of fracture type and promoting fixation of the fracture according to the surgeon’s preference. All plates are equipped with Variable Angle (VA) Locking Screw holes, allowing angulation possibilities of up to 15° in each direction around the central axis of the plate hole to bypass intramedullary implants.
The Proximal Femur Plate and the Proximal Femur Hook Plate are the two main plates. The Greater Trochanter (GT) Ring Attachment Plate, VA Locking Attachment Plate and Distal Femur Spanning Attachment Plate can be assembled to the two main plates with threaded inserts and upper screws. A dedicated Greater Trochanter (GT) Hook Plate without plate shaft is available as standalone device for fixation of simple type AG fractures as well as greater trochanter osteotomies.
There are sizing templates available for all plates which help to select the proper plate(s) for the best plating combination and assembly.
The surgical technique guide provides guidance on implant selection depending on fracture pattern and fixation recommendations (minimum number of screws and cortices).
Not all of the plates are available in all regions of the world due to local medical device regulations.
Plate features
3.5/4.5 VA-LCP PPFx Proximal Femur Plates (VA-PFP)
The VA-PFP (Fig 4) has an anatomically shaped plate head and shaft. It includes 3.5 VA locking holes in the plate head and proximal plate shaft to provide fixation points around an intramedullary implant. There are 4.5 VA-LCP combi-holes in the plate shaft accepting 4.5 mm cortex screws, 5.0 mm VA Locking Screws and monocortical 5.0 mm VA PPFx Locking Screws. The plate was specifically designed to address type B or combined types AG and B fractures.
(1) Six 3.5 mm VA Locking holes, offset from the axis of the femur.
(2) Six holes with undercuts for wire or suture attachments.
(3) Threaded hole and slot to connect GT Ring Attachment Plate.
(4) Anterior and posterior 3.5 mm VA Locking offset holes. Number increasing with plate length.
(5) 4.5 mm VA-LCP combi holes.
- Proximal plate shaft: centered. Number increasing with plate length.
- Distal plate shaft: staggered. Six holes.
(6) Curvature to fit the femoral shaft anatomy.
(7) Distal flare to fit the distal femoral anatomy (for 9-hole and longer plates).
(8) Distal plate tip with wire hole and slot for Articulated Tension Device.
The plate head and proximal plate shaft must not be bent. The plates are side specific (left and right versions) and are available in following lengths: 2-hole (119 mm), 7-hole (216 mm), 8-hole (251 mm), 9-hole (285 mm), 10-hole (320 mm), 11-hole (354 mm) and 12-hole (388 mm). The 2-hole plate must always be used in combination with the GT Ring Attachment Plate and not as a standalone plate.
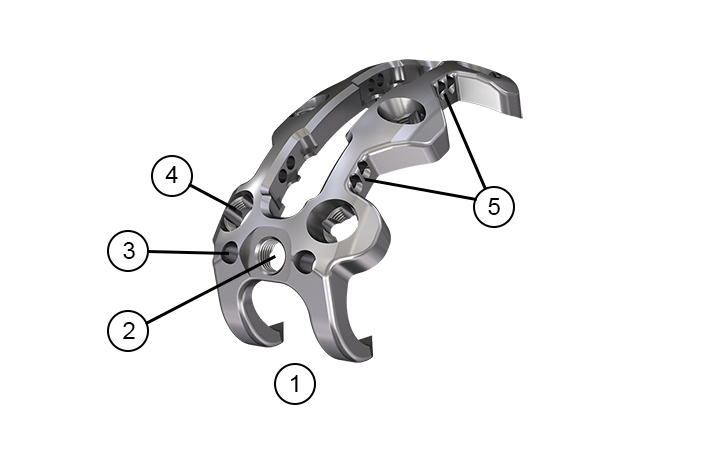
3.5/4.5 VA-LCP PPFx Proximal Femur Hook Plates (VA-PFHP)
The VA-PFHP (Fig 5) has an anatomically shaped plate head and shaft. It has two proximal hooks as well as cable slots to reduce the greater trochanter. There are 3.5 VA locking holes in the plate head and proximal plate shaft to provide fixation points around an intramedullary implant. The VA-PFHP contains 4.5 VA-LCP combi holes in the plate shaft accepting 4.5 mm Cortex Screws, 5.0 mm VA Locking Screws and monocortical 5.0 mm VA PPFx Locking Screws. The plate was specifically designed to treat types AG and B fractures.
(1) Two superior sharp hooks of which the posterior one slightly elongated.
(2) Threaded hole for insertion handle.
(3) Two wire holes for provisional fixation.
(4) Six 3.5 mm VA Locking holes, offset from the axis of the femur.
(5) Center slot to place two cables and cable crimps with corresponding holes for cable passage.
(6) Anterior and posterior 3.5 mm VA Locking offset holes. Number increasing with plate length.
(7) 4.5 mm VA-LCP combi holes.
- Proximal plate shaft: centered. Number increasing with plate length.
- Distal plate shaft: staggered. Six holes.
(8) Curvature to fit the femoral shaft anatomy.
(9) Distal flare to fit the distal femoral anatomy (for 10-hole plate only).
(10) Distal plate tip with wire hole and slot for Articulated Tension Device.
The plate head and proximal plate shaft must not be bent. The plates are side specific (left and right versions). There are plates with a small plate head and a large plate head (6 mm larger) available in following lengths:
Plates with small plate head: 5-hole (211 mm), 8-hole (285 mm), 10-hole (354 mm)
Plates with large plate head: 5-hole (217 mm), 8-hole (291 mm), 10-hole (360 mm)
3.5 VA Locking PPFx Greater Trochanter Hook Plates (VA-GTHP)
The VA-GTHP (Fig 6) is a short implant without plate shaft. It is indicated for fixation or re-attachment of the greater trochanter following fracture or osteotomy.
(1) Two superior sharp hooks.
(2) Threaded hole for insertion handle.
(3) Two wire holes for provisional fixation.
(4) Six 3.5 mm VA Locking holes, offset from the axis of the femur.
(5) Center slot to place two cables and cable crimps with corresponding holes for cable passage.
The VA-GTHP is available in two sizes. The large plate is 6 mm longer than the small one. The plate profile is universal for left and right application.
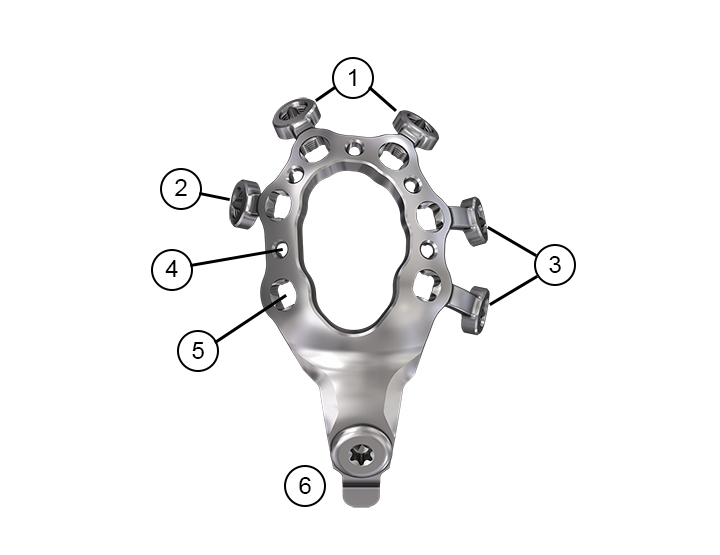
3.5 VA Locking PPFx Greater Trochanter Ring Attachment Plates (VA-GTRAP)
The VA-GTRAP (Fig 7) must be used with the VA-PFP and not as a standalone device. The inner ring must not be bent. In combination with the VA-PFP the plate is indicated for fixation or re-attachment of the greater trochanter following a fracture or osteotomy.
(1) Two contourable superior arms, with 3.5 mm VA Locking holes.
(2) Contourable posterior arm, with 3.5 mm VA Locking hole.
(3) Two contourable anterior arms, with 3.5 mm VA Locking holes.
(4) Five holes with undercuts for wire or suture attachments.
(5) Inner ring with six 3.5 mm VA Locking holes.
(6) One-screw connection to VA-PFP, pre-assembled, with a tab for secondary connection.
The VA-GTRAP is available in two sizes. The large plate is 5 mm longer than the small one. The plates are side specific (left and right versions).
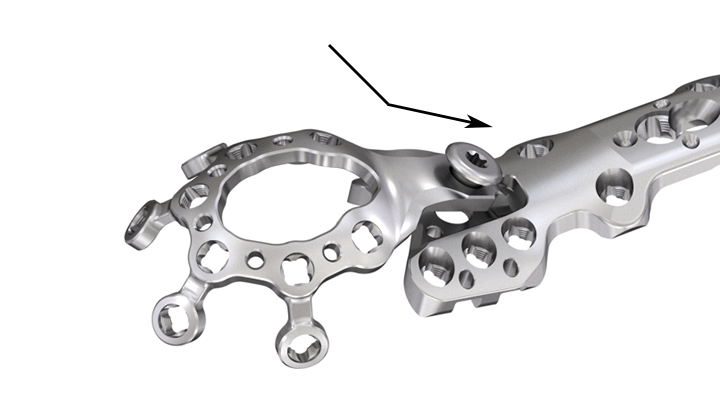
The VA-GTRAP must be attached before the VA-PFP is in situ (Fig 8). The assembly is performed by inserting the tab of the VA-GTRAP in the slot of the VA-PFP and by tightening the connecting screw with the 6 Nm torque limiting handle.
3.5 VA Locking Attachment Plate (VA-LAP)
The VA-LAP (Fig 9) attaches to both main plates (VA-PFP and VA-PFHP) and serves as an alternative to cables for added fixation around intramedullary implants. The VA-LAP must not be used as a standalone device. It is indicated to augment the stabilization of fractures, including type B fractures when used with either the VA-PFP or the VA-PFHP, types B and C fractures when used with other LCP plates and VA-LCP plates and fractures in the presence of intramedullary implants, in the femur, tibia, and humerus.
(1) Contourable tabs with four 3.5 mm VA Locking holes.
(2) Middle slot, allowing a one-point connection with the main plate, using one connecting screw.
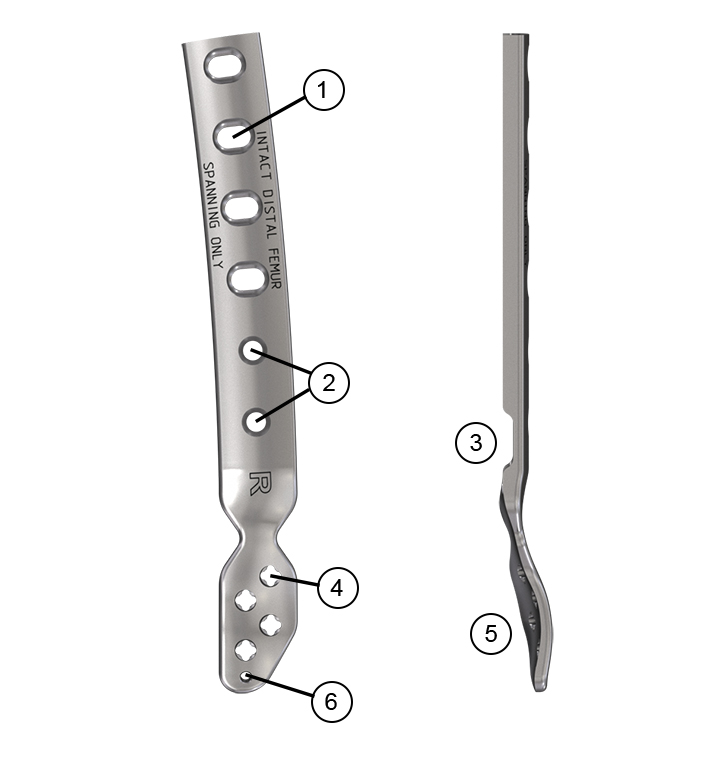
3.5 VA Locking PPFx Distal Femur Spanning Attachment Plate (VA-DSAP)
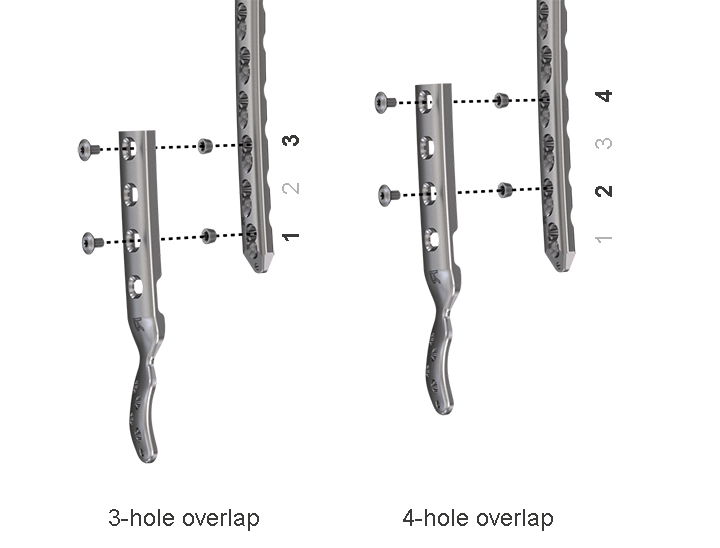
The VA-DSAP (Fig 10) attaches to both main plates (VA-PFP and VA-PFHP) to extend the fixation construct over the intact distal femur to the lateral femoral condyle. The plate overlap for the assembly must be either three or four holes (Fig 11). Two connecting screws are required to attach the VA-DSAP to two non-adjacent holes of the main plate. The VA-DSAP must not be used to span a fracture as this could lead to implant failure. The plate distributes stress among multiple points of fixation and is designed to avoid abrupt stiffness changes, thereby supporting the distal bone to protect it from further fractures.
(1) Four slots in the plate shaft for two-point connection with the main plate.
(2) The 6-hole plate version includes two 4.5 mm Cortex Screw holes.
(3) Bending Iron slot.
(4) Four 3.5 mm VA Locking holes in the plate head.
(5) Pre-shaped plate head to fit the intact distal femur and lateral femoral condyle.
(6) Wire hole for provisional fixation.
The VA-DSAP is attached to the main plate using a 3-hole or 4-hole overlap with two connecting screws (threaded inserts and upper screws) in non-adjacent holes of the main plate (Fig 11).
Innovations in Treatment of Periprosthetic Proximal Femur Fractures
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO Foundation”
The brands and labels “approved by AO Technical Commission” and “approved by AO Foundation”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.