RFN-Advanced Retrograde Femoral Nailing System
Christopher Finkemeier, Martin Hessmann, Mark Lee, Andrew Oppy, Karl Stoffel
Retrograde nailing of native and periprosthetic distal femoral fractures can be challenging due to:
- limited implant anchorage possibilities in far distal fractures,
- challenging implant placement in the presence of prosthesis components or other implants.
Insufficient implant anchorage may result in malunions, delayed unions, or nonunions requiring revision surgery. The new RFN-Advanced (RFN-A) Retrograde Femoral Nailing System was developed to address these issues. The Locking Attachment Washer (LAW) can be regarded as the most important innovation of the RFN-A System. The LAW concept allows to connect an anatomically shaped 6-hole plate (the locking attachment washer) at the lateral femoral epicondyle to the retrograde nail in an angular stable manner. The enhanced fixation options of the RFN-A will be beneficial to expand the retrograde nailing indications toward far distal fractures, to improve implant anchorage in poor bone quality, and to support early patient mobilization.
Clinical problem
Distal femoral fractures typically occur in young patients because of high-energy trauma and in elderly patients because of simple falls. After the age of 60 years, a rapid increase in the incidence of distal femoral fractures has been reported in both genders, with a large female predominance [1]. Depending on the degree of comminution, patient factors, revisional history, and the possible involvement of prostheses, treatment of distal femoral fractures can be challenging. Surgical management aims to provide adequate stability for fracture healing, to maintain reduction, and to allow early postoperative patient mobilization. The latter aspect is significant because of the growing number of elderly patients with limited ability to comply with partial weight-bearing protocols. Hence, there is a demand for fracture fixation solutions that can resist high loads across the fracture site. Retrograde intramedullary nailing (IMN) as well as locked plating are commonly used techniques to treat distal femoral fractures. Similar nonunion and revision rates have been reported for both surgical procedures for native [2] and periprosthetic fractures [3]. From a biomechanical perspective, IMN offers a higher load-bearing capacity compared with lateral locked plating because the fixation device is closer to the weight-bearing axis of the femur. However, with retrograde nailing of native and periprosthetic distal femoral fractures, the following disadvantages compared with locked plating are: (1) limited implant anchorage possibilities in far distal fractures, (2) challenging implant placement in the presence of prosthesis components or other implants. Insufficient implant anchorage may result in malunions, delayed unions, or nonunions requiring revision surgery with corresponding burden on the healthcare system. The Periprosthetic Fracture Task Force and the Intramedullary Nailing Expert Group (INEG) (Fig 1) considered all these aspects in the development of a state-of-the-art retrograde nailing system - the new RFN-Advanced Retrograde Femoral Nailing System.
References
1) Elsoe R, Ceccotti AA, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop. 2018 Jan;42(1):191196.
2) Hierholzer C, von Rden C, Ptzel T, et al. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: a retrospective analysis. Indian J Orthop. 2011 May-Jun; 45(3): 243250.
3) Shin YS, Kim HJ, Lee DH. Similar outcomes of locking compression plating and retrograde intramedullary nailing for periprosthetic supracondylar femoral fractures following total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017 Sep;25(9):29212928.
Clinical solutions
RFN-Advanced Retrograde Femoral Nail
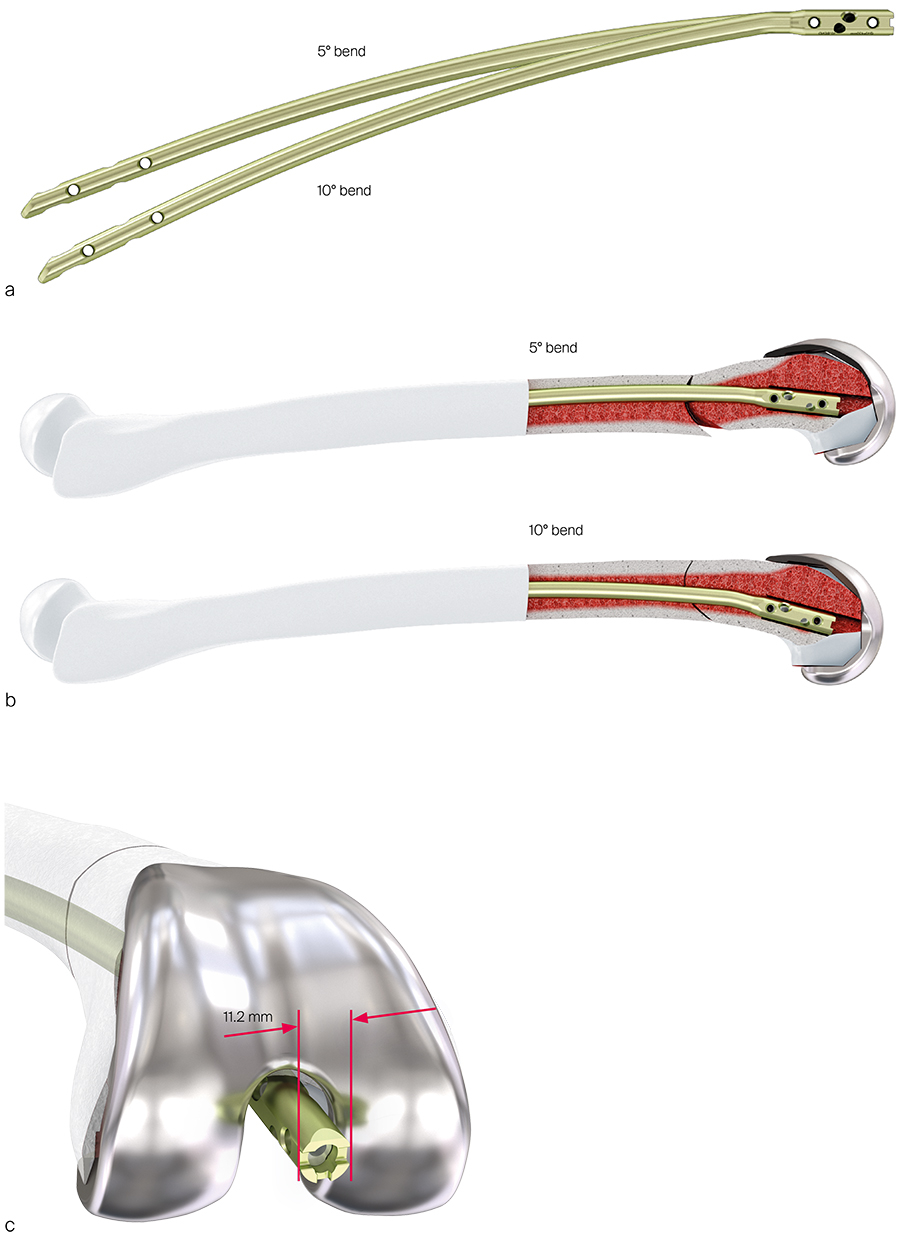
The first aspect in the development of the RFN-Advanced (RFN-A) Retrograde Femoral Nail was the analysis of the best nail shape based on an anatomical study with many femoral CT scans. The study revealed that two nail shapes with different distal bends are required to adequately address native and periprosthetic fractures. The RFN-A is therefore provided with a 5° bend and a 10° bend (Fig 2a). The nail with the 10° bend is advantageous for fixation of periprosthetic fractures where the entry point is forced to be more posterior due to the presence of a total knee arthroplasty. Thus the risk of an extension deformity as a result of a posterior nail entry portal can be reduced (Fig 2b). The surgeon can choose between the two nail shapes based on the fracture configuration and implant placement factors. There could be periprosthetic fracture cases where the 5° bend nail might be better than the 10° bend nail. Similarly, the 10° bend nail might be preferred over the 5° bend nail to address native fractures. The nails have flat edges at the medial and lateral sides to limit the maximum nail width to 11.2 mm to fit through most total knee arthroplasties (TKAs) (Fig 2c).
All nails have a 1.0 m radius of curvature to address the anterior bend of the femur. This nail bend is the same as for the TFN-Advanced Proximal Femoral Nail and the FRN-Advanced Femoral Recon Nail. The RFN-A is made of the same material as the TN-A (Ti-6Al-4V). The universal nail design for the left and right femur helps to reduce the nail portfolio.
The RFN-A is offered in following diameters and lengths:
- Nail diameters: 9 mm, 10 mm, 11 mm, 12 mm, and 14 mm (only 5° bend nail).
- Nail lengths: 160 mm to 280 mm in 40 mm increments and 300 mm to 480 mm in 20 mm increments.
The nail cross section is round for the nail diameters 9 mm and 10 mm and fluted for the larger diameter nails.
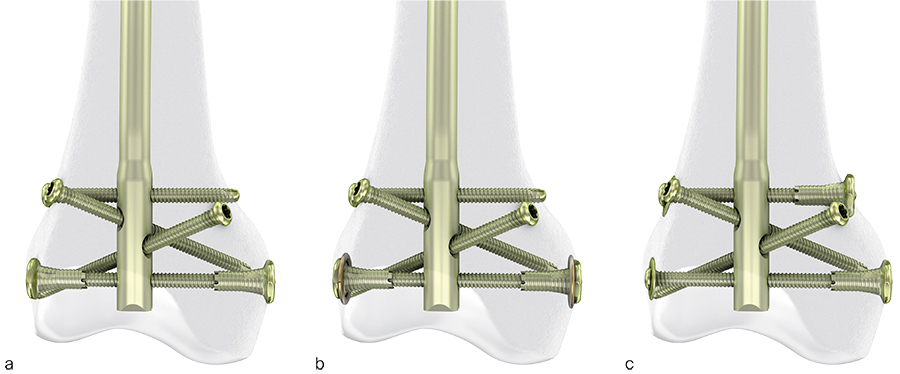
Nail locking options and locking screws
All nails have four multiplanar distal locking options (Fig 4). For proximal locking, the long nails (300 mm to 480 mm nail length) have two lateral to medial (LM) and two anterior to posterior (AP) locking options. The short nails (160 mm to 280 mm nail length) allow locking with 2 LM screws.
The RFN-A has a preassembled polymer inlay at the distal nail part to achieve angular stable locking between the locking screws and the nail. Angular stable locking reduces interfragmentary motion and screw toggle. According to development test data, the angular movement of a locking screw in the nail without sleeve was more than twice as high as that of an angular stable locking screw in the nail with sleeve.
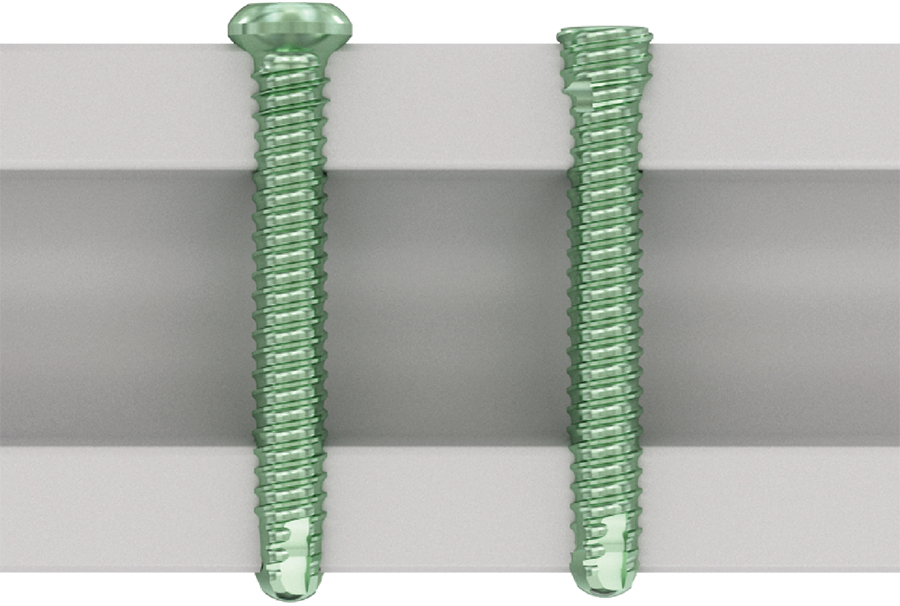
The nail can be locked with two new types of 5 mm locking screws (Fig 3): Locking Screw (headed design) and Low Profile Locking Screw (headless design). The latter can be helpful to avoid soft-tissue irritations at the lateral femoral epicondyle.
In poor bone quality even angular stable locking screws may cut through the bone resulting in loss of nail fixation. To improve distal implant anchorage and increase resistance against cut through, the surgeon can choose one of the following two enhanced fixation options.
Enhanced fixation option 1: titanium nuts and washers for locking screws
The RFN-Advanced Retrograde Femoral Nailing System comprises optional titanium condylar nuts and washers.
Nut and washer designs
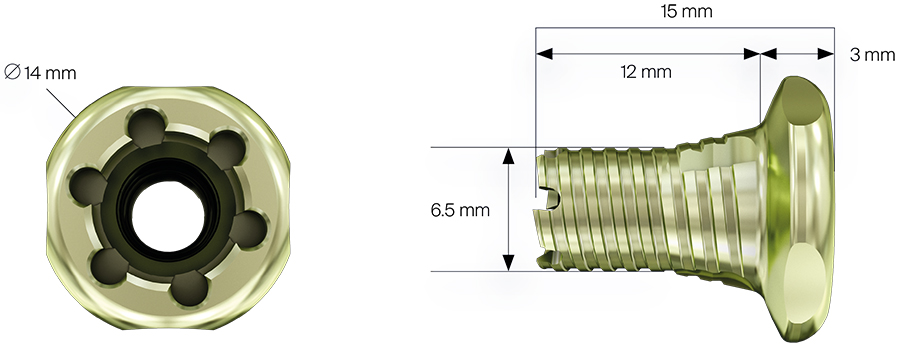
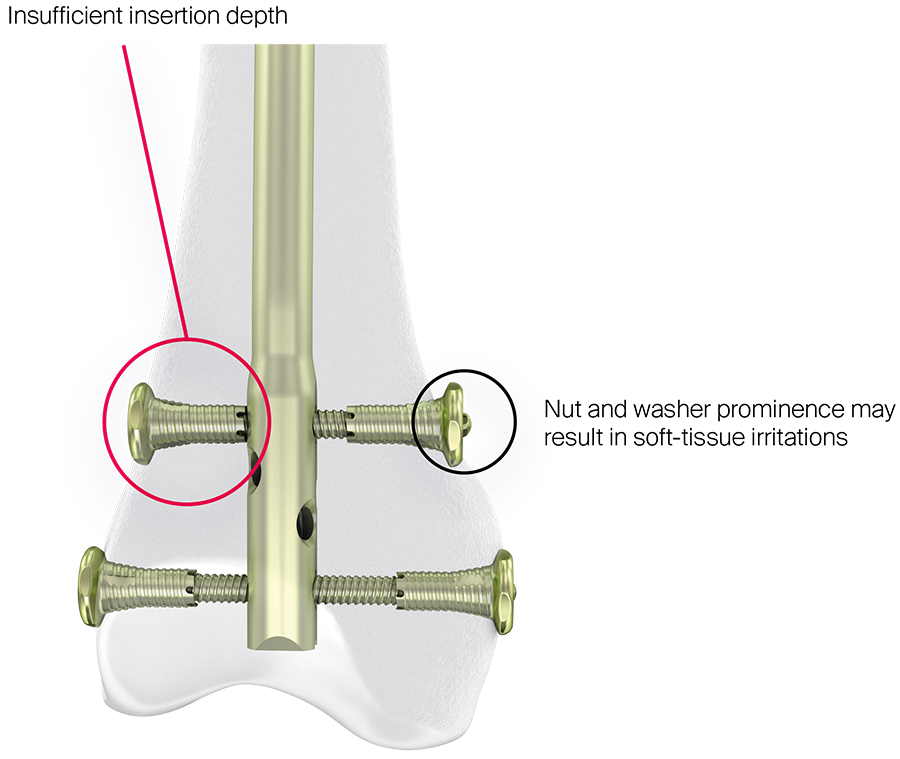
The conical design of the nut (largest outer diameter: 14 mm) increases the interlocking surface in the bone of the femoral condyles (Fig 5). The nuts can be assembled to sit underneath the locking screw head and at the screw tip. The surgeon can either use nuts on both sides of the femoral condyles or only on one side. The nut has a friction feature to avoid unintentional loosening from the locking screw. A countersink can be used to ease insertion of the nut in hard bone.
Titanium washers with 1.1 mm thickness are available for the nut to increase the outer diameter of the locking construct to 17 mm, which reduces the risk of the nut sinking into the bone. There are also titanium washers of 1.2 mm thickness for the standard locking screws available to increase the outer diameter without use of the nut to 14 mm. Locking screws, nuts, and washers should be assembled such that there is the same outer diameter of the locking configuration at the lateral and medial femoral epicondyles which warrants similar resistance against sinking into the bone (Fig 6).
The use of nuts and washers may be limited in patients where the nail is inserted deeply into the femoral canal or in small stature patient because of insufficient nut insertion depth resulting in premature contact of the nut with the nail (Fig 7). Furthermore, using nuts and washers in combination with the most proximal of the distal locking screws can result in unwanted hardware prominence which could lead to soft-tissue irritations.
There are two different instrumentation techniques to place the nut and washer:
- Nut-Over-Screw Technique: In this technique the locking screw is inserted first before the nut is placed over the screw tip at the opposite side. Tightening of the nut at the far cortex must be performed while applying counter-torque at the locking screw with the screwdriver at the near cortex.
- Nut-Over-Drill Bit Technique: In this technique the drill bit is kept in position after drilling. Subsequently, the nut is inserted over the drill bit tip until it is fully seated in the bone. After removal of the drill bit the locking screw is inserted through the nut. Tightening of the locking screw must be performed while applying counter-torque at the nut in the far cortex with the nut driver.
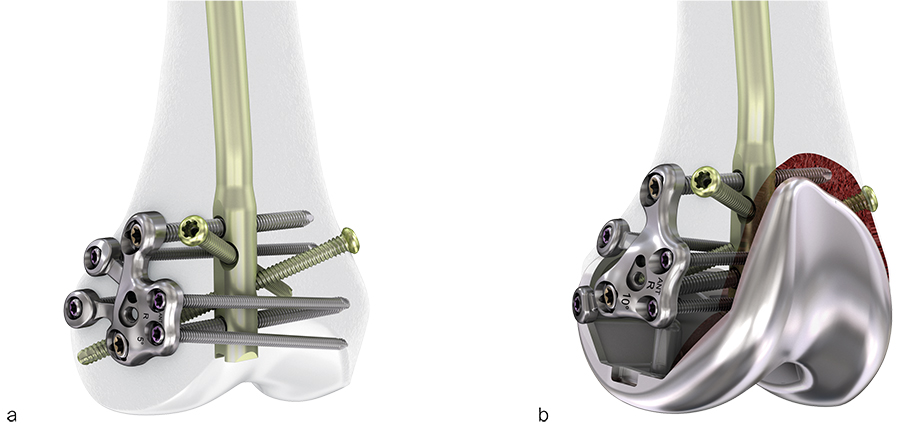
Enhanced fixation option 2: Locking Attachment Washer
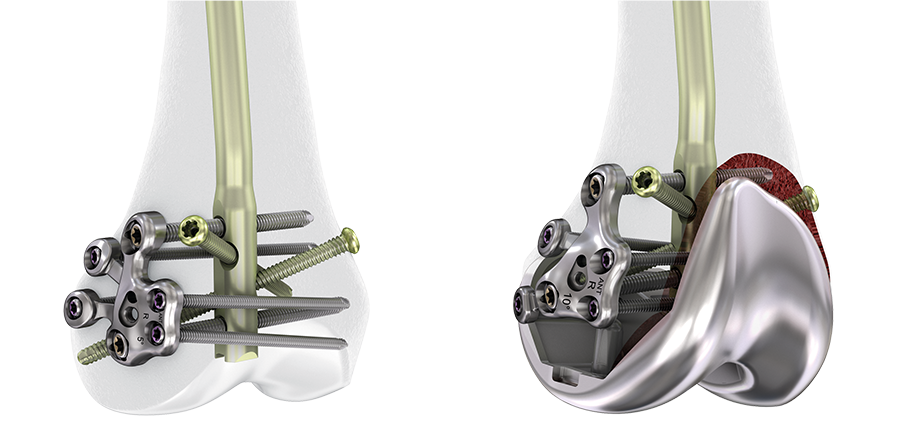
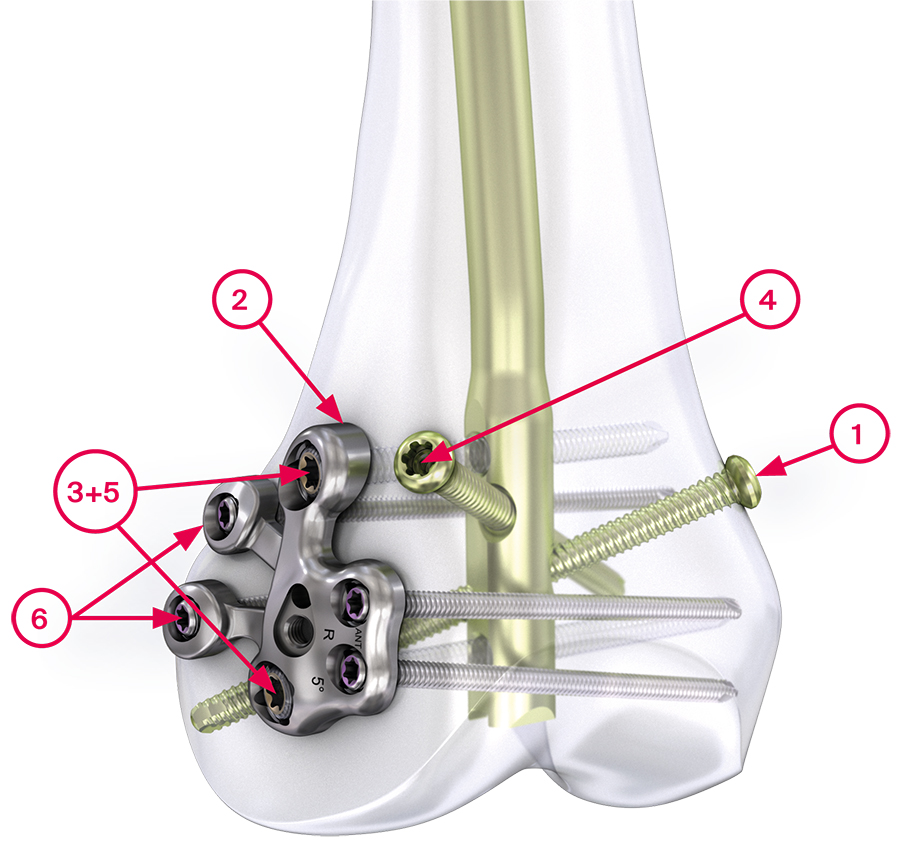
The Locking Attachment Washer (LAW) can be regarded as the most important innovation of the RFN-A System. This novel fixation option is expected to significantly improve retrograde nailing of native and periprosthetic distal femoral fractures by optimizing distal implant anchorage (Fig 8). The LAW concept allows to connect an anatomically shaped 6-hole plate (the locking attachment washer) at the lateral femoral epicondyle to the retrograde nail in an angular stable manner. This is accomplished by placing two 5 mm variable angle (VA) interlocking screws through the LAW and the two LM nail holes. In addition, four 3.5 mm VA screws can be inserted in the remaining LAW holes thereby enhancing nail anchorage in the distal femur.
Surgeons already use nail and plate combinations in clinical practice to improve distal femoral fracture fixation. However, current implants used for this so-called double fixation technique are not specifically designed for the purpose of connecting a plate and a nail. In this regard the LAW concept pioneers fracture fixation. It offers the advantages of nailing and plating in one fixation construct.
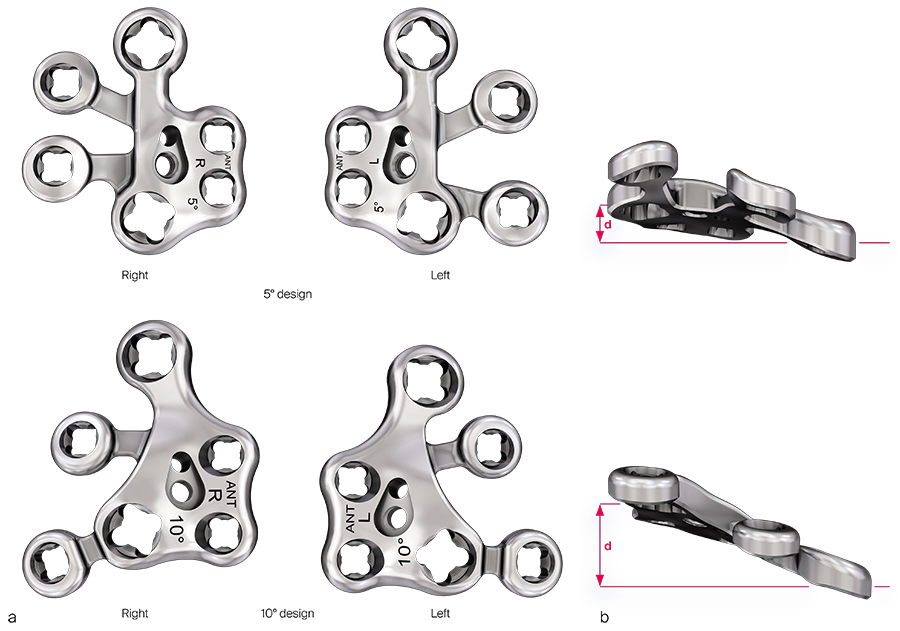
LAW design
The LAW is made of stainless steel. It is pre-contoured and offered in 5° and 10° design versions to closely match the anatomy of the lateral femoral epicondyle when paired with the retrograde nail of the corresponding bend (Fig 9). The LAW contains etch details to provide information on the LAW type, left- or right-side use as well as orientation. The positions of the posterior 3.5 mm VA locking screw holes are different between the left and right locking attachment washers because this accounts for the descending oblique screw trajectories when the universal RFN-A is used in the left or right femur. In certain patients, it might be preferred to pair the 5° LAW with the 10° bend nail to achieve better LAW fit. For the same reason, the 10° LAW might be used in combination with the 5° bend nail. The 10° LAW has a larger out-of-plane offset between the two 5.0 mm VA screw holes compared with the 5° LAW. This could be beneficial for the transition from the lateral femoral epicondyle if the proximal LM screw is located more superior due to patient anatomy, nail insertion depth, or the presence of a total knee arthroplasty femoral component (Fig 8). OPTILINK 5.0 mm VA Locking Screws are used to connect the stainless steel LAW to the titanium alloy nail. These stainless steel screws have undergone carburizing, a low temperature heat treatment in an environment enriched with carbon atoms to allow safe pairing with titanium implants.
The LAW increases the fixation density of the nail in the distal femur, which is especially useful to stabilize short distal bone segments.
Based on a compression test in a standardized distal femoral foam model the RFN-A with a fully instrumented LAW provided a 42% higher load to failure and a 30.5% higher axial stiffness than the RFN-A without LAW. In both constructs two distal nail interlocking screws were used to analyze the sole benefit of the LAW.
The improved nail anchorage distally contributes indirectly to the stability at the fracture site although the LAW does not bridge the fracture.
Indications
The RFN-A System is intended to stabilize fractures of the distal femur and the femoral shaft, including:
- Supracondylar fractures, including those with intraarticular extension
- Combination of ipsilateral condylar and diaphyseal fractures
- Ipsilateral femur/tibia fractures
- Femoral fractures in multiple trauma patients
- Periprosthetic fractures
- Fractures in the morbidly obese
- Fractures in osteoporotic bone
- Impending pathologic fractures
- Malunions and nonunions
Surgical technique for LAW placement
After nail insertion and attachment of the aiming arm to the nail insertion handle, the LAW is applied in following surgical steps:
Step 1: Secure the nail position with a screw or drill bit in the medial oblique locking hole.
Step 2: Place the LAW (with available handle). Once the LAW is properly oriented, hold it in position on the bone using the protection sleeves through the aiming arm.
Step 3: Partially insert the two 5.0 mm VA locking screws stopping approximately 1 cm short before full insertion.
Step 4: Insert the lateral oblique screw (optional).
Step 5: Adjust the LAW fit and hold it in place. Fully insert and lock the two 5.0 mm VA locking screws with 6 Nm.
Step 6: Contour the two posterior LAW holes with their tab features to the bone by using the bending drivers in situ. Insert the four 3.5 mm VA locking screws and lock them with 2.5 Nm.
RFN-A Instruments
The instrumentation of the RFN-A is supported by the same set of basic instruments that is also used for the other nails of the Advanced Nailing System. There is a QUICK CONNECT LATCH mechanism to ease the assembly of the aiming arm to the insertion handle (Fig 1). The TWIST & LOCK technology allows to secure the protection sleeves in the aiming arm with one quarter twist.
The surgical technique of implanting the RFN-A was optimized based on anatomy lab experiences and finally confirmed in validation labs by evaluating every surgical step of the procedure (Fig 2).
Innovations in retrograde femoral nailing: Retrograde Femoral Nail Advanced
Hazards and labeling
Due to varying countries’ legal and regulatory approval requirements, consult the appropriate local product labeling for approved intended use of the products described on this website. All devices on this website are approved by the AO Technical Commission. For logistical reasons, these devices may not be available in all countries worldwide at the date of publication.
Legal restrictions
This work was produced by AO Foundation, Switzerland. All rights reserved by AO Foundation. This publication, including all parts thereof, is legally protected by copyright.
Any use, exploitation or commercialization outside the narrow limits set forth by copyright legislation and the restrictions on use laid out below, without the publisher‘s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, scanning or duplication of any kind, translation, preparation of microfilms, electronic data processing, and storage such as making this publication available on Intranet or Internet.
Some of the products, names, instruments, treatments, logos, designs, etc referred to in this publication are also protected by patents, trademarks or by other intellectual property protection laws (eg, “AO” and the AO logo are subject to trademark applications/registrations) even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name, instrument, etc without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
Restrictions on use: The rightful owner of an authorized copy of this work may use it for educational and research purposes only. Single images or illustrations may be copied for research or educational purposes only. The images or illustrations may not be altered in any way and need to carry the following statement of origin “Copyright by AO Foundation, Switzerland”.
Check www.aofoundation.org/disclaimer for more information.
If you have any comments or questions on the articles or the new devices, please do not hesitate to contact us.
“approved by AO Technical Commission” and “approved by AO Foundation”
The brands and labels “approved by AO Technical Commission” and “approved by AO Foundation”, particularly "AO" and the AO logo, are AO Foundation's intellectual property and subject to trademark applications and registrations, respectively. The use of these brands and labels is regulated by licensing agreements between AO Foundation and the producers of innovation products obliged to use such labels to declare the products as AO Technical Commission or AO Foundation approved solutions. Any unauthorized or inadequate use of these trademarks may be subject to legal action.
AO ITC Innovations Magazine
Find all issues of the AO ITC Innovations Magazine for download here.
Innovation Awards
Recognizing outstanding achievements in development and fostering excellence in surgical innovation.